Risk Factors For Developing Hypoglycemia
The study by Apel et al identified 3 factors associated with a higher risk of developing hypoglycemia:
Renal dysfunction, in and of itself, may also be a risk factor for developing hypoglycemia. Some evidence suggests that insulin is metabolized by the kidneys to some extent. Furthermore, patients with acute kidney injury have clinically relevant changes in insulin metabolism, as evidenced by increased hypoglycemic events and lower insulin requirements upon developing AKI.6
A higher insulin dose caused more hypoglycemia .7
The 2018 study by Scott et al, identified that lower glucose prior to insulin , higher doses of insulin , and lower doses of D50 were independently associated with hypoglycemia in the multivariate analysis.5 Age, history of diabetes, and history of renal failure were not independently associated.
What Medications Are Used To Treat Hyperkalemia
treatmenthyperkalemiadrugtreatmenthyperkalemia
Drugs used in the treatment of hyperkalemia include the following:
- Calcium : Reduces the risk of ventricular fibrillation caused by hyperkalemia.
- Insulin administered with glucose: Facilitates the uptake of glucose into the cell, which results in an intracellular shift of potassium.
Furthermore, how do you treat hyperkalemia?
Similarly one may ask, what are the drugs that reduce potassium?
- Diuretics. Diuretics like furosemide, bumetanide, hydrochlorothiazide, and chlorthalidone are the main medication-related cause of low potassium levels.
- Albuterol.
- Risperdal and Seroquel.
What potassium level necessitates urgent treatment for hyperkalemia?
A Hyperkalemia Emergency, which we define as a serum potassium>6.0 meq/L or a sudden increase in serum potassium 1.0 meq/L above 4.5 meq/L within 24 hours associated with cardiopulmonary arrest, evolving critical illness, AMI, or signs and symptoms of neuromuscular weakness, should be treated with agents that
Hyperkalemia Is The Great Ecg Imitator
These ECG findings are not specific to hyperkalemia alone. Given the broad differential for these ECG changes, hyperkalemia has been dubbed the Great ECG Imitator. It is important to consider the patients presentation, clinical complaints and trends on the ECG.
PEARL: Hyperkalemia has been known to cause almost any dysrhythmia. Pay special attention to patients in slow VT and wide-complex bradycardia and consider treating them empirically as hyperkalemia.
Role Of The Pharmacist
Pharmacists can play a vital role in the management of hyperkalemia. They should be aware of newly approved treatment options and can assist with dosing of the various medications used, as well as assess for drug-inducing hyperkalemia agents. Since management options for hyperkalemia have remained consistent for many years prior to the approval of patiromer, the only comparator of the newly approved agent was SPS. Although the data regarding efficacy were limited for SPS, it became a mainstay treatment option due to lack of alternatives. The 2015 approval of patiromer now adds another option for management of hyperkalemia in the outpatient setting. Neither patiromer nor ZS-9 replace current treatment approaches for hyperkalemia. ZS-9 may be beneficial as suppressive or preventive treatment in those with CKD.
Signs And Symptoms Of Hyperkalemia
Patients with hyperkalemia may be asymptomatic, or they may report the following symptoms :
-
Generalized fatigue
-
Paralysis
-
Palpitations
Evaluation of vital signs is essential for determining the patients hemodynamic stability and the presence of cardiac arrhythmias related to hyperkalemia. Additional important components of the physical exam may include the following:
-
Cardiac examination may reveal extrasystoles, pauses, or bradycardia
-
Neurologic examination may reveal diminished deep tendon reflexes or decreased motor strength
-
In rare cases, muscular paralysis and hypoventilation may be observed
-
Signs of renal failure, such as edema, skin changes, and dialysis sites, may be present
-
Signs of trauma may indicate that the patient has rhabdomyolysis, which is one cause of hyperkalemia
See Clinical Presentation for more detail.
