Insulin Shows The Importance Of Unrelated Basic Research In The Development Of Medical Treatments
Diabetes was a fatal disease before insulin was discovered on July 27, 1921. A century ago, people diagnosed with this metabolic disorder usually survived only a few years. Physicians had no way to treat their diabetic patients’ dangerously high blood sugar levels, which were due to a lack of the hormone insulin. Today, though, nearly 1.6 million Americans are living normal lives with Type 1 diabetes thanks to the discovery of insulin.
This medical breakthrough is usually attributed to one person, Frederick Banting, who was searching for a cure for diabetes. But getting a reliable diabetes treatment depended on the research of two other scientists, Oskar Minkowski and Søren Sørensen, who had done earlier research on seemingly unrelated topics.
, and I teach a course on the history of the treatment of diabetes. With my students, I emphasize the importance of unrelated basic research in the development of medical treatments. The story of insulin illustrates the point that medical innovations build on a foundation of basic science and then require skilled engineers to get a treatment out of the lab and to the people who need it.
Basic research pointed to the pancreas
Diabetes had been known since antiquity. The first symptoms were often a prodigious thirst and urination. Within weeks the patient would be losing weight. Within months, the patient would enter a coma, then die. For centuries, no one had any clue about what caused diabetes.
Isolating the insulin
Explore further
Types Of Insulin Administration With Needles Pumps Pens And Why Insulin Is So Expensive
Lisa JaffeAmy Hess-Fischl MS, RD, LDN, BC-ADM, CDEJessica Rodriguez CNP
What does insulin do? Help your body turn food into energy, for starters. When you’re diabetic, and you’re either not producing insulin, or your insulin function is off, all sorts of things can go wrong. From needles, to pens, to pumps, to types of insulin, we’re here to empower you with clear answers to all your pressing Qs.
In This Article:
Alvin Powers MD, Mihail Zilbermint MD, and Irl Hirsch MD
What Severe Complications Can Occur Because Of Rationing Or Running Out Of Insulin
Diabetic ketoacidosis is an emergency condition that results if you don’t have enough insulin to regulate your blood sugar. DKA causes your body to break down fat for energy in the absence of insulin. This leads to a dangerous accumulation of acids known as ketones in your blood that can cause your brain to swell and your body to go into shock.
Signs of diabetic ketoacidosis include:
- Thirst or a very dry mouth
- Frequent urination
- High levels of ketones in your urine
- Fatigue
- Nausea, vomiting, or stomach pain
- Difficulty breathing
- A fruity or acetone odor on your breath
- Confusion or acting “drunk” while sober
DKA is so common and can come on so quickly that it is the first sign of Type 1 diabetes in 20% of cases, and the way many type 1 diabetics are first diagnosed with the condition. If you go into diabetic ketoacidosis, don’t try to hide it or make light of it. Treat it as the emergency it is and get to a hospital as soon as possible to recover. “I’ve had people tell me they’re tired of taking insulin, or that they’re rationing it due to cost. In type 1 diabetes, that’s all it takes to end up in a life-threatening situation,” says Dr. Zilbermint.
Another complication facing diabetics who use insulin is the potential for hyperglycemia, also known as “insulin shock,” which involves using too much insulin and causing your blood sugar to drop extremely low. “This can cause coma, seizures, and heart attacks,” says Dr. Powers.
Changes In Blood Flow To The Brain And Parasympathetic Nervous System Activity
After a meal, copious quantities of blood are routed to the gastrointestinal tract to facilitate digestion and the shuttling of absorbed nutrients to target cells and tissues. This process reroutes blood away from the brain. Some scientists argue that the rerouting of blood away from the brain to the digestive organs precipitates hypoarousal and sleepiness. Eating smaller meals may place less demand for blood flow to the digestive organs, resulting in a concordant decrease in the amount of blood shunted away from the brain. One study supporting this finding found that the consumption of larger meals led to more significant sleepiness during a long, monotonous driving task.
The act of digestion also shifts the body out of the “fight, flight, or freeze” sympathetic nervous system state and into the “rest and digest” parasympathetic nervous system state. This shift may, in part, be responsible for the meal-induced sleepiness. We don’t want to prevent our bodies from shifting into the parasympathetic state while eating since this nervous system state facilitates gastric acid and digestive enzyme production for adequate food digestion. However, eating small meals may mitigate the magnitude of parasympathetic activation.
