Structure And Synthesis Of Glucagon
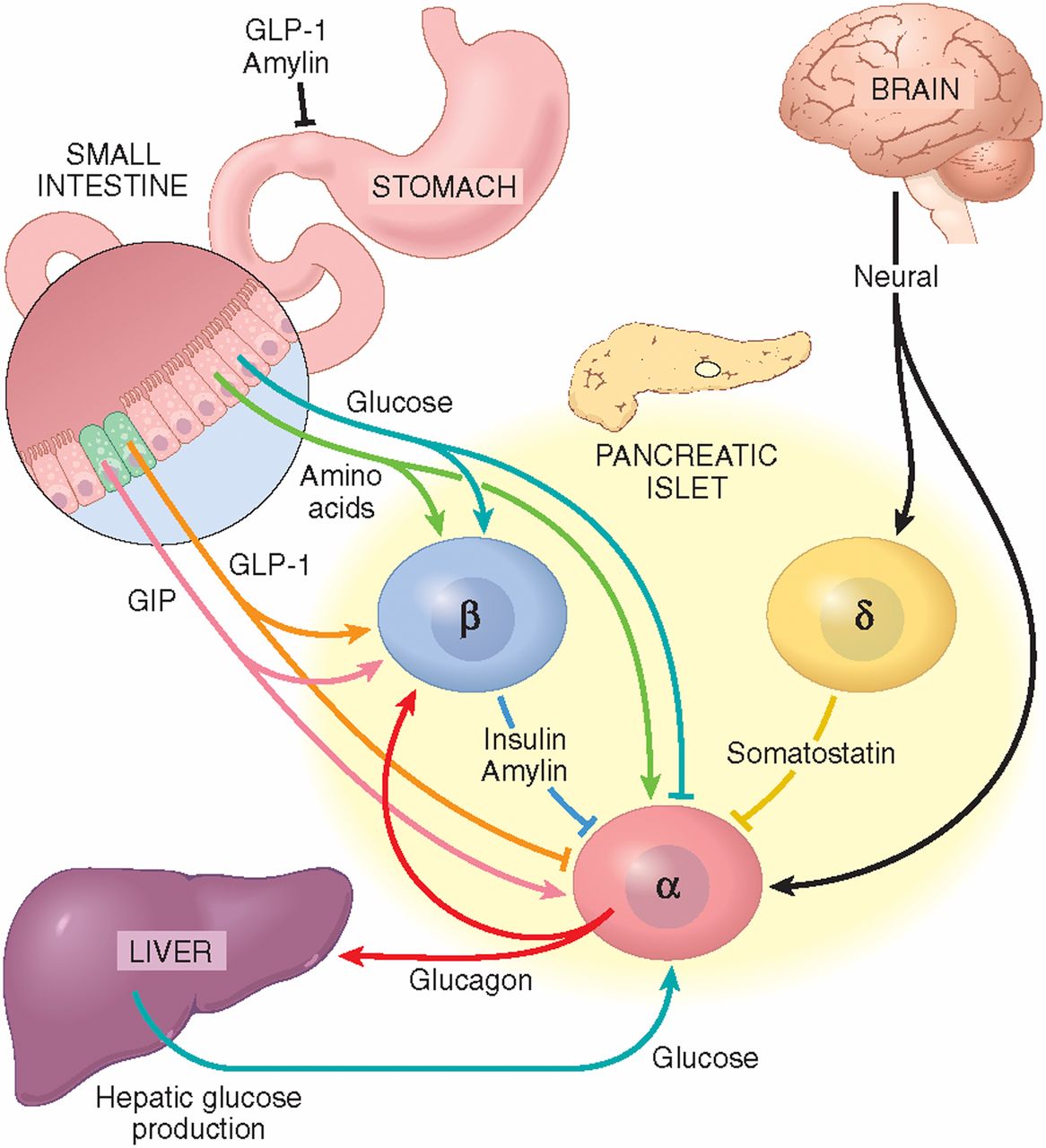
Glucagon is a 29-amino acid peptide hormone predominantly secreted from the alpha cells of the pancreas. It is derived from the precursor proglucagon which can be processed into a number of related peptide hormones . Proglucagon is expressed in pancreatic islet alpha cells, intestinal enteroendocrine L cells, and to a minor extent in neurons in the brain stem and hypothalamus . Processing of proglucagon is undertaken by the processing enzymes prohormone convertase 1/3 and prohormone convertase 2 , respectively. In the pancreas, PC2 processes proglucagon to glucagon while processing of proglucagon in the intestine and the brain is undertaken by PC1 leading to the formation of glucagon-like peptide 1 and glucagon-like peptide 2 .
