How Insulin Medicine Is Made
Insulin is made in different ways. You and your healthcare team will discuss which insulin you can take.
- Human insulin this is synthetic and made in a laboratory to be like insulin made in the body.
- Analogue insulin the insulin molecule is like a string of beads. Scientists have managed to alter the position of some of these beads to create genetically engineered insulin known as analogues.
- Animal insulin This isnt used much anymore, but some people find that insulin from animals works best for them. It is usually from a cow or pig.
Other Options For The Initiation Of Insulin Therapy
The recent Treating to Target in type 2 Diabetes study compared the introduction of basal insulin at bedtime to insulin initiation with either biphasic insulin twice daily or prandial insulin before meals . The biphasic and prandial insulin regimens provided better glycemic control than once-daily basal insulin but at the expense of increased risks of hypoglycemia and weight gain. Although biphasic insulin reduced A1C levels to the same extent as prandial insulin, the latter regimen was associated with the most hypoglycemic episodes and the highest weight gain . Therefore, and considering that to date there is no clinical trial evidence supporting the specific lowering of postprandial glucose levels when aiming to lower cardiovascular risk in type 2 diabetes, initiation with prandial insulin is generally not a first-choice approach when starting insulin in type 2 diabetic patients. This was confirmed by a recently reported direct comparison of once-daily insulin glargine versus thrice-daily insulin lispro in insulin-naive patients . Finally, also regarding feasibility in clinical practice and patients’ acceptance, three injections per day is the least attractive option for initiation of insulin therapy.
People With Type 2 Dont Make Insulin
This isnt true. People with type 2 diabetes may actually produce higher-than-normal levels of insulin earlier in the course of the disease, a condition known as hyperinsulinemia. This happens because type 2 diabetes is caused by insulin resistance, a condition in which the body loses the ability to respond normally to the hormone. Taking insulin shots can help overcome insulin resistance, and they can take the place of naturally occurring insulin production, which does tend to dwindle over time.
You May Like: What Happens If A Diabetic Eats Too Much Sugar
Who Gets Type 2 Diabetes
What makes people more likely to develop type 2 diabetes? No one knows for sure. But experts have a few ideas about what puts a person at greater risk:
- Most people who have type 2 diabetes are overweight.
- People with family members who have diabetes get diabetes more often.
- People who are older than 10 are more likely to develop type 2 diabetes than younger kids.
The High Blood Sugar Correction Factor:
Correction Factor = 1800 ÷Total Daily Insulin Dose = 1 unit of insulin will reduce the blood sugar so many mg/dl
This can be calculated using the Rule of 1800.
Example:
= 1800 ÷ TDI = 1 unit insulin will drop reduce the blood sugar level by 45 mg/dl
While the calculation is 1 unit will drop the blood sugar 45 mg/dl, to make it easier most people will round up or round down the number so the suggested correction factor may be 1 unit of rapid acting insulin will drop the blood sugar 40-50 mg/dl.
Please keep in mind, the estimated insulin regimen is an initial best guess and the dose may need to be modified to keep your blood sugar on target.
Also, there are many variations of insulin therapy. You will need to work out your specific insulin requirements and dose regimen with your medical provider and diabetes team.
You May Like: Adverse Effects Of Insulin
Estimation Of Global Insulin Use For Type 2 Diabetes 201: A Microsimulation Analysis
- AffiliationsCenter for Primary Care and Outcomes Research and Center for Population Health Sciences, Departments of Medicine and of Health Research and Policy, Stanford University, Palo Alto, CA, USACenter for Primary Care, Harvard Medical School, Boston, MA, USA
- Sylvia KehlenbrinkAffiliations
- Division of General Medicine, University of Michigan, Ann Arbor, MI, USACenter for Clinical Management Research, Veterans Affairs Ann Arbor Healthcare System, Ann Arbor, MI, USA
Insulin Treatment In Type 2 Diabetes
The decision to take insulin is never an easy one. For many patients, it comes after years of having type 2 diabetes and trying multiple weight-loss regimens, diets, and oral medications. For other patients, the decision to take insulin is made when blood glucose levels are simply too high to control with other drugs.
The good news is that insulin almost always works. Daily injections, however inconvenient or painful at first, can be very effective at controlling blood glucose. Anxious about giving injections? Help is available. If your health care provider prescribes insulin, a trained diabetes educator or pharmacist can teach you how to measure out the proper dose and administer your daily injections.
Why should I use insulin?
With type 2 diabetes, over time, the pancreas is often unable to produce insulin on its own. When that happens, your blood glucose levels will become very difficult to control without daily injections of insulin. Injectable insulin is identical to the insulin made by the body, but can be categorized into two main types: basal insulin keeps your blood glucose stable all day long, even when not eating, while bolus insulin helps your body respond to the quick rise in blood glucose after meals.