Errors When Treating Hyperkalemia
When treating hyperkalemia, the potential for errors and patient harm is significant due to the urgency of the treatment, the difficulty in measuring and administering bolus doses of IV insulin, and the risk of treatment-induced hypoglycemia. A 2017 analysis of almost 200 adverse events associated with hyperkalemia treatment showed that delayed treatment and administration of insulin by the wrong route or the wrong dose were the most common types of errors.1 The analysis also showed that, despite the administration of dextrose, hypoglycemia was still a relatively common occurrence often linked to the variability in dextrose and insulin dosing, the type of insulin used, duration of the dextrose and insulin infusion, the sequence of administering the dextrose and insulin, and patient factors such as renal dysfunction. Some episodes of hypoglycemia have also been caused by administering only the insulin portion of the treatment and not the glucose component.2
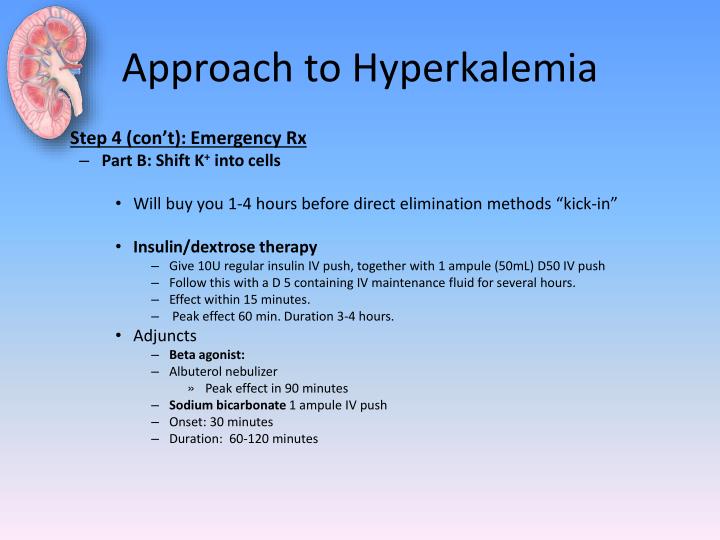
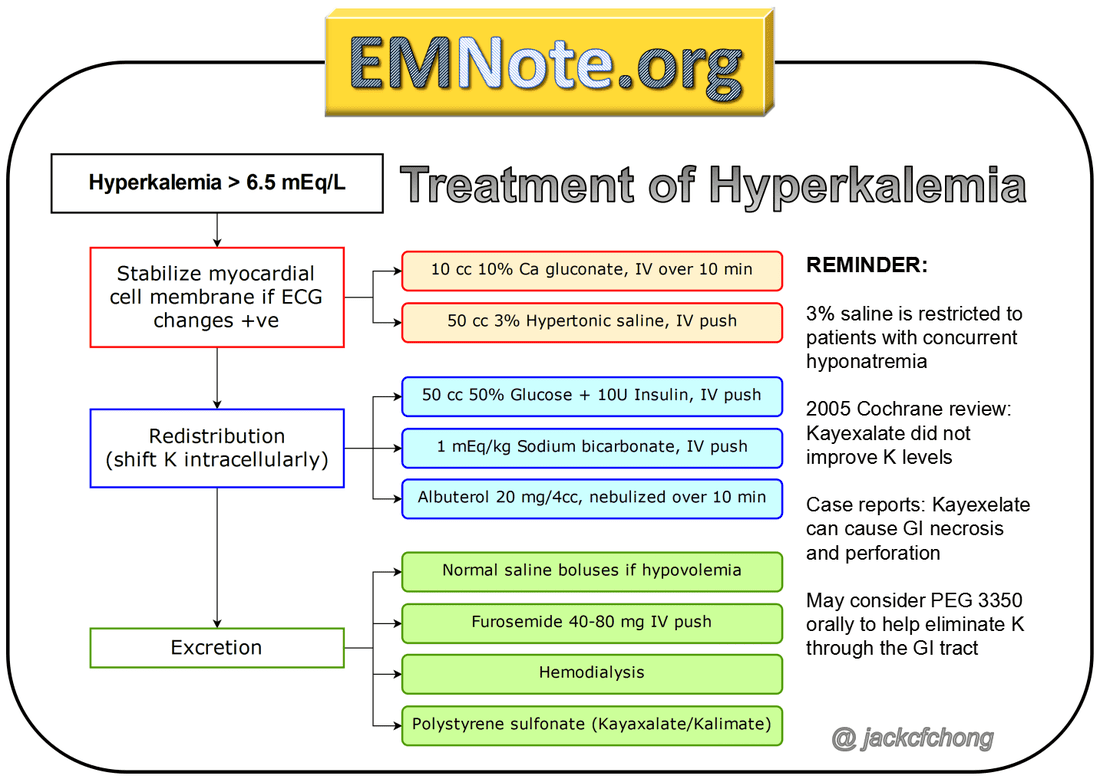
General Approach To Emergency Management Of Hyperkalemia
Place the patient on a cardiac monitor, establish IV access and obtain an ECG
If the patient is stable, consider the cause and rule out pseudohyperkalemia and repeat the potassium to confirm hyperkalemia.