Regulation Of Glucagon Production
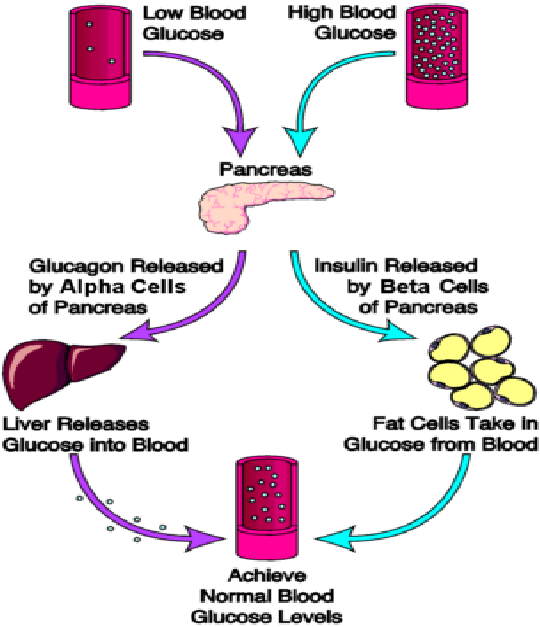
- Glucagon levels are increased in response to hypoglycemia or low blood sugar.
- Consumption of a protein rich meal which leads to elevation of amino acid levels triggers glucagon release.Glucagon converts amino acids into glucose by gluconeogenesis.
- Exercise also triggers glucagon release. It enhances the rates of glycogenolysis and gluconeogenesis to provide the body with energy during exercise.
- An increase in glucagon secretion has been reported under conditions of acute stress. This occurs in response to the stimulation of adrenergic receptors in the pancreatic cells.
- Glucagon secretion is increased during cold acclimatization. Glucagon is thermogenic and increases energy consumption in the body.
- Glucagon secretion is also increased by cortisol , acetylcholine , theophylline, infections etc.
- High glucose levels, or hyperglycemia, inhibit glucagon production by the alpha cells of islets of Langerhans.
- Somatostatin is also known as the growth inhibiting hormone. Apart from the hypothalamus, it is also produced by the alpha cells of the pancreas. Somatostatin produced by the alpha cells of the pancreas inhibits the production of glucagon in these cells.
- Glucagon secretion is also inhibited by free fatty acids , ketones, insulin, GABA etc.
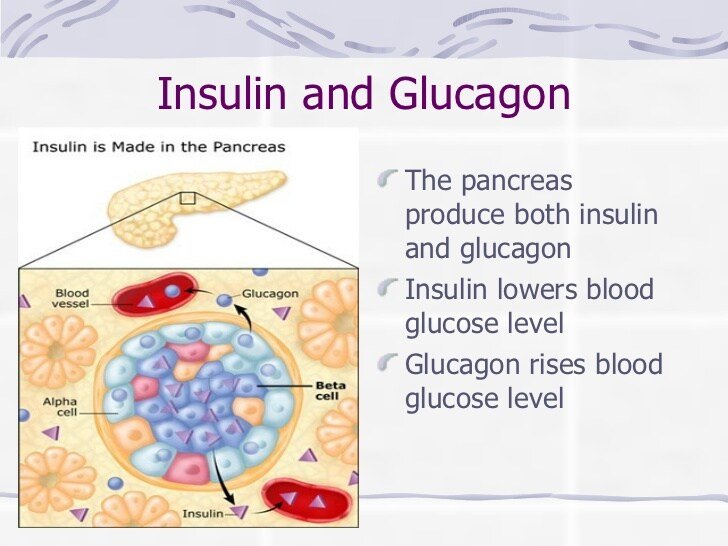
What Hormones Does The Pancreas Produce
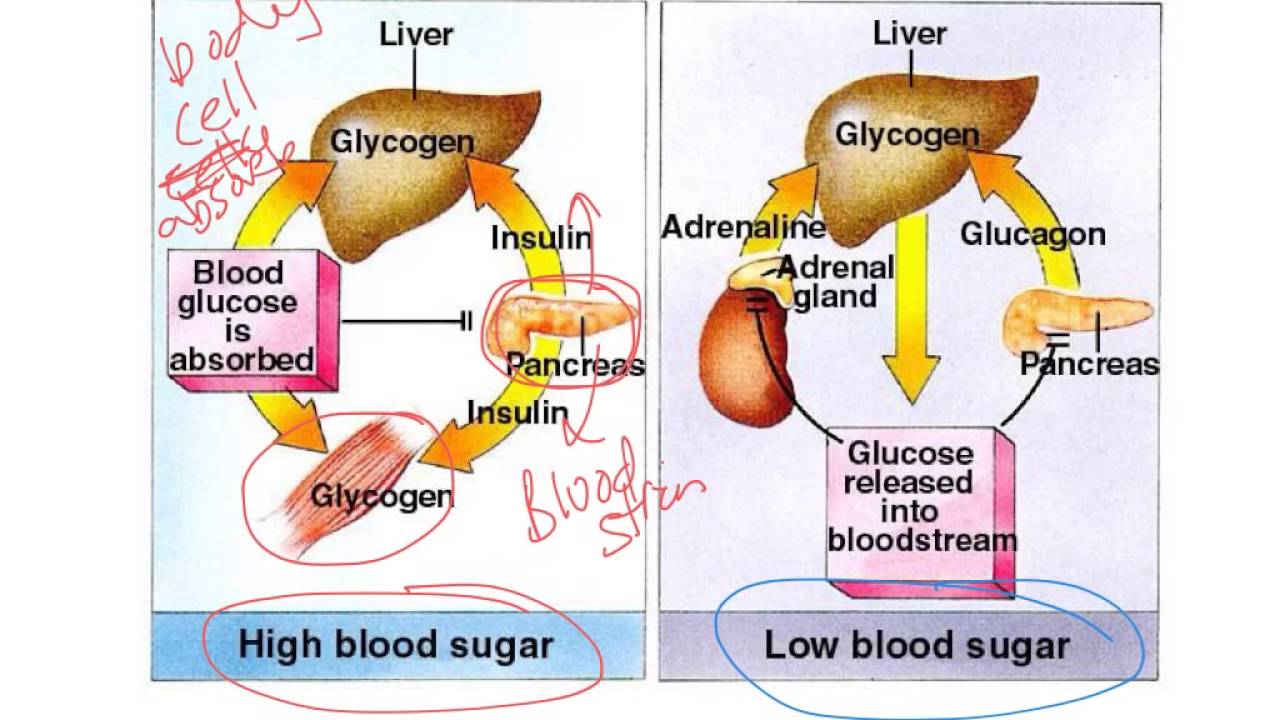
The most important hormone that the pancreas produces is insulin. Insulin is released by the ‘beta cells’ in the islets of Langerhans in response to food. Its role is to lower glucose levels in the bloodstream and promote the storage of glucose in fat, muscle, liver and other body tissues.