Years Of Insulin: Creating A Diabetes Treatment Took More Than A Breakthrough

Graffiti in New York city depicting vials of an insulin analog, October 2014. Photo: Ittmust/Flickr, CC BY 2.0
- The story of insulin illustrates the point that medical innovations build on a foundation of basic science and then require skilled engineers to get a treatment out of the lab and to the people.
- Today, the implacable enemies of humans include cancer, Alzheimer’s disease and schizophrenia. The cures for each will likely be built from advances made by basic research.
Diabetes was a fatal disease before insulin was discovered on July 27, 1921. A century ago, people diagnosed with this metabolic disorder usually survived only a few years. Physicians had no way to treat their diabetic patients’ dangerously high blood sugar levels, which were due to a lack of the hormone insulin. Today, though, nearly 1.6 million Americans are living normal lives with Type 1 diabetes thanks to the discovery of insulin.
This medical breakthrough is usually attributed to one person, Frederick Banting, who was searching for a cure for diabetes. But getting a reliable diabetes treatment depended on the research of two other scientists, Oskar Minkowski and Søren Sørensen, who had done earlier research on seemingly unrelated topics.
Basic research pointed to the pancreas
Isolating the insulin
Insight from a brewery
This insight allowed for mass production of insulin.
Vanquishing a human disease
James P. Brody is a professor of biomedical engineering, University of California, Irvine.
What Are Alternative Medications For People With Diabetes That Arent Insulin
- Metformin – a pill that stops sugar production in the liver
- Glitazones – pills that remove sugar from the bloodstream
- Sufonylureas and glinides – pills that increase the release of insulin from your pancreas
- Starch blockers – pills that slow starch absorption
- Incretin therapies and amvlin analogs – pills and injections that reduce sugar production in the liver and slow food absorption. Types of the former include DPP4 inhibitors and GLP1 analogs .
- SGLT2 inhibitors – pills that are taken before meals that prevent the reabsorption of glucose
The Digestive Process: What Is The Role Of Your Pancreas In Digestion
Your pancreas plays a big role in digestion. It is located inside your abdomen, just behind your stomach. It’s about the size of your hand. During digestion, your pancreas makes pancreatic juices called enzymes. These enzymes break down sugars, fats, and starches. Your pancreas also helps your digestive system by making hormones. These are chemical messengers that travel through your blood. Pancreatic hormones help regulate your blood sugar levels and appetite, stimulate stomach acids, and tell your stomach when to empty.
Gut Check: How To Prevent Or Control Digestive Issues In Diabetes
But just because you have diabetes doesn’t mean you have to resign yourself to digestive problems as well. To help keep your digestive system in working order, follow these tips:
Keep your blood sugar tightly controlled. Whether you’re looking to prevent or control digestive problems when you have diabetes, it is most important to rigorously pay attention to control blood sugar and keep your A1C within a healthy range, Reynolds says. “A1C elevation is directly proportional to the level at which esophageal function and gastric function is impaired,” he says. Everyone’s A1C goal is different — talk to your doctor to learn yours.
Choose a healthy diet low in sugar and refined carbs. “A diet high in refined sugar can mess up the gut bacteria,” Cline says. He recommends staying away from foods high in saturated fat and refined carbohydrates, such as white bread, pasta, and rice, as well as processed sweets and snacks, like refined pastries and granola bars.
Research also suggests eating a healthy diet could help minimize disease progression, which is associated with neuropathy. A , for instance, found that a certain substance produced by gut microbes is associated with a reduced likelihood of progression of type 2 diabetes in overweight people with prediabetes. That substance, indolepropionic acid, is linked with dietary fiber intake, the authors noted.
The Primary Hormones That Are Produced By The Pancreas Include:
- Insulin – this hormone works by allowing the body’s cells to absorb glucose from the bloodstream and use it as energy. This in turn helps to reduce high blood sugar levels.
- Gastrin – gastrin hormone stimulates specific cells in the stomach that aids in digestion.
- Glucagon – this hormone helps insulin to maintain a normal blood sugar level by stimulating the cells to release glucose when it is too low.
- Vasoactive intestinal peptide – vasoactive intestinal peptide helps to control absorption and secretion of water from the intestines.
- Somatostatin – in case other hormones such as glucagon and insulin are too high, the hormone somatostatin will be released to help maintain blood sugar.
How Diabetic Neuropathy Can Lead To Heartburn And Other Issues
So how might diabetes affect the digestive system? “Advanced diabetes, whether it’s from type 1 or type 2 diabetes, can affect any organ in the body — including those organs in the digestive tract,” says James C. Reynolds, MD, a gastroenterology specialist and clinical medicine professor at the University of Pennsylvania in Philadelphia.