Stabilize the cardiac membrane with Calcium Gluconate 1-3 amps
if:
a) K>6.5 or
c) absent p waves or
d) peri-arrest/arrest
Drive K into cells with 2 amps D50W + Regular Insulin 10 units IV push
followed by B-agonists 20mg by neb or 8 puffs via spacer if:
a) K>5 with any hyperkalemia ECG changes or
b) K>6.5 regardless of ECG findings
Eliminate Kthrough the kidneys and GI tract while achieving euvolemia and establish good urine flow
Normal Saline IV boluses if hypovolemia
Furosemide IV only ifhypervolemic
PEG 3350 17g orally for alert patients remaining in your ED for prolonged period of time
Dialysis for arrest, peri-arrest, dialysis patient or severe renal failure
Monitor rythym strip, glucose at 30 mins, K and ECG at 60 mins
and repeat as needed until the K is below 6, ECG has normalized and/or dialysis has been started
Treatment And Prevention Of Hyperkalemia In Adults
INTRODUCTION Hyperkalemia is a common clinical problem that is most often a result of impaired urinary potassium excretion due to acute or chronic kidney disease and/or disorders or drugs that inhibit the renin-angiotensin-aldosterone system . Therapy for hyperkalemia due to potassium retention is ultimately aimed at inducing potassium loss . In some cases, the primary problem is movement of potassium out of the cells, even though the total body potassium may be reduced. Redistributive hyperkalemia most commonly occurs in uncontrolled hyperglycemia . In these disorders, hyperosmolality and insulin deficiency are primarily responsible for the transcellular shift of potassium from the cells into the extracellular fluid, which can be reversed by the administration of fluids and insulin. Many of these patients have a significant deficit in whole body potassium and must be monitored carefully for the development of hypokalemia during therapy. The treatment and prevention of hyperkalemia will be reviewed here. The causes, diagnosis, and clinical manifestations of hyperkalemia are discussed separately. DETERMINING THE URGENCY OF THERAPY The urgency of treatment of hyperkalemia varies with the presence or absence of the symptoms and signs associated with hyperkalemia, the severity of the potassium elevation, and the cause of hyperkalemia. Our approach to therapeutic urgency is as follows :Continue reading >>
Can Lactulose Be Used For Hyperkalemia
4.4/5Lactulosehyperkalemialactuloseused
Diarrhea may occur if the dose of lactulose is too high. Problems associated with diarrhea are fluid and potassium loss in the diarrheal stool leading to dehydration and low blood levels of potassium .
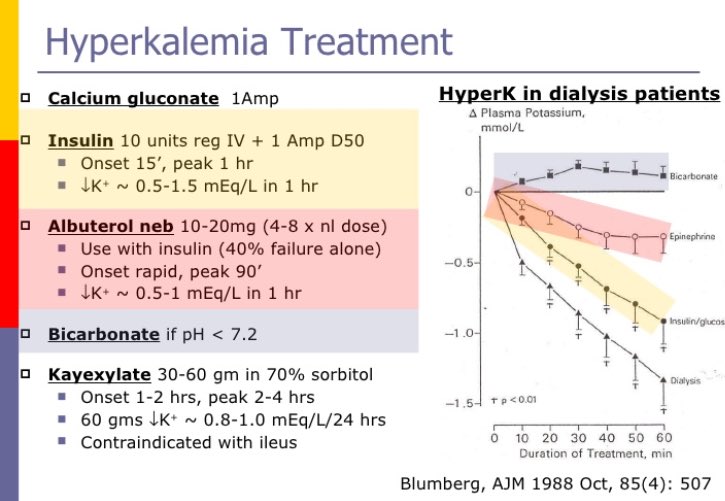
Also Know, does calcium bind to potassium? Calcium is given intravenously to protect the heart, but calcium does not lower the potassium level. Then insulin and glucose are given, which move potassium from blood into cells, thus lowering the potassium level in blood. Albuterol may be given to help lower the potassium level.