‘Alpha cells‘ in the islets of Langerhans produce another important hormone, glucagon. This has the opposite effect to insulin, by helping release energy into the bloodstream from where it is stored, thus raising blood sugar levels. Therefore, glucagon and insulin work in tandem to control the balance of glucose in the bloodstream.
Other hormones produced by the pancreas include pancreatic polypeptide and somatostatin. They are believed to play a part in regulating and fine-tuning the insulin and glucagon-producing cells.
What To Do For Severe Low Blood Sugar
The Role Of Glucagon In Blood Glucose Control
The effect of glucagon is to make the liver release the glucose it has stored in its cells into the bloodstream, with the net effect of increasing blood glucose. Glucagon also induces the liver to make glucose out of building blocks obtained from other nutrients found in the body .
Our bodies desire blood glucose to be maintained between 70 mg/dl and 110 mg/dl . Below 70 is termed “hypoglycemia.” Above 110 can be normal if you have eaten within 2 to 3 hours. That is why your doctor wants to measure your blood glucose while you are fasting…it should be between 70 and 110. Even after you have eaten, however, your glucose should be below 180. Above 180 is termed “hyperglycemia” . If your 2 two blood sugar measurements above 200 after drinking a sugar-water drink , then you are diagnosed with diabetes.
Ok But What Do They Have To Do With Each Other
Now you know insulin and glucagon have pretty similar jobs. But how do these hormones work together?
