We Know Some People Get Confused Between Type 1 And Type 2 Diabetes And Were Often Asked About The Differences Between Them
Although type 1 and type 2 diabetes both have stuff in common, there are lots of differences. Like what causes them, who they affect, and how you should manage them. There are other types of diabetes like gestational and MODY. But this page is mainly about the differences between type 1 and type 2.
For a start, type 1 affects 8% of everyone with diabetes. While type 2 diabetes affects about 90%.
Lots of people get confused between type 1 and type 2 diabetes. This can mean you have to explain that what works for one type doesn’t work for the other, and that there are different causes.
The main thing to remember is that both are as serious as each other. Having high blood glucose levels can lead to serious health complications, no matter whether you have type 1 or type 2 diabetes. So if you have either condition, you need to take the right steps to manage it.
Types Of Insulin Where To Inject It And The Best Methods For Insulin Delivery
Daphne E. Smith-Marsh PharmD, CDEW. Patrick Zeller MD
role of insulinshort- and long-term complicationsYour diabetes treatment team is there to help you. Patients’ Guide to Managing Your Child’s Type 1 Diabetes Jay Cutler’s interview with EndocrineWeb
This article will provide a basic overview of insulin. You can also visit our Patients’ Guide to Insulin for more information as well as read more in the section on Type 1 Diabetes Treatments, which has a chart providing more detail about the types of insulin that your doctor may prescribe.
Example #4: Formulas Commonly Used To Create Insulin Dose Recommendations
This example illustrates a method for calculating of your background/basal and bolus doses and estimated daily insulin dose when you need full insulin replacement. Bear in mind, this may be too much insulin if you are newly diagnosed or still making a lot of insulin on your own. And it may be too little if you are very resistant to the action of insulin. Talk to your provider about the best insulin dose for you as this is a general formula and may not meet your individual needs.
The initial calculation of the basal/background and bolus doses requires estimating your total daily insulin dose:
What Precautions Should You Take While Doing Exercise For Type 1 Diabetes
Trying any exercise that catches your interest isn’t as easy for you as the people who don’t have type 1 diabetes. You would have to consult your diabetes educator or your doctor before you start a new workout or try a new exercise routine.
Your healthcare professional may advise you to follow certain steps to prevent a drastic drop in blood sugar levels before and after exercise. These steps include:
- Decrease the amount of basal or bolus insulin before or after exercise if you’re experiencing low blood sugar levels after any physical activity.
- You can manage your sugar levels by consuming carbohydrates during or after the exercise.
- Opt for resistance activities before you go for aerobic workouts.
- You know your body well; adjust the time and intensity of exercise accordingly.
Why Do I Need Insulin Injections: How Insulin Worksand Why You Need It
Everyone needs insulin. It doesn’t matter who you are, how old you are, where you come from…you need it. Insulin is a hormone that is secreted by the islet cells in the pancreas in response to high blood glucose levels. But even in the absence of high glucose, the pancreas always releases a low level of insulin.
Insulin works on blood cells, muscle cells and fat cells to signal the cells to essentially open up and let glucose in from the bloodstream. The cells then use glucose as fuel, or energy. If there’s an excess of glucose, insulin directs the liver to store the glucose . So, when things are working as they should, the body keeps a tight rein on the amount of glucose in the blood. Someone without diabetes, for example, generally have blood sugar levels between 72 and 99 mg/dl before eating, and up to 140 mg/dl two hours after eating.
Without insulin, then, blood glucose levels become too high. Complications from high blood glucose can result: in the short-term, a serious condition called diabetic ketoacidosis can occur that, if not treated promptly, can be fatal. Longer-term, high glucose levels can lead to irreversible problems with the heart and circulatory system, the nervous system, the eyes and the kidneys.
Why Insulin Can Become Necessary For A Person With Type 2 Diabetes
Starting insulin treatment should not be seen as a setback.
People with type 2 diabetes may require insulin when their meal plan, weight loss, exercise and antidiabetic drugs do not achieve targeted blood glucose levels.
Diabetes is a progressive disease and the body may require insulin injections to compensate for declining insulin production by the pancreas. That is why starting insulin treatment should never be seen as a failure.
Starting insulin treatment should never be seen as a failure.
Treatment with insulin may be added to an antidiabetic medication or completely replace it. Regardless of the treatment, lifestyle habits are essential to managing diabetes.