Moreover, how does albuterol work in hyperkalemia?
Albuterol is an adrenergic agonist that has an additive effect with insulin and glucose, which may in turn help shift potassium into the intracellular space. This agent lowers the serum potassium level by 0.5-1.5 mEq/L. It can be very beneficial in patients with renal failure when fluid overload is concern.
What is the emergency treatment for hyperkalemia?
Drugs used in the treatment of hyperkalemia include the following: Calcium : Reduces the risk of ventricular fibrillation caused by hyperkalemia. Insulin administered with glucose: Facilitates the uptake of glucose into the cell, which results in an intracellular shift of potassium.
Examples Of Recent Errors
Several recent insulin errors during hyperkalemia treatment have been reported to ISMP or have appeared in the literature. For example, just this month, we learned about an error in which a nurse correctly calculated the volume needed for a 10 unit dose of insulin lispro, but accidentally measured out 20 units of insulin using a 10 mL non-insulin syringe. A physician prescribed treatment that included calcium gluconate 1 g IV, insulin lispro 10 units IV, and dextrose 50% IV. The nurse calculated that she would need 0.1 mL of the insulin for the 10 unit dose, and a nurse manager verified the calculation. Using a 10 mL syringe, she drew the insulin lispro into the syringe up to the first gradation mark, believing this represented 0.1 mL. But the first syringe marking was actually 0.2 mL. The nurse manager did not verify the dose in the syringe prior to administration. The error was quickly discovered when a clinical nurse specialist asked the nurse, who had just completed orientation, to demonstrate how she had measured the insulin dose in a 10 mL syringe. The patients blood glucose was monitored, and she experienced no adverse effects.
Hyperkalemia In Cardiac Arrest
Based on the principles of treatment and indications discussed above, our experts recommend the following approach to suspected hyperkalemia or confirmed hyperkalemia in cardiac arrest in addition to usual ACLS measures:
Push 1 amp calcium chloride in well running peripheral IV or central line and repeat until the QRS is <100ms
Epinephrine 5-20 mcg q2-5 minutes
Sodium Bicarbonate 1 amp IV
Shift potassium with Insulin and Glucose followed by B-agonist
Dialysis
Rebound Hyperkalemia
In cases of cardiac arrest due to hyperkalemia, perform CPR until the hyperkalemia is corrected. This may be a much longer time than usual. When ROSC is achieved, it will be primarily due to the effects of calcium rather than decreased potassium levels. The effect of calcium can last 20-30min. Since the stabilizing effects of calcium will wear off, you must promptly work on shifting the potassium and enhancing its elimination as described above. Consider repeating the calcium bolus if there are any worsening ECG changes. Repeat serial potassium measurements to monitor for rebound hyperkalemia, which occurs more often than wed like.
PEARL: the patient in cardiac arrest with hyperkalemia should not be pronounced dead until their potassium level is normalized
Rx Severe Hyperkalemia: Temporizing Measures
IV calcium to stabilize the myocardium
- IV calcium is indicated for patients with EKG changes or a potassium >6.5 mM.
- Initial dose:
- Peripheral access: 3 grams IV calcium gluconate over 10 minutes.
- Central access: 1 gram IV calcium chloride over 10 minutes or slow IV push.
IV insulin plus dextrose to shift potassium into cells
- Insulin dose: 5 units IV insulin .
- Dextrose dose:
- Traditionally, 2 ampules of D50W has often been used . Only one ampule of D50W may be inadequate to prevent hypoglycemia.
- D10W may be used instead . D10W has the advantages of causing less rebound hypoglycemia and less irritation of veins.
- Dextrose administration may be omitted if the baseline glucose level is already >250 mg/dL . If the baseline glucose is high then the dose of dextrose might be cut in half, to 25 grams.
beta-2 agonists
bicarbonate
Patients Without Risk Factors For Hypoglycemia After Insulin
If patients do not have any risk factors for hypoglycemia after insulin, no modification to traditional practice is needed. Some sources recommend holding dextrose if pre-treatment blood glucose is greater than 250 mg/dL.7 However, monitoring blood glucose every hour for 4 to 6 hours after insulin is still recommended regardless of the number of risk factors the patient has for hypoglycemia.