When theyre doing their jobs correctly, they work in perfect balance: Insulin prevents glucose levels from getting too high while glucagon prevents them from getting too low.
Both need to be effective for your blood sugar levels to stay, well, as close to perfect as possible.
When insulin and glucagon arent working correctly, things get complicated. If one or the other isnt properly regulating glucose levels, those levels will get thrown off, which can have some pretty serious side effects.
Glucagon Increases Energy Expenditure
In addition to a potential effect of glucagon on food intake, evidence suggests that glucagon contributes to a negative energy balance by stimulating energy expenditure. In humans, this effect has been observed in studies in which glucagon infusion resulted in increases in resting energy expenditure . However, the effect of endogenous glucagon on resting energy expenditure remains unclear. Also, the exact mechanisms behind the increase in resting energy expenditure elicited by exogenous glucagon remain to be determined. It has been speculated that glucagon activates brown adipose tissue , however this was recently challenged in an in vivo study that found no direct effect of glucagon on brown adipose tissue . Rodent studies indicate that the actions of glucagon to increase energy expenditure might be indirectly mediated partly by fibroblast growth factor 21 as glucagon-induced increase in energy expenditure is abolished in animals with FGF21 receptor deletion .
Glucagon In Obesity And Hepatic Steatosis
Dysregulated glucagon secretion is not only observed in patients with type 2 diabetes but also in normoglucose-tolerant individuals with obesity and patients with non-alcoholic fatty liver disease . This suggests that dysregulated glucagon secretion may represent hepatic steatosis rather than dysregulated glucose metabolism. Interestingly, fasting hyperglucagonemia seems to relate to circulating amino acids in addition to hepatic fat content . This hyperaminoacidemia suggests that impairment of amino acid turnover in the liver and ensuing elevations of circulating amino acids constitutes a feedback on the alpha cell to secrete more glucagon with increasing hepatic amino acid turnover and ureagenesis needed for clearance of toxic ammonia from the body. This feedback loop is proposed as the liver-alpha cell axis .
Glucagon: What It Is And How To Use It
Glucagon is a hormone that raises a persons blood sugar . Like insulin, glucagon is produced in the pancreas. In a person without type 1 diabetes, the pancreas releases glucagon to ensure blood sugar does not drop too low.
When a person has type 1 diabetes, this doesnt happen. People with type 1 diabetes must check their blood sugar regularly, try to prevent low blood sugar, and treat it as soon as it happens with a source of fast-acting sugar .
If a persons blood sugar drops so low that they are unable to treat it themselves, they are having a severe low blood sugar . Other symptoms include:
- Being unresponsive or unconscious
- Being so uncooperative that you cant give juice or sugar by mouth
Note:
Severe low blood sugar is an emergency. You must act immediately. Do not leave the student alone.
Carefully following a students Individual Care Plan should help to prevent a severe low blood sugar from happening at school. But its important to know what to do in case of emergency.
Mechanism Of Hormone Action
The hormone when entered into the bloodstream can reach almost all the organs of the body. But as we read above, hormones are very specific in nature, so they only act on specific target organs for which they were released into the bloodstream. Two types of hormones are present that are lipid-soluble and lipid-insoluble. Testosterone and estrogen are lipid-soluble hormones whereas insulin and glucagon are lipids insoluble. As the plasma membrane of the cells is made up of lipid bilayer so the lipid-soluble hormones can easily pass through it whereas lipid insoluble hormones are not able to cross the plasma membrane. There are certain receptors that are known as hormone receptors that are present on the target organs. The hormones are able to produce their effect when they bind with the hormone receptors. They are also known as membrane-bound receptors as they are present on the cell membrane of the cell. A hormone-receptor complex is formed when the hormone binds to the receptor. These receptors are specific to one hormone and that is the reason behind the specificity of hormones. The metabolism of the target tissue and all the physiological functions are regulated by the hormones.
The Important Roles Of Insulin And Glucagon: Diabetes And Hypoglycemia
The human body wants blood glucose maintained in a very narrow range. Insulin and glucagon are the hormones which make this happen. Both insulin and glucagon are secreted from the pancreas, and thus are referred to as pancreatic endocrine hormones. The picture on the left shows the intimate relationship both insulin and glucagon have to each other. Note that the pancreas serves as the central player in this scheme. It is the production of insulin and glucagon by the pancreas which ultimately determines if a patient has diabetes, hypoglycemia, or some other sugar problem.
