Reasons To Prevent Amputation
- Most-cost effective solution for patients (lower-limb amputations in diabetic patients comes with financial yearly costs of between $30,000 and $60,000
- Almost half the individuals who have an amputation because of vascular disease pass away within 5 years
- Having both legs amputated will have a negative impact on their life
- Lower limb amputation is associated with the loss of independence, depression, and a shortened lifespan
When Is Amputation Necessary
Not everyone with diabetes will need an amputation. If a person with diabetes does require this procedure, it is likely to be due to a wound or ulcer that did not heal on the foot or lower leg.
Most amputations are progressive, which means that a doctor will start by removing the smallest possible amount of tissue. If either the surgery wound does not heal or blood flow does not go to the limb properly, they may recommend further surgery to remove more tissue.
Peripheral Artery Disease Symptoms
Peripheral artery disease symptoms include:
- Intermittent claudication
In the most severe case, as mentioned above, due to a combination of decreased sensation and reduced blood flow to the feet, ulcers may develop. If the tissues continue to receive insufficient oxygen, tissue death occurs. Gangrene is a serious and potentially life-threatening condition. Other potentially serious problems that may develop include cellulitis and osteomyelitis ; also is possible.
People with diabetes are at increased risk for milder problems with the feet that are not specific to diabetes but may occur more frequently due to problems with the nerves and circulation to the feet.
Some of these conditions are:
- and corns, that may develop due to abnormal alignment of the feet or abnormal gait
- Fungal infections of the nails, which can appear as thickened, discolored, and at times brittle nails
- Tinea pedis, or athlete’s foot, a fungal infection of the skin of the feet
- Hammertoes, or bent toes due to muscle weakness.
- Bunions, or the angling of the big toe toward the second toe. The area of the bunion may become reddened and irritated, leading to formation.
Other types of foot problems can be relieved by proper footwear, sometimes with orthotic devices, and splinting or bracing. For some conditions like hammertoes, bunions, and ingrown toenails; surgery may be necessary to correct severe cases.
You May Like: Where Are Insulin And Glucagon Produced
When To See Your Doctor Or Podiatrist
- Any breaks in the skin need to be treated straight away, so see your doctor or podiatrist. Also, try to work out what might have caused the problem so that you can prevent it happening again.
- If one of your feet is hot and swollen, check it again the next day â see your doctor if it remains hot and swollen. Antibiotics may be needed to treat an infection.
- Toenail infections should be treated promptly.
- Let your doctor know if you develop pain in the feet and legs or notice changes in the colour or temperature of your feet and legs.
Your feet should also be examined regularly by a doctor, diabetes specialist or podiatrist. Your doctor or podiatrist can advise you on foot care and also on the selection of appropriate footwear.
How Can Diabetes Affect My Feet

Over time, diabetes may cause nerve damage, also called diabetic neuropathy, that can cause tingling and pain, and can make you lose feeling in your feet. When you lose feeling in your feet, you may not feel a pebble inside your sock or a blister on your foot, which can lead to cuts and sores. Cuts and sores can become infected.
Diabetes also can lower the amount of blood flow in your feet. Not having enough blood flowing to your legs and feet can make it hard for a sore or an infection to heal. Sometimes, a bad infection never heals. The infection might lead to gangrene.
Gangrene and foot ulcers that do not get better with treatment can lead to an amputation of your toe, foot, or part of your leg.A surgeon may perform an amputation to prevent a bad infection from spreading to the rest of your body, and to save your life. Good foot care is very important to prevent serious infections and gangrene.
Although rare, nerve damage from diabetes can lead to changes in the shape of your feet, such as Charcots foot. Charcots foot may start with redness, warmth, and swelling. Later, bones in your feet and toes can shift or break, which can cause your feet to have an odd shape, such as a rocker bottom.
You May Like: Does Drinking Water Lower Blood Sugar
Ask About Amputation Prevention
If you have diabetes then dont take your limbs for granted. Amputation prevention is about taking early and aggressive steps to heal and preserve your lower legs, feet, and toes. The program commences with vascular screening to assess your risk and diagnose PAD in its earliest stage.