Medication Errors During Insulin Administration For Patients With Hyperkalemia
Hyperkalemia is a serious, potentially lethal electrolyte disturbance that requires medical treatment without delay if it is severe enough to cause disturbances in cardiac conduction. Although hyperkalemia treatment guidelines in the literature vary,1 many organizations begin treatment with the administration of one or more intravenous bolus doses of 50% dextrose and an IV bolus dose of 10 units of insulin. Some organizations use a rapid-acting insulin rather than short-acting insulin because it may decrease the incidence of hypoglycemia, given its shorter half-life.1
Association Between Hyperkalemia And Outcomes
The potassium ion is the most abundant cation in the body. There is an estimated total reserve of 30004000 mmol in adults, of which only 60 mmol are extracellular . Hyperkalemia is associated with poor outcomes in many different settings: in the general population , in patients with cardiac and renal disease and in critically ill patients . In a retrospective study of hospitalized patients, Khanagavi et al. found that acute kidney injury and prolonged hyperkalemia are independent predictors of in-hospital mortality. In acute myocardial infarction, a serum potassium above 4.5 mmol/L is associated with a higher mortality . More recently, Legrand et al. identified that a serum potassium>4.5 mmol/L in heart failure patients admitted to the emergency department is associated with an increased risk of death.
The net effect is a U-shaped mortality curve associated with potassium abnormalities . Several observational studies have identified hypokalemia as an independent risk factor for poor outcome . This association raises concern regarding the potential for overcorrection, as may occur with some fast-acting potassium-lowering agents. However, these associations do not mean causality and thresholds for treating hyperkalemia remain debated.
Causes Of Hyperkalemia In Acutely Ill Patients
Factors associated with the development of hyperkalemia can be classified into three categories, and include altered renal clearance of potassium , release from the intracellular space and altered transfer to the intracellular space . Hyperkalemia in the patient with normal renal function is unusual and should prompt evaluation for pseudo-hyperkalemia if no ECG abnormalities consistent with hyperkalemia are identified . While concomitant medications are often a contributor to hyperkalemia, in our experience they are rarely the only cause in acute settings.
Table 1 Mechanisms contributing to the development of hyperkalemia
A special warning should be made with regards to the use of succinylcholine, classically used to induce paralysis in acutely ill patients for rapid sequence intubation. Succinylcholine induces skeletal muscle cell depolarization with an efflux of intracellular potassium by nicotinic receptor activation. In a population of critically ill patients, succinylcholine increased serum potassium on average 0.4 mmol/L . It should be avoided in patients with hyperkalemia and in patients with up-regulation of nicotinic receptors, as they are at risk of greater potassium elevation. This includes those with anatomical denervation, prolonged administration of neuromuscular blocking drugs, burn injury, and prolonged immobilization . Alternative to succinylcholine are available in patients at risk of hyperkalemia .
Medications In The Emergency Management Of Hyperkalemia
Three main principles
There are specific treatments geared at targeting each of these three main principles, which we will discuss below. Unfortunately, there is no clear evidence to guide exactly when to initiate specific treatments for hyperkalemia. Our experts recommend using two factors to guide your management:
with the following indications for immediate treatment of hyperkalemia in the ED:
Principle 1: Stabilize the cardiac membrane
There is no good literature to help guide whether calcium gluconate or calcium chloride is better for stabilizing the cardiac membrane in hyperkalemia. The most important difference to remember is that calcium chloride has 3 times more elemental calcium than calcium gluconate and has greater bioavailability. However, calcium gluconate has less risk of local tissue necrosis at the IV site. Therefore, if you decide to give calcium gluconate, ensure you are giving sufficient doses of calcium since one amp may not be enough. Three amps of calcium gluconate are often required to start to see the ECG changes of hyperkalemia resolve. Remember that calcium does not lower the potassium level.
Our experts recommend using calcium chloride through a large well-flowing peripheral IV or central line in the arrest or peri-arrest patient. Calcium gluconate is recommended for all other patients given its lower risk for local tissue necrosis.