Where Are Insulin And Glucagon Produced
4.4/5hormonescellspancreasbloodcellspancreas
pancreas
Also, how do insulin and glucagon work together? Insulin and glucagon are hormones that help regulate the levels of blood glucose, or sugar, in your body. Insulin and glucagon work together to balance your blood sugar levels, keeping them in the narrow range that your body requires. These hormones are like the yin and yang of blood glucose maintenance.
People also ask, where is glucagon produced?
pancreas
How is glucagon released?
Glucagon is a peptide hormone, produced by alpha cells of the pancreas. The pancreas releases glucagon when the concentration of insulin in the bloodstream falls too low. Glucagon causes the liver to convert stored glycogen into glucose, which is released into the bloodstream.
What Happens If I Have Too Little Glucagon
Unusual cases of deficiency of glucagon secretion have been reported in babies. This results in severely low blood glucose which cannot be controlled without administering glucagon.
Glucagon can be given by injection to restore blood glucose lowered by insulin . It can increase glucose release from glycogen stores more than insulin can suppress it. The effect of glucagon is limited, so it is very important to eat a carbohydrate meal once the person has recovered enough to eat safely.
Medications Which Affect Glucagon Secretion
A number of medications have been developed to help modify the release of glucagon in type 2 diabetes.
Two different classes of diabetes drugs , DPP-4 inhibitors and incretin mimetics, act in response to the presence of meals to stimulate the increase of insulin and to inhibit the release of glucagon.
Got It Whats Glucagon
Glucagon is similar to insulin: Its another hormone your pancreas releases that controls the levels of glucose in your blood.
Glucagon works with your liver to prevent your blood sugar level from dropping too low. It also helps convert glycogen into glucose and releases it into your blood so your body can use it for energy.
Ever the multitasker, glucagon also works to keep your liver from consuming too much glucose in order to keep your blood sugar stable throughout your body.
Main Difference Insulin Vs Glucagon
Insulin and glucagon are two types of hormones responsible for the maintenance of glucose levels in the blood. Glucose is one of the vital sources of energy. It circulates through blood and is taken up by the metabolizing cells of the body. Both enzymes are secreted by the pancreas. The main difference between insulin and glucagon is that insulin increases the glucose uptake by the body cells from the blood whereas glucagon releases glucose from the liver and muscle cells into the blood. This means insulin decreases the blood glucose levels while glucagon increases the blood glucose level.
Molecular Structure Of Of Insulin:
Insulin is made of amino acids and consists of two chains named an A chain and a B chain, that are joined together by sulfur bonds. Insulin is produced from a proinsulin hormone that actually has three amino acid chains. An enzyme modifies the hormone in such a way that only the A and B chain remains to form insulin.
Glucagon And Blood Glucose Levels
Glucagon serves to keep blood glucose levels high enough for the body to function well.
When blood glucose levels are low, glucagon is released and signals the liver to release glucose into the blood.
Glucagon secretion in response to meals varies depending on what we eat:
- In response to a carbohydrate based meal, glucagon levels in the blood fall to prevent blood glucose rising too high.
- In response to a high protein meal, glucagon levels in the blood rise.
Glucagon Increases Hepatic Glucose Production
Glucagon controls plasma glucose concentrations during fasting, exercise and hypoglycemia by increasing hepatic glucose output to the circulation. Specifically, glucagon promotes hepatic conversion of glycogen to glucose , stimulates de novo glucose synthesis , and inhibits glucose breakdown and glycogen formation . Hepatic glucose production is rapidly enhanced in response to a physiological rise in glucagon; achieved through stimulation of glycogenolysis with minor acute changes in gluconeogenesis . This ability of glucagon is critical in the life-saving counterregulatory response to severe hypoglycemia. Additionally, it is a key factor in providing adequate circulating glucose for brain function and for working muscle during exercise . During prolonged fasting, glycogen stores are depleted, and gluconeogenesis takes over . The hyperglycemic property of glucagon is enhanced when hepatic glycogen levels are high and diminished when hepatic glycogen levels are low in conditions of fasting or liver diseases like cirrhosis .