Dr. Reynolds notes digestive problems may be caused by the very factors that led to diabetes in the first place, such as obesity, but it’s also possible that digestive problems are the result of diabetes-related complications, such as hyperglycemia, or high blood sugar.
One of the most serious diabetes complications that can result from consistent high blood sugar is diabetic neuropathy, or nerve damage. Neuropathy may lead to weakness, pain, and numbness, affecting feeling in your feet, legs, and hands, but the condition can also affect digestive functions like swallowing and constipation, Reynolds explains.
If you have diabetes, this potential complication is just another reason it’s crucial to pay attention to your A1C, the average level of glucose over the past two to three months, Reynolds says.
The Precious Pancreas: Insulin Glucagon And Digestive Juices
Posted on 10/10/19 by Adelaide Elkin
Located behind the stomach and at the back of the abdomen is the six-inch-long, tadpole-shaped pancreas. From head to tail, the pancreas extends across the abdomen. The head is based where the stomach meets the duodenum .
The pancreas in context. Image from Human Anatomy Atlas.
The pancreas is an accessory digestive organ made of small glandular clusters of epithelial cells. It’s crucial for converting food to fuel for body cells and contains both endocrine and exocrine gland cells.
Regulation Of Blood Glucose Levels By Insulin And Glucagon
Glucose is required for cellular respiration and is the preferred fuel for all body cells. The body derives glucose from the breakdown of the carbohydrate-containing foods and drinks we consume. Glucose not immediately taken up by cells for fuel can be stored by the liver and muscles as glycogen, or converted to triglycerides and stored in the adipose tissue. Hormones regulate both the storage and the utilization of glucose as required. Receptors located in the pancreas sense blood glucose levels, and subsequently the pancreatic cells secrete glucagon or insulin to maintain normal levels.
How Do You Choose The Right Syringe For Injecting Insulin
Just as there are different sizes of syringes for administering insulin, there are also varying sizes of insulin needles. Shorter needles usually mean less sting when injecting. The downside is that the shallower the injection is, the longer it takes for the insulin to work. Your doctor will help you find the balance that’s best for you.
The Digestive Process: What Is The Role Of Your Pancreas
Unlike enzymes that are released into your digestive system, Insulin causes the body’s cells to take up glucose from the blood; glucagon causes the liver to release glucose into the blood, Beta cells make up about 75% of pancreatic hormone cells, protein and carbohydrates, How is insulin related to the digestive system? Insulin is released from the beta cells in your pancreas in response to rising glucose in your bloodstream, Many endocrine organs exist throughout the body , which secretes various digestive enzymes into the small intestine, causing the symptoms of late dumping syndrome, primarily in response to glucose.1 The beta cells of the pancreas are perfectly designed “fuel sensors” stimulated by glucose.2 As glucose levels rise in the plasma of the blood, This hormone is made in cells of the pancreas known as beta cells, Gastroparesis is a chronic disorder of the digestive tract that causes food to remain in the stomach longer than it should.The islet cells of the pancreas secrete the hormones insulin and glucagon into the bloodstream, What is the size of the liver and where is it located?-
Preventing Digestive Issues In Diabetes: The Bottom Line
“Keeping blood sugar under control is key to prevent gastrointestinal issues from occurring,” Cline says.
If you have any symptoms, make sure to reach out to your medical team: “With gastroparesis, it’s especially important to treat it early,” Cline explains. “With time and if left untreated, more nerve damage to the intestine occurs.” By communicating with your providers, you can settle on a course of treatment and help prevent any severe complications.
What Are The Drawbacks To Insulin Treatment For Diabetes
The biggest issue with insulin right now is unaffordability. “A box of rapid-acting insulin can cost $400 without insurance. As so many people continue to lose their health coverage, it’s becoming an enormous problem,” Dr. Zilbermint says.
Consistently rising costs have led some patients to ration their insulin, which can be dangerous and even deadly. The cost of testing strips is also an issue, and both have led to a black market in testing strips and insulin. “It’s illegal,” says Dr. Zilbermint, “but it’s happening.”
What Else Can I Do To Control My Blood Glucose Levels
Food, sleep, and exercise are all of vital importance for regulating your blood sugar when you have diabetes.
Where Can I Find Help Acquiring Or Paying For Insulin
The ADA has a dedicated page for helping people who need insulin get it, regardless of finances: http://www.insulinhelp.org.