At MINT, Dr. Goke Akiinwande is a specialist in opening arteries and veins and proud to operate a dedicated amputation prevention center. To schedule a FREE vascular screening call one of our offices in Creve Coeur, Farmington, or St. Louis, Missouri, or use online booking today.
- 4.94/5
Understanding The Connection Between Diabetes And Amputation
Amputation because of diabetes is more common than many people realize. which beggars the question why is it that diabetics lose limbs?
According to the WHO , lower limb amputations are 10 times more likely in people who have diabetes than in people who do not have diabetes.
With almost 60% of amputations caused by common complications of diabetes and peripheral disease, its vital to address the connection between the two so that patients can seek help and save their limbs before its too late.
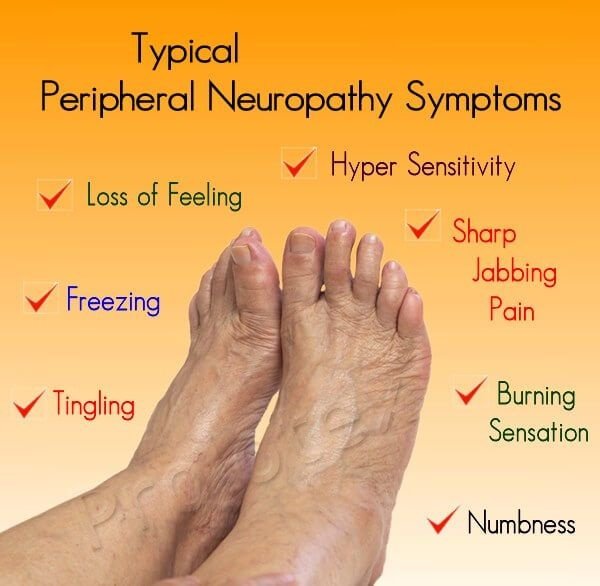
A major problem for people with diabetes is peripheral neuropathy which is essentially a loss of feeling or sensation in the feet and legs. When this occurs, theyre less likely to notice mild leg or foot ulcers before they become more severe.
In other words, many diabetics require amputation because they simply cant feel the open diabetic sores on their feet and legs until they are at a higher risk of amputation and approaching a point of no return.
However, with more effective foot care and patient strategies implemented, theres absolutely no reason why many of these high-risk patients cant be healed.
You May Like: How Is Insulin Related To The Digestive System
Treatment For Loss Of Sensation In Feet Due To Diabetes
If you are diabetic and have loss of feeling in your feet, the first thing that you have to do is to consult your health care practitioner. Treatment for each patient may vary; the primary aim of any treatment for diabetic peripheral neuropathy is to bring blood sugar level under control.
- Your doctor may recommend measures to control blood glucose level. You should avoid eating food products that contain sugar. Exercise regularly; eat vegetables and cereals and fruits. Avoid bread and other products made from white flour.
- Take anti diabetic medicines regularly.
- The health care practitioner may also recommend multivitamin supplements.
- You may also be recommended to take certain medicines that will help to reduce symptoms accompanied with nerve damage.
- Alternative therapies such as acupressure and electrotherapy are also beneficial to reduce symptoms.
Statistics Related To Diabetes And Amputations
Over half of limb amputations in the United States are attributable to diabetes and related complications. The majority of limb amputations are performed on the lower extremities.
From 1980 to 2003, lower extremity amputations increased from 33,000 to 84,000 in 1997, and dropped back down to 75,000 amputations in 2003. In 2010, about 73,000 lower-limb amputations were performed in adults aged 20 years or older with diagnosed diabetes. As is easily seen, amputations are still a big problem for those with diabetes.1
I advise reading the following articles:
Diabetic neuropathy and subsequent damage to sensory nerves in the feet contribute greatly to deformities and ulcers, thereby increasing the risk for amputations if left untreated. For those under the age of 65, 3.9 of 1000 people with diabetes had an amputation. From age 65 to age 74, the incidence increased to 6.6 per 1000. For those over the age of 75, amputation occurred at a rate of 7.9 per 1000.
Rates were 50 percent higher for men than women. The elderly have more amputations, as do the non-Hispanic black population. The rate for amputations for people with diabetes is 28 times higher than for people without diabetes.