Many people are reluctant to inject insulin for various reasons:
- Fear of pain or needles
- Guilt
- Impression that this is the “last resort”
- Fear of hypoglycemic attacks
- Fear of weight gain
- Memories of loved one who had to take insulin
If this is the case, do not hesitate to discuss your concerns with a health care professional. Some of your fears may be due to false beliefs. Learning more about today’s insulin treatment will probably allay your fears. For many people, insulin is an effective way to achieve good blood-sugar control, which can prevent or delay certain diabetes complications over the long term.
Type 1 Diabetes Mellitus And The Use Of Flexible Insulin Regimens
IRL B. HIRSCH, M.D., University of Washington School of Medicine, Seattle, Washington
Am Fam Physician. 1999 Nov 15;60:2343-2352.
See related patient information handout on flexible insulin regimens, provided by an AAFP staff patient education writer.
This article exemplifies the AAFP 1999 Annual Clinical Focus on the prevention and management of the complications of diabetes.
Over the past 30 years, dramatic changes have occurred in the management of type 1 diabetes mellitus .1–3 Insulin replacement strategies now stress the importance of administering smaller doses of insulin throughout the day. This approach allows insulin doses to be changed as needed to correct hyperglycemia, supplement for additional anticipated carbohydrate intake or subtract for exercise.
Although significant effort is required, it has become theoretically possible to maintain near-normal glycemia in most patients with type 1 diabetes. The 1993 report from the Diabetes Control and Complications Trial demonstrated that meticulous glycemic control is possible and reduces the occurrence of microvascular complications in patients who have type 1 diabetes.4
Addressing Concerns About Carb Restriction For Type 1 Diabetes
The most common concerns about carb-restricted diets for people with type 1 diabetes are that they are too difficult to maintain, may cause diabetic ketoacidosis , and may increase the likelihood of hypoglycemia.
Sustainability
Carbohydrate restriction is entirely doable for people with type 1 diabetes. A very-low-carb diet maybe too restrictive for some people, who may prefer to eat a more liberal low-carb diet long term.
In addition to Dr. Bernstein, there are many medical and nutrition professionals with type 1 diabetes who have been following a low-carb approach for years with impressive, often life-changing results. Here are just a few who have shared their stories:
Video: Managing type 1 diabetes with low carb with Dr. Katharine Morrison
Why Do People With Type 1 Diabetes Develop Insulin Resistance
Why do people with Type 1 diabetes develop insulin resistance despite seemingly good health overall? It’s an important question. Insulin resistance is associated with a host of negative health outcomes, including heart attack and stroke. If you have Type 1 diabetes, you cannot assume that staying fit and trim – or even maintaining excellent blood sugars – will eliminate the risks.
It has already been established that people with Type 1 diabetes tend to exhibit much higher levels of insulin resistance than expected from typical risk factors . There is something about Type 1 diabetes itself, or the way that it is treated, that itself causes insulin resistance independent of all of the usual factors that the general population is asked to look out for. This may be disheartening for those of us with T1D that seem conventionally healthy: we share a major risk factor for heart disease that “cannot be easily identified using standard clinical predictors .”
A recent study published by the American Diabetes Association represents an attempt to understand why this occurs. The authors isolated two proposed contributors to the phenomenon: hyperglycemia and iatrogenic hyperinsulinemia.
In short: injecting insulin makes your tissues insulin resistant.
Why Do Some People With Type 2 Diabetes Need To Take Insulin
Type 2 diabetes can progress with time, which means that it gets more difficult for a person’s body to regulate glucose levels. The body’s many cells become less responsive to insulin , and the specific cells in the pancreas that produce insulin make less of it . This is not necessarily related to a person’s diabetes management, and it is likely not possible to prevent.
For many people, adjusting lifestyle factors such as a reduced calorie diet and increased physical activity are key to keeping blood glucose levels stable and in a target range. Healthcare professionals may also recommend that people with type 2 diabetes take additional medications like metformin, DPP-4 inhibitors, SGLT-2 inhibitors, or GLP-1 agonists to their treatment plan to improve glucose management, reduce A1C, lose weight, or support heart and kidney health.
Glycemic Control During Serious Medical Illness And Surgery
Serious medical illness and surgery produce a state of increased insulin resistance and relative insulin deficiency. Hyperglycemia can occur even in patients without diabetes as a consequence of stress-induced insulin resistance coupled with the use of dextrose-containing IV fluids. Increases in glucagon, catecholamines, cortisol, and growth hormone levels antagonize the effects of insulin, and the alpha-adrenergic effect of increased catecholamine levels inhibits insulin secretion. Counterregulatory hormones also directly increase hepatic gluconeogenesis.