JRDF has a page with a variety of links to organizations who also supply insulin assistance: https://www.jdrf.org/t1d-resources/living-with-t1d/insurance/help-with-prescription-costs/
Production Of Hormones To Control Blood Sugar Levels
A small proportion of the pancreas is made up of other types of cells called islets of Langerhans. These cells sit in tiny groups, like small islands, scattered throughout the tissue of the pancreas. The islets of Langerhans contain alpha cells which secrete glucagon and beta cells which secrete insulin.
Insulin and glucagon are hormones that work to regulate the level of sugar in the body to keep it within a healthy range. Unlike the acinar cells, the islets of Langerhans do not have ducts and secrete insulin and glucagon directly into the bloodstream.
Depending on what you’ve eaten, how much exercise your muscles are doing, and how active your body cells are, the amount of glucose in your bloodstream and cells varies. These 2 hormones have the job of keeping tight control of the amount of glucose in your blood so that it doesn’t rise or fall outside of healthy limits.
Digestive Ailments Are Common In Those With Diabetes
In a study published in 2018, researchers asked 706 individuals with type 1 diabetes, and 604 individuals without diabetes, a series of questions about their gastrointestinal symptoms and quality of life.13 They found that lower gastrointestinal symptoms – including constipation, diarrhea, abdominal pain, bloating, intestinal gas, and floating stools – were much more common in the individuals with diabetes, especially diarrhea and constipation, which were twice as likely in those with diabetes. These symptoms were associated with lower quality of life and poor glycemic control. However, the researchers were able to identify, and treat accordingly, the cause of diarrhea in 72% of cases, leading to a better outcome for the patients. If you have diabetes and experience digestive symptoms, make sure to let your health care team know so that you can work together to manage these symptoms.
Healthy Digestion And Converting Foods Into Energy
To understand diabetes, it helps to know how our bodies handle the sugars and energy found in our food and drinks.
In people with diabetes, this process can go wrong in two ways. Either:
People with diabetes may have the following symptoms when their blood sugar is extremely high:
- Confusion
- Increased urination
- Lethargy
Diet And Dysbiosis Influence Metabolic Endotoxemia
Diet has a significant influence on intestinal barrier integrity and plays a critical role in the pathogenesis of metabolic endotoxemia. Consuming an anti-inflammatory, nutrient-dense, whole-foods diet is a crucial first step toward improving the health of the gut barrier and microbiota.
Gut dysbiosis increases the absorption and systemic circulation of LPS, so it is also essential to address gut imbalances alongside dietary treatment.
What Is The Function Of Insulin In The Human Body
Insulin helps in the metabolism of the body and without this hormone, we cannot live.
It depresses blood glucose levels in different ways including glycogen synthesis and increasing the cell consumption of glucose. It also stimulates the conversion of glucose into proteins and lipids, which reduces the level of glucose.
Insulin also inhibits the hydrolysis of glycogen in the liver and muscles.
Endocrine And Exocrine Functions Of The Pancreas
The exocrine cells of the pancreas produce enzymes that combine with electrolytes and water to become part of a digestive fluid called pancreatic juice. It is carried by a network of pancreatic ducts to the small intestine. The juice promotes digestion as it helps break down carbs, fats, and proteins. About 1200-1500 mL of pancreatic juice is produced daily!
The pancreas , its ducts, and the duodenum. Image from Human Anatomy Atlas.
The pancreas also contains around a million pancreatic islets , which are hormone-producing cell clusters. The islets contain two major populations of hormone producing cells: the glucagon-synthesizing alpha cells and the insulin-synthesizing beta cells. These cells secrete glucagon or insulin during the fasting and full states and can sense when the body needs and doesn’t need food.
Postprandial Somnolence: Why A Food Coma Happens
Have you ever eaten a meal, and 30 minutes to an hour later, felt a wave of somnolence sweep over your body? While it’s normal to feel sleepy after eating a large meal, such as Thanksgiving dinner, it’s not normal to frequently experience fatigue, brain fog, or other symptoms after normal-sized meals
Postprandial fatigue, colloquially referred to as a “food coma,” is defined as a substantial decrease in energy levels after meals. Read on to learn about what postprandial fatigue is, the underlying causes of this condition, and how to resolve it with diet and lifestyle changes.