Monitor glucose q30 minutes
Rx Severe Hyperkalemia: Potassium Elimination
dialysis vs. kaliuresis
- Ultimately, most patients will require elimination of excess potassium from the body. This may be achieved either via the kidneys or via dialysis.
- Patients with end-stage renal disease on chronic dialysis will require emergent dialysis . For most other patients, kaliuresis should be attempted prior to emergent dialysis.
kaliuresis step #1 = volume resuscitation if hypovolemic
- Many patients present with renal failure and hyperkalemia due to volume depletion. The first step in managing these patients is volume repletion.
- Isotonic bicarbonate is the preferred resuscitative fluid in metabolic acidosis .
- The isotonic bicarbonate should be dosed with the goal of bringing the patient’s serum bicarbonate level back to a high-normal level . The dose can be estimated by calculating the patient’s bicarbonate deficit . Divide the bicarbonate deficit by 150 to estimate the number of liters of isotonic bicarbonate needed. The dose is usually 1-2 liters.
- Bicarbonate should be infused rapidly for patients with hypovolemia and severe hyperkalemia .
- If the patient remains hypovolemic after receiving enough sodium bicarbonate to normalize the serum bicarbonate level, then residual hypovolemia can be treated with lactated ringers.
kaliuresis step #2 = consider fludrocortisone
kaliuresis step #3 = diuretic cocktail
Insulin Dosing Evaluation In Hyperkalemia
Several studies have compared insulin dosing strategies in hyperkalemia.8-10,13,18 These studies compared patients receiving 10 units to lower doses, such as 5 units or 0.1 unit/kg, and assessed for potassium-lowering ability and incidence of hypoglycemia.8-10,13,18 Hypoglycemia was generally defined as blood glucose less than 70 mg/dL; however, there were varying definitions of severe hypoglycemia and duration of monitoring for hypoglycemia after insulin administration.8-10,13,18
Determine The Cause Of Hyperkalemia
First rule out pseudohyperkalemia which accounts for 20% of hyperkalemia lab values.
Pseudohyperkalemia is caused by hemolyzed sample, poor phlebotomy technique leukocytosis or thrombocytosis.
Then treat the underlying cause:
- Medications: ACEi, Potassium sparing diuretics, B-Blockers, NSAIDs, Trimethoprim and Non-prescription salt substitutes
- Renal Failure
- Cell death: Secondary to rhabdomyolisis, massive transfusion, crush or burn injuries.
- Acidosis: Consider Addisons crisis, primary adrenal insufficiency and DKA.
PEARL: If hyperkalemia cannot be explained by any other cause and the patient has unexplained hypotension, draw a random cortisol and ACTH level and give 100 mg IV solucortef for presumed adrenal insufficiency.
Lowering Total Body Potassium
Treatments that shift potassium into the cells have no effect on total body potassium. Potassium can be eliminated by renal excretion, gastrointestinal elimination, or dialysis. The agents taken to lower total body potassium can interfere with tests to determine the cause of hyperkalemia. Thus, spot urine potassium, creatinine, and osmolality levels should be obtained before the agents are initiated; however, treatment should not be delayed while awaiting results.
Gastrointestinal excretion is accomplished using sodium polystyrene sulfonate , which binds potassium in the colon in exchange for sodium; it can be given orally or as a retention enema. The enema form is faster; the oral route can take four to six hours because it requires the resin to get to the colon before it takes effect. Sodium polystyrene sulfonate often is given with sorbitol to decrease constipation. However, sorbitol can have intestinal complications, with reports of bowel necrosis and perforation in immunocompromised patients. Using furosemide with polystyrene reduces the risk of volume overload because of the sodium that is exchanged for potassium by the resin .
Step 2: Intracellular Potassium Shift
Alright. So weve stabilized the myocardium .
Now for the next step; actually lowering serum potassium levels. How do we do that? Like I said before, you can either shift the potassium into the cells, or remove it entirely from the body.
Let’s start with shifting potassium into the cells. It works faster than potassium removal, so this will help keep us out of the danger zone while we buy ourselves more time.
There are a few ways to shift potassium into the cells:
-
Insulin
-
Beta-2 agonists
-
Bicarbonate
Your first choice in an emergent situation is usually insulin. Its safe and works quickly .