Much less is known about optimal blood glucose levels in hospitalized patients with preexisting diabetes whose hyperglycemia reflects both their diabetes and a stress response to illness. Nonetheless, it is clear that management of hospitalized patients with preexisting diabetes requires modification of treatment regimens to compensate for both the decreased caloric intake and the increased physiologic stress. Near-normal blood glucose levels should be maintained in medical and surgical patients with diabetes, for the following reasons:
-
To prevent the development of ketosis
-
To prevent electrolyte abnormalities and volume depletion secondary to osmotic diuresis
-
To prevent the impairment of leukocyte function that occurs when blood glucose levels are elevated
-
To prevent the impairment of wound healing that occurs when glucose levels are elevated
How Do Health Care Professionals Diagnose Type 1 Diabetes
Health care professionals usually test people for type 1 diabetes if they have clear-cut diabetes symptoms. Health care professionals most often use the random plasma glucose test to diagnose type 1 diabetes. This blood test measures your blood glucose level at a single point in time. Sometimes health professionals also use the A1C blood test to find out how long someone has had high blood glucose.
Even though these tests can confirm that you have diabetes, they can’t identify what type you have. Treatment depends on the type of diabetes, so knowing whether you have type 1 or type 2 is important.
To find out if your diabetes is type 1, your health care professional may test your blood for certain autoantibodies. Autoantibodies are antibodies that attack your healthy tissues and cells by mistake. The presence of certain types of autoantibodies is common in type 1 but not in type 2 diabetes.
Do I Have Other Treatment Options For My Type 1 Diabetes
The National Institute of Diabetes and Digestive and Kidney Diseases has played an important role in developing “artificial pancreas” technology. An artificial pancreas replaces manual blood glucose testing and the use of insulin shots. A single system monitors blood glucose levels around the clock and provides insulin or a combination of insulin and glucagon automatically. The system can also be monitored remotely, for example by parents or medical staff.
In 2016, the U.S. Food and Drug Administration approved a type of artificial pancreas system called a hybrid closed-loop system. This system tests your glucose level every 5 minutes throughout the day and night through a continuous glucose monitor, and automatically gives you the right amount of basal insulin, a long-acting insulin, through a separate insulin pump. You still need to manually adjust the amount of insulin the pump delivers at mealtimes and when you need a correction dose. You also will need to test your blood with a glucose meter several times a day. Talk with your health care provider about whether this system might be right for you.
The illustration below shows the parts of a type of artificial pancreas system.
Starting in late 2016 and early 2017, the NIDDK has funded several important studies on different types of artificial pancreas devices to better help people with type 1 diabetes manage their disease. The devices may also help people with type 2 diabetes and gestational diabetes.
Getting Started With Insulin If You Have Type 2 Diabetes
New to insulin? Learn about insulin dosing and timing and how often to test your blood sugar levels if you have type 2 diabetes.
If you have type 2 diabetes, it is likely that your treatment regimen will change over time as your needs change, and at some point, your healthcare professional may suggest that you start taking insulin. While this might feel scary, there are millions of others living with type 2 diabetes and taking insulin, so it’s definitely manageable.
What Happens When You Have Type 1 And Type 2 Diabetes
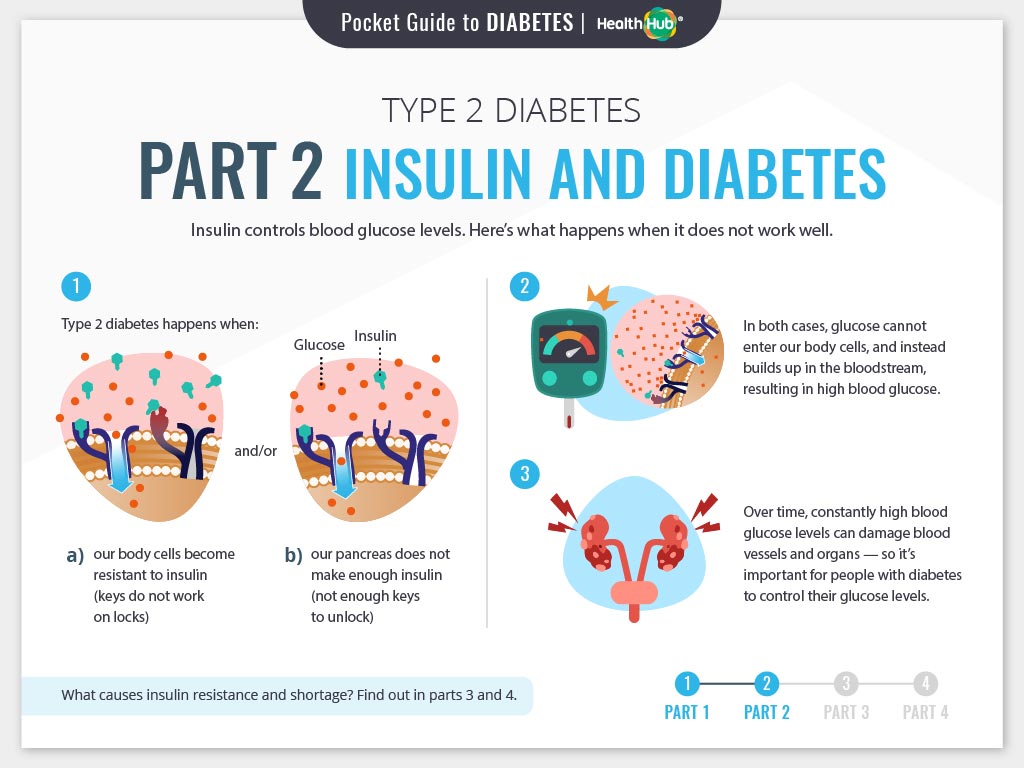
If you have either type 1 or type 2 diabetes, it means you have too much glucose in your blood. This is the same for both types. But the difference between them is how this happens.