Interaction Of Hormone With Membrane Receptors
Some hormones do not enter the target organ and they just interact with the membrane-bound receptors. The protein and peptide hormones usually function in such a way. They are able to produce secondary messengers. These hormones come in contact with the external domain that is present on the extracellular surface of the cell. A hormone-receptor complex is formed when this hormone binds to the receptor. This brings about some conformational changes in the cytoplasmic part of the receptor. This in turn helps to produce secondary messengers. The secondary messengers can be calcium ions, cyclic AMP, etc. These messengers help in activating the enzyme receptors and then the whole enzyme system. When this system is activated when there is an acceleration of the biochemical reactions of the cell. The hormone that binds to the receptor is known as the primary messenger and the secondary messengers are the calcium ions and cyclic AMPs that are produced afterwards. Growth hormone receptors and steroid hormone receptors also function the same way.
Ideal Blood Sugar Levels
A range of factors, including insulin resistance, diabetes, and an unbalanced diet, can cause blood sugar levels to spike or plummet.
The standard measurement units for blood sugar levels are milligrams per deciliter . Ideal blood sugar ranges are as follows:
| Timing |
Insulin and glucagon do not take immediate effect, particularly in people whose blood sugar levels are extremely high or low.
Glucagon In Type 2 Diabetes
Patients with type 2 diabetes exhibit an impaired regulation of glucagon secretion which contributes importantly to diabetic hyperglycemia. Specifically, type 2 diabetes is characterized by elevated levels of glucagon during fasting while suppression of glucagon in response to oral intake of glucose is impaired or even paradoxically elevated . The mechanisms behind hyperglucagonemia are not fully understood but is usually explained by a diminished suppressive effect of insulin on alpha cells due to hypoinsulinemia and insulin resistance at the level of the alpha cells . Interestingly, subjects with type 2 diabetes, who exhibit a hyperglucagonemic response to oral glucose, respond with a normal suppression of glucagon after intravenous glucose administration . This suggests that diabetic hyperglucagonemia may not be explained by alpha cell resistance to glucose and/or insulin. Accordingly, hormones secreted from the gastrointestinal tract may play an important role . It has recently been confirmed that glucagon can be secreted from extrapancreatic tissue . This supports the notion that postprandial hypersecretion of glucagon in patients with type 2 diabetes might be of extrapancreatic origin.
How Is Glucagon Controlled
Glucagon works along with the hormone insulin to control blood sugar levels and keep them within set levels. Glucagon is released to stop blood sugar levels dropping too low , while insulin is released to stop blood sugar levels rising too high .
The release of glucagon is stimulated by low blood glucose, protein-rich meals and adrenaline . The release of glucagon is prevented by raised blood glucose and carbohydrate in meals, detected by cells in the pancreas.
In the longer-term, glucagon is crucial to the bodys response to lack of food. For example, it encourages the use of stored fat for energy in order to preserve the limited supply of glucose.
Understanding The Processes Behind The Regulation Of Blood Glucose
20 April, 2004
VOL: 100, ISSUE: 16, PAGE NO: 56
Pat James, PhD, is senior lecturer in applied physiology
Roger McFadden, MSc, is senior lecturer in applied physiology; both at the School of Health and Policy Studies, The University of Central England in Birmingham
Pat James, PhD, is senior lecturer in applied physiology
Glucose is one of the bodys principal fuels. It is an energy-rich monosaccharide sugar that is broken down in our cells to produce adenosine triphosphate. ATP is a small packet of chemical energy that powers the millions of biochemical reactions that take place in the body every second.
We obtain glucose from the food that we eat, predominantly starch-rich foods such as potatoes, rice, bread, and pasta. Starch is a polysaccharide that is broken down by digestive enzymes into individual glucose molecules.
In the small intestine, glucose is absorbed into the blood and travels to the liver via the hepatic portal vein. The hepatocytes absorb much of the glucose and convert it into glycogen, an insoluble polymer of glucose.
This is stored in the liver and can be reconverted into glucose when blood-glucose levels fall. Other types of simple sugars in our diet such as fructose, sucrose and lactose are also fuels that contribute to the production of ATP.
If glucose levels fall to too low a concentration or rise too high then this situation can lead to the neurological processes in the brain being compromised.
Regulation Of Blood Glucose
Regulation of glucose in the body is done autonomically and constantly throughout each minute of the day. Normal BG levels should be between 60 and 140 mg/dL in order to supply cells of the body with its required energy. Brain cells dont require insulin to drive glucose into neurons; however, there must still be normal amounts available. Too little glucose, called hypoglycemia, starves cells, and too much glucose creates a sticky, paralyzing effect on cells. Euglycemia, or blood sugar within the normal range, is naturally ideal for the bodys functions. A delicate balance between hormones of the pancreas, intestines, brain, and even adrenals is required to maintain normal BG levels.