A typical dose of insulin for hyperkalemia is 5 10 units IV.
Of course, insulin is not so safe if your patient has low blood sugar . So IV dextrose is usually given alongside the insulin to balance that out.
If your patients blood glucose is > 250 mg/dL, you don’t need to worry about giving the dextrose because they’ve got enough of a blood sugar buffer to handle 10 units of insulin.
You can also use beta-2 agonists for hyperkalemia. They lower serum potassium , but they take a lot longer.
You could consider albuterol adjunctive therapy for hyperkalemia . The usual dose is albuterol 20 mg via nebulizer.
So, what is this magical mechanism that insulin and albuterol BOTH use to lower serum potassium?
All they’re doing is increasing the activity of Na+-K+-ATPas .
Another way to force potassium into the cells is with sodium bicarbonate.
How does that work?
Clinical Manifestations Of Hyperkalemia
Clinical manifestations of mild to moderate hyperkalemia are usually non-specific and may include generalized weakness, fatigue, nausea, vomiting, intestinal colic, and diarrhea. Severe hyperkalemia may lead to life-threatening conditions such as cardiac arrhythmias and muscle paralysis.
Potassium and sodium play a key role in the function of the myocardium; therefore, their concentration gradients are strictly maintained. Any imbalance of this concentration gradient affects the ability of the heart to maintain a normal rhythm. The concentration gradient is maintained by the sodium potassium ATPase pumps located on the cellular membrane that actively pump sodium outside and potassium inside the cell. When the potassium level increases in the extracellular space, the potassium concentration gradient across the cellular wall decreases; and this decreases the resting membrane potential. The change in resting membrane potential caused by hyperkalemia is the principle pathophysiologic mechanism behind most of its symptoms. The decrease in the resting membrane potential decreases the number of sodium channels activated that in turn decrease the magnitude of inward sodium current. This causes a prolonged conduction of the impulse with prolonged depolarization .
Insulin For The Treatment Of Hyperkalemia: A Double
Potassium plays a critical role in cellular metabolism and normal neuromuscular function. Tightly regulated homeostatic mechanisms have developed in the process of evolution to provide primary defense against the threats of hyper- and hypokalemia. The kidney plays a primary role in potassium balance, by increasing or decreasing the rate of potassium excretion. Distribution of potassium between the intracellular and the extracellular fluid compartments is regulated by physiologic factors such as insulin and catecholamines which stimulate the activity of the Na+-K+ ATPase. Only about 10% of the ingested potassium is excreted via the gut under normal physiologic conditions .
The definition of hypoglycemia has been a topic of debate. The workgroup of the American Diabetes Association and the Endocrine Society defines iatrogenic hypoglycemia in patients with diabetes mellitus as all episodes of an abnormally low plasma glucose concentration that expose the individual to potential harm. A plasma glucose concentration of 70 mg/dL is recommended as the alert value even though symptoms of hypoglycemia usually develop at a level below this threshold . This value allows time for close monitoring of the patient to prevent symptomatic hypoglycemia and has been used to define hypoglycemia in numerous clinical trials.
Disclosures. None declared.
Cardiac Manifestations Of Hyperkalaemia
Although patients with hyperkalemia can present rarely with weakness progressing to flaccid paralysis, paresthesias, or depressed deep tendon reflexes, the clinical presentation of hyperkalemia is usually benign until cardiac rhythm or conduction disorders occur. Elevation of extracellular potassium has several effects on myocardial electrophysiology that contribute to intracardiac conduction disturbances. The intracellular to extracellular potassium gradient lessens when extracellular potassium increases, thus decreasing the resting membrane potential. Elevated extracellular potassium also increases membrane permeability for potassium, lowers membrane resistance, increases repolarizing currents, and shortens transmembrane action potential duration.
While rising serum potassium initially increases conduction velocity, it decreases it at higher levels . Classic hyperkalemia electrocardiographic findings include signs of hyperexcitability such as peaked T-waves . Further, altered conduction may manifest as PR prolongation, loss of P-waves, QRS widening, bradycardia, and ultimately a sine wave rhythm due to action potential shortening and prolongation of diastolic depolarization.