If you have type 1 diabetes, it means you have an autoimmune condition. This means your body has attacked and destroyed the cells that make a hormone called insulin. So you can’t make insulin anymore.
We all need insulin as it helps take the glucose from our blood into our body’s cells. We then use this glucose for energy. Without insulin, the glucose level in your blood gets too high.
Type 2 diabetes is different. If you’ve got type 2, either your body doesn’t make enough insulin, or your insulin doesn’t work properly. This is known as insulin resistance. Like type 1, this means the level of glucose in your blood is too high.
What Medicines Do I Need To Treat My Type 1 Diabetes
If you have type 1 diabetes, you must take insulin because your body no longer makes this hormone. Different types of insulin start to work at different speeds, and the effects of each last a different length of time. You may need to use more than one type. You can take insulin a number of ways. Common options include a needle and syringe, insulin pen, or insulin pump.
Some people who have trouble reaching their blood glucose targets with insulin alone also might need to take another type of diabetes medicine that works with insulin, such as pramlintide. Pramlintide, given by injection, helps keep blood glucose levels from going too high after eating. Few people with type 1 diabetes take pramlintide, however. The NIH has recently funded a large research study to test use of pramlintide along with insulin and glucagon in people with type 1 diabetes. Another diabetes medicine, metformin, may help decrease the amount of insulin you need to take, but more studies are needed to confirm this. Reseachers are also studying other diabetes pills that people with type 1 diabetes might take along with insulin.
Hypoglycemia, or low blood sugar, can occur if you take insulin but don’t match your dose with your food or physical activity. Severe hypoglycemia can be dangerous and needs to be treated right away. Learn more about hypoglycemia and how to prevent or treat it.
Should You Exercise If You Have High Type 1 Diabetes
While most of the time, blood sugar levels usually drop after exercise, however, sometimes some short and intense bouts of workouts can increase your blood sugar levels. This high sugar level is due to the release of stress hormones during high-intensity or strenuous activity.
If you experience that your blood sugar level is high before you start your workout, keep checking your sugar levels frequently during the workout session and immediately after it too. Don’t dehydrate in the process; keep a water bottle or any other fluid handy to keep yourself hydrated at all times; it’s because dehydration can enhance your blood sugar concentration.
If you find your blood sugar levels high after the workout, you can have rapid-acting insulin to lower it down. If it’s an insulin pump that you use, then you can increase your basal insulin infusion but temporarily or until your sugar levels return to normal.
You’ll Need To Calculate Some Of Your Insulin Doses
You’ll also need to know some basic things about insulin. For example, 40-50% of the total daily insulin dose is to replace insulin overnight.
Your provider will prescribe an insulin dose regimen for you; however, you still need to calculate some of your insulin doses. Your insulin dose regimen provides formulas that allow you to calculate how much bolus insulin to take at meals and snacks, or to correct high blood sugars.
The Exercise You Can Do Safely With Type 1 Diabetes
According to the American Diabetes Association, adults having type 1 diabetes should at least do 150 minutes of moderate-intensity aerobic exercise per week. Examples of such activities include jogging, cycling, dancing, walking, etc.
The ADA also advises adults with type 1 diabetes to aim to complete at least 2-3 sessions of resistance activities every week. These resistance activities usually include some muscle-strengthening activities such as resistance band exercises.