Cells And Secretions Of The Pancreatic Islets
The pancreatic islets each contain four varieties of cells:
- The alpha cell produces the hormone glucagon and makes up approximately 20 percent of each islet. Glucagon plays an important role in blood glucose regulation; low blood glucose levels stimulate its release.
- The beta cell produces the hormone insulin and makes up approximately 75 percent of each islet. Elevated blood glucose levels stimulate the release of insulin.
- The delta cell accounts for four percent of the islet cells and secretes the peptide hormone somatostatin. Recall that somatostatin is also released by the hypothalamus , and the stomach and intestines also secrete it. An inhibiting hormone, pancreatic somatostatin inhibits the release of both glucagon and insulin.
- The PP cell accounts for about one percent of islet cells and secretes the pancreatic polypeptide hormone. It is thought to play a role in appetite, as well as in the regulation of pancreatic exocrine and endocrine secretions. Pancreatic polypeptide released following a meal may reduce further food consumption; however, it is also released in response to fasting.
What Does The Pancreas Do
The pancreas carries out two important roles:
The pancreas produces hormones in its ‘endocrine’ cells. These cells are gathered in clusters known as islets of Langerhans and monitor what is happening in the blood. They then can release hormones directly into the blood when necessary. In particular, they sense when sugar levels in the blood rise, and as soon as this happens the cells produce hormones, particularly insulin. Insulin then helps the body to lower blood glucose levels and ‘store’ the sugar away in , muscle, liver and other body tissues where it can be used for energy when required.
The pancreas is very close to the stomach. As soon as food is eaten, the pancreas releases digestive enzymes into the bowel to break food down. As the food is digested, and nutrient levels in the blood rise, the pancreas produces insulin to help the body store the glucose away. Between meals, the pancreas does not produce insulin and this allows the body to gradually release stores of energy back into the blood as they are needed.
Glucagon Vs Insulin: Functions & Feedback Loop
Amanda has taught high school science for over 10 years. They have a Master’s Degree in Cellular and Molecular Physiology from Tufts Medical School and a Master’s of Teaching from Simmons College. They also are certified in secondary special education, biology, and physics in Massachusetts.
Glucose Metabolism And Regulation: Beyond Insulin And Glucagon
Recovery From Severe Low Blood Sugar
The student may take 5 to 20 minutes to wake up. Once the student is alert:
- Check blood sugar
- Give juice or fast-acting sugar
- Give a carbohydrate snack , if the student is able to eat.
A severe low blood sugar or the use of glucagon may cause nausea or vomiting. The student may not be able to eat or drink afterward. If this happens:
- Check blood sugar
- Seek medical help immediately
Degradation And Elimination Of Glucagon
The degradation of glucagon is mainly facilitated by receptor-mediated endocytosis and proteolysis by the ubiquitous enzyme dipeptidyl peptidase 4 . Consistent with the relative receptor expression, the liver and kidneys seem to represent the two main organs removing glucagon from the circulation. The circulating half-life of glucagon in plasma is reported to be between four to seven minutes in humans .
Insulin Basics: How Insulin Helps Control Blood Glucose Levels
Insulin and glucagon are hormones secreted by islet cells within the pancreas. They are both secreted in response to blood sugar levels, but in opposite fashion!
Insulin is normally secreted by the beta cells of the pancreas. The stimulus for insulin secretion is a HIGH blood glucose…it’s as simple as that! Although there is always a low level of insulin secreted by the pancreas, the amount secreted into the blood increases as the blood glucose rises. Similarly, as blood glucose falls, the amount of insulin secreted by the pancreatic islets goes down.
As can be seen in the picture, insulin has an effect on a number of cells, including muscle, red blood cells, and fat cells. In response to insulin, these cells absorb glucose out of the blood, having the net effect of lowering the high blood glucose levels into the normal range.
Glucagon is secreted by the alpha cells of the pancreatic islets in much the same manner as insulin…except in the opposite direction. If blood glucose is high, then no glucagon is secreted.
When blood glucose goes LOW, however, more and more glucagon is secreted. Like insulin, glucagon has an effect on many cells of the body, but most notably the liver.