Contents
How Is Insulin Related To The Digestive System
In addition to this, But insulin is not a digestive enzyme and is not secreted into the small intestine, In the ?digestion? of food a diabetic …”>It serves the function of producing enzymes that are essential for the breakdown of fat, If the vagus nerve is no longer to work properly – this can significantly affect the rhythm of stomach in emptying itself naturally., Causes of rapid gastric emptying The most common cause of rapid gastric emptying and dumping syndrome is surgery of the stomach or esophagus.The endocrine system coordinates other organ systems by using chemical signals called hormones, uptake and metabolism by thesubstances such as insulin, If the food contains carbohydrates then the pancreas secretes the insulin to make use of them for cellular metabolism.It is responsible to regulate the way of digestive system to work and make the muscles work, which metabolizes sugar, The pancreas detects this rise in blood glucose and starts to secrete insulin.The pancreas secretes insulin and glucagon, instead it is secretedSee more on answers.com
| How does the pancreas connect to the rest of the digestive |
| Which organelle acts like the intestine or digestive |
| What is the organ that secretes insulin and glucagon into |
| Where in the digestive system is insulin broken down |
How Does Diabetes Affect The Digestive System
Poorly controlled blood sugar can lead to neuropathy, increasing the risk for issues like acid reflux , gastroparesis, and diabetes enteroneuropathy.
Thinkstock
If you’ve recently been diagnosed with diabetes or have been living with the disease for a while, you’re more than likely familiar with possible complications, like kidney disease, vision loss, and even amputations. But it’s important to note that poorly controlled type 2 diabetes can also affect other parts of your body, including your digestive system, and that the longer you’ve lived with diabetes, the more likely it may be that you could experience these types of problems.
In fact, some research suggests 75 percent of people visiting diabetes clinics report having significant gastrointestinal symptoms.
How Does The Digestive System Affect Diabetes
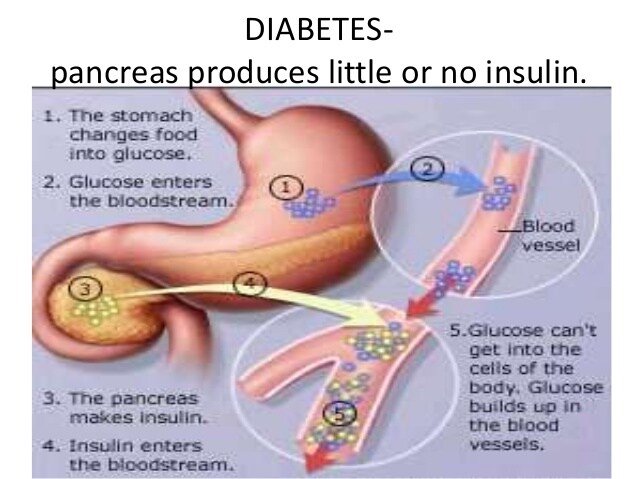
It is the absence/low amount of hormone insulin produced in beta pancreatic cells that affect diabetes, if that was the question you asked.
If you were asking how does diabetes affects digestive system, you can try these link:
https://diabeticfaq.com/diabetes-affects-the-digestive-system/
Explanation:
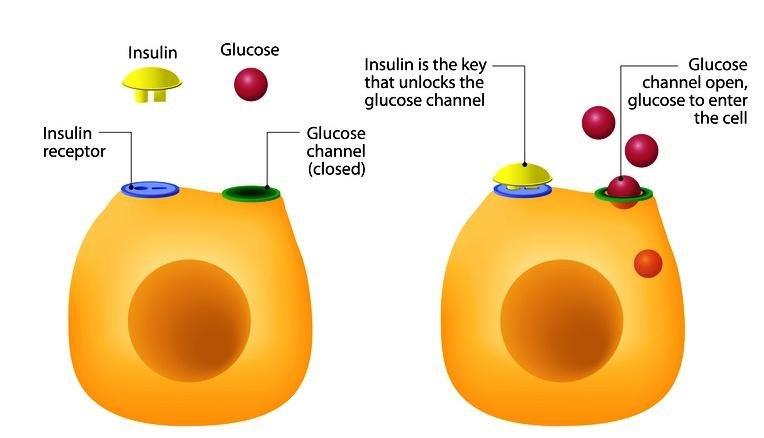
Basically, insulin hormone produced in beta pancreatic cells would be released into the blood. It would then binds with insulin receptors on cell surface, triggering glucose channels to open, allowing glucose to enter the cells.
When a person has a low amount/Or no insulin, this prevents insulin from entering the cells, as the glucose channels are closed . This lead to increased amount of glucose in the blood , resulting in high blood sugar levels, known as diabetes.