Remember, different workouts will pose different effects on your body depending upon its intensity, time duration, etc. For example, your sugar levels are likely to drop after any aerobic activity. So, the longer the aerobic workout session, the more will be the more blood sugar levels will be dropped.
No matter what type of exercise or physical activity you choose to do, it’s highly crucial to check your sugar levels before and after every workout session. Coordinating between insulin intake and food consumption, you can also keep your levels optimal during physical activities.
Exercise For Type 1 Diabetes
The Emotional Impact Of Type 1 And Type 2 Diabetes
Living with type 1 or type 2 diabetes can sometimes feel overwhelming.
Both types are different but feeling down or anxious because of your diabetes can affect anyone. It is important to understand that a long-term condition can come with an emotional impact, no matter how it has been caused or how you treat it.
If you’re struggling with your diabetes, remember that you’re not alone.
There is lots of support available to you, like our helpline. There you can speak to our highly trained advisors about how you’re feeling. And you can also speak to people who are going through similar experiences on our forum. There are lots of things you can do to help yourself and it’s just about finding what works for you.
It can be frustrating to explain the differences between type 1 and type 2.
Both types face confusion over what causes the condition and how it can be treated. This will be slightly different whether you’re type 1 or the more common type 2. Just because something is more common, doesn’t mean it is understood.
And while it is emotionally draining to constantly correct people, you should also know that you’re not alone. There are many people living with diabetes facing similar questions and struggles, regardless of type. You can reach out to them to give or receive support in the forum and at local groups.
Is Diet And Exercise Enough Or Do I Need Metformin

In the past few years, the American Diabetes Association has seen changes to its guidelines related to the effectiveness of diet and exercise in managing diabetes. It is current practice to start metformin early to protect beta cells from further damage.
Metformin can lower A1C by 1-2 percent. It should be used in the treatment of Type 2 diabetes for this reason, along with its protective mechanism related to beta cells in the pancreas. Most people with diabetes will want to achieve an A1C of less than 7 percent in order to avoid the long term complications of diabetes.
Your healthcare provider will look at your A1C numbers, and determine the need for interventions, including diet, exercise, oral medications, non-insulin injectable medications for diabetes, or insulin. Generally, what happens is that a person with diabetes will do well on metformin for a number of years, and then they tend to start seeing their A1C creep up.
It becomes more difficult to keep the A1C below 7 percent with diet, exercise, and metformin. At this point, your healthcare provider may be looking at adding in a number of different oral medications for diabetes, or adding a GLP-1 injectable, and eventually insulin if A1C goal is not achieved by other means.
Some important factors that should be taken into consideration when picking a diabetes medication are:
- the costs,
- side effects , and
- the risk of a low blood sugar.4
Taking Insulin Will Interfere With Your Lifestyle
You might be thinking that once you start on insulin, you won’t be able to do the things you like to do. This is simply not true. You can travel, go out to eat, play sports, ride a bike, swim, go camping…there’s no reason that you can’t do everything that you used to do before you got diabetes. Sure, you’ll likely need to figure out logistics, such as taking your insulin with you and possibly adjusting insulin doses, but this is all doable. Meet with a diabetes educator to help you fit insulin — and diabetes — into your lifestyle. And remember that plenty people with type 1 diabetes do this every day!
When Do People With Type 2 Diabetes Start Insulin
After 10 to 20 years, many people with type 2 diabetes will begin insulin therapy, although every person’s journey with type 2 diabetes is different. This happens when lifestyle changes and medications aren’t keeping your glucose levels in your target range. It is important that you start treatment as early as possible to avoid persistent hyperglycemia , which can lead to long-term health complications affecting your heart, kidneys, eyes, and other organs.
Do Only People With Type 1 Diabetes Take Insulin
This is a very commonly asked and extremely important question. The answer is clear and simple: No. But a lot of people have the misconception that insulin treatment equals type 1 diabetes.
Type 1 diabetes doesn’t mean that you have to take insulin, it means that your body makes very little insulin. All people who have type 1 diabetes have to take insulin. But many people with type 2 diabetes need to take insulin as well. Most people with type 2 diabetes still make a lot of their own insulin, but it’s not enough to keep their blood glucose levels in the normal range. Medications other than insulin will help their bodies make more insulin or respond better to the insulin that they are making, but often they are not able to make enough insulin to meet their needs even with these other medications. When this happens, they need to go onto insulin therapy, but they still have type 2 diabetes because they are still making a lot of their own insulin.