These statistics are alarming when compared with the CDC estimate that 23.6 million Americans currently have diabetes, a number that is up from 18.2 million in 2003. No wonder a cornerstone of diabetes self-management and education is foot care.
Read Also: Do You Give Insulin Or Dextrose First For Hyperkalemia
Diabetes Comprehensive Foot Exam
A comprehensive foot exam is done yearly, and includes assessment of present diabetes complications, such as neuropathy, nephropathy, retinopathy, peripheral vascular disease, and cardiovascular disease. Notes are made related to any prior amputations, history of an ulcer, or presence of a current ulcer. The examiner will assess for calf pain, changes in the feet since the last evaluation, and any problem with shoes.
The exam includes assessment of smoking status, A1C level, skin, and hair and nail condition. The examiner will look for thin, fragile, shiny and hairless skin when evaluating for circulation problems. Thickened, discolored, ingrown or infected toenails may signal a fungal infection.
The examiner will measure and draw the patients skin condition into a diagram, using a key to mark where pre-ulcers, ulcers, calluses, or bunions are, to name a few. They will note toe and foot deformities, including Charcots foot, and prominent metatarsal heads . They will also look for foot drop, and check for pulses in the feet, .
The examiner also assesses for the appropriate footwear that is fit properly. At this point, the examiner can order therapeutic shoes or foot inserts if necessary. If shoes or foot inserts are ordered, they are often covered by insurance, and it is best to get them at the podiatrist or orthoptist, as opposed to at the shoe store.
The examination can be performed by a Certified Diabetes Educator, a podiatrist, or an RN foot specialist, to name a few.
Diabetes: Protect Your Feet And Legs
Foot and leg problems are common diabetes complications, but proper precautions can prevent up to half of all diabetes-related amputations.
If you have diabetes, you are more likely than people without this disorder;to develop leg and foot problems. Diabetes can destroy nerves and cause you to have poor circulation. Left unchecked, these complications can lead to amputation. But there’s a lot you can do to prevent that from happening.
Also Check: Is 10 Units Of Insulin A Lot
Treating Diabetic Neuropathy And Poor Circulation
Specific treatment of conditions that can affect the legs and feet in people with diabetes â diabetic neuropathy and poor circulation in the legs and feet â is necessary.
Tight control of the amount of glucose in the bloodstream has been shown to reduce the risk of neuropathy, slow its progress and help improve symptoms.
Reducing other risk factors for diabetic neuropathy and poor circulation to the legs and feet can also help. These include:
- not smoking;
- losing weight if overweight.
What Is Diabetic Neuropathy
Up to 70%;of people with diabetes develop diabetic neuropathy, a condition of nerve damage that significantly increases the risk of amputation in the future. This occurs so frequently because high blood sugar levels damage the protective covering on the nerves and the blood vessels that deliver oxygen to nerves. Eventually, the damage becomes so extensive that nerves cant efficiently send signals around the body.
Diabetic neuropathy is easiest to recognize by the;numbness and tingling;it causes in the hands and feet, but it also presents itself through other symptoms:
- Shooting or burning pains
- Dizziness, especially when standing up or walking
- Sensation of wearing an invisible sock or glove
- Difficulty sleeping because of feet and leg pain
- Loss of coordination and difficulty walking or moving the arms
This is known as;peripheral neuropathy;since it begins in the toes and fingers and moves up and inward along the body. You might experience constant or sporadic pain that develops suddenly or gradually over many years. Regardless, the signs of neuropathy indicate that youre at risk of diabetic wounds that, if left untreated, often require amputation.
Recommended Reading: How Many Carbs Should A Diabetic Have In One Day
S To Prevent Amputation
Fortunately, the National Institute of Diabetes and Digestive and Kidney Diseases reports that as many as half of all amputations related to these foot and leg complications can be prevented if the problems are caught early.
Many measures can significantly reduce the risk of ulcer formation, including having properly fitted shoes, doing routine foot checks, not walking barefoot, and stopping smoking, says Tan. Properly fitted shoes and moisture-absorbing socks are important to prevent foot injury, particularly with diabetic;neuropathy;when one may not feel or notice an injury.
Here is a list of the most important things you can do to avoid amputation.
1. Quit smoking. The American Diabetes Association points out that if you’re a smoker, quitting is the first and best way to prevent an amputation. Smoking decreases the blood flow in the small blood vessels of your legs and feet, making it difficult for wounds to heal.
Having diabetes and smoking creates an especially high-risk scenario for amputation, says Matt Petersen, the managing director of medical information and professional engagement at the American Diabetes Association. In addition to careful management of diabetes with the support of a healthcare provider, smoking cessation is the most direct way to decrease the risk of amputation.
4. Be sure your doctor examines your feet at least once a year or whenever you notice a problem.
6. Don’t use alcohol, hydrogen peroxide, astringent, or iodine on your feet.
Keep The Blood Flowing To Your Feet
Try the following tips to improve blood flow to your feet:
- Put your feet up when you are sitting.
- Wiggle your toes for a few minutes throughout the day. Move your ankles up and down and in and out to help blood flow in your feet and legs.
- Do not wear tight socks or elastic stockings. Do not try to hold up loose socks with rubber bands.
- Be more physically active. Choose activities that are easy on your feet, such as walking, dancing, yoga or stretching, swimming, or bike riding.
- Stop smoking.
Smoking can lower the amount of blood flow to your feet. If you smoke, ask for help to stop. You can get help by calling the national quitline at 1-800-QUITNOW or 1-800-784-8669. For tips on quitting, go to SmokeFree.gov.
Recommended Reading: How To Instantly Lower Blood Sugar
What Are Major And Minor Amputations
Amputations in general, not just diabetes-related amputations, are classed as major and minor.
- Minor amputation regards removal of toes or feet
- Major amputation refers to the above or below the knee amputation.
One of the horror stories that go round is that people with diabetes are doomed to suffering amputations. Whilst it is true that people with diabetes have a higher statistical risk of amputation, it is largely a preventable fate.
Approximately 6,000 amputations are carried out each year for people with diabetes. Diabetes UK reports that, of these, around 80% are believed to be preventable. The NHS advises that amputation is commonly needed if damage occurs to the foot and gangrene sets in.
Damage to the foot could include any of the following:
- Cuts
Peripheral Neuropathy And Diabetes
Diabetic foot pain is mainly due to a condition called peripheral neuropathy. Approximately 50% of people who have type 2 diabetes will develop peripheral neuropathy, which happens when high blood sugar levels cause damage to the nerves in the legs and the feet.
If you are frequently feeling foot pain, your type of neuropathy may be sensory, where even the slightest touch can cause overwhelming pain. The reaction is not proportional to the stimulus, because the nerves are overly sensitive.
Another type of peripheral neuropathy is motor neuropathy, wherein the nerves that connect to the muscles are weakened and therefore hurt. As a result, it may be a challenge to balance yourself with weakened legs and feet. This imbalance may lead to the development of corns, calluses, cuts, scrapes, and swelling.
For diabetics with motor neuropathy, customized orthotics may help address the balance issues and prevent the development of other foot issues. Its important that you keep your muscles in use so that your legs and feet stay strong.
Recommended Reading: Can You Lose Weight With Diabetes
Check Your Feet Every Day
You may have foot problems, but feel no pain in your feet. Checking your feet each day will help you spot problems early before they get worse. A good way to remember is to check your feet each evening when you take off your shoes. Also check between your toes. If you have trouble bending over to see your feet, try using a mirror to see them, or ask someone else to look at your feet.
Look for problems such as
- cuts, sores, or red spots
- swelling or fluid-filled blisters
- ingrown toenails, in which the edge of your nail grows into your skin
- corns or calluses, which are spots of rough skin caused by too much rubbing or pressure on the same spot
- plantar warts, which are flesh-colored growths on the bottom of the feet
- athletes foot
- warm spots
If you have certain foot problems that make it more likely you will develop a sore on your foot, your doctor may recommend taking the temperature of the skin on different parts of your feet. A hot spot can be the first sign that a blister or an ulcer is starting.
Cover a blister, cut, or sore with a bandage. Smooth corns and calluses as explained below.