Don’t Miss: How Many Points Does Metformin Lower Blood Sugar
How Should Insulin Therapy Be Intensified
The available options for additional insulin injections include a second injection of basal insulin, prandial insulin before one or more meals, or a switch to biphasic insulin. The choice between intensification of basal insulin versus the introduction of prandial or biphasic insulin should be individualized based on patients’ diurnal blood glucose profiles. When considering the profiles obtained with NPH insulin or long-acting insulin analog once daily, the effect appears to wane during the day, even in patients starting insulin therapy, i.e., with remaining endogenous insulin secretion . These patients could benefit from adding a second injection of basal insulin . However, in the context of declining endogenous insulin secretion, daytime hyperglycemia is usually related to elevated postprandial glucose levels, favoring the initiation of prandial or biphasic insulin.
How To Titrate Insulin Dosage And Monitor Progress
A major feature of this regimen is that insulin is added to existing treatment. Glycaemic control should therefore improve immediately and for practical purposes, should not deteriorate. This means that the dose of insulin can be increased relatively slowly, minimising the risk of hypoglycaemia. As described originally, the regimen2 increased the insulin dosage by 4 units a day if the fasting blood glucose exceeded 8 mmol/L on three consecutive days and by 2 units a day if it exceeded 6 mmol/L. We tend to do it slightly slower and adjust insulin dosage according to these glucose thresholds every 1-2 weeks. The slower pace helps to gain the patient’s confidence and reduces the risk of hypoglycaemia. This titration regimen is of course not ‘cast in stone’ and there are ongoing trials that are exploring the best options.
After 2-3 months, the patient is likely to be on about 30 units of insulin each day and maximum oral drug therapy. Measuring the HbA1c concentration after this interval helps to quantify the new level of glycaemic control and further increases in insulin dosage can be made accordingly. There is generally a reduction in HbA1c of about 2% and an increase in body weight of several kilograms. If these changes are not evident, one should consider the possibility that the patient has not been taking the insulin regularly or someone unfamiliar with the regimen has reduced or stopped one or more of the oral hypoglycaemic drugs.
Also Check: Cellular Actions Of Insulin Could Be Inhibited By
What Is Type 2 Diabetes
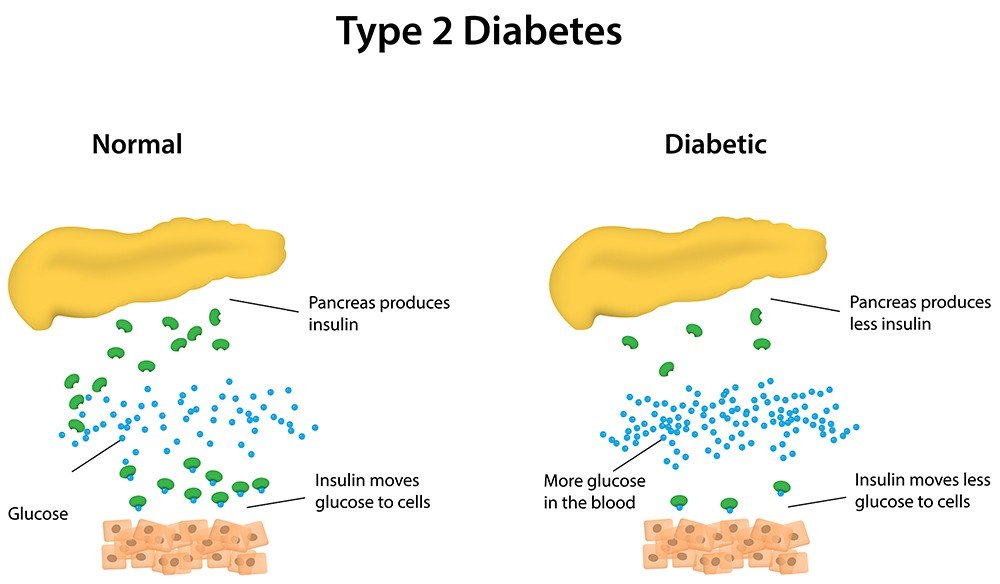
There are two major types of diabetes: type 1 and type 2. Each type causes high blood sugar levels in a different way.
In type 1 diabetes, the pancreas can’t make insulin. The body can still get glucose from food, but the glucose can’t get into the cells, where it’s needed, and glucose stays in the blood. This makes the blood sugar level very high.
With type 2 diabetes, the body still makes insulin. But a person with type 2 diabetes doesn’t respond normally to the insulin the body makes. So glucose is less able to enter the cells and do its job of supplying energy.
When glucose can’t enter the cells in this way, doctors call it insulin resistance. Although there’s plenty of insulin in the person’s body, because it doesn’t work properly, the pancreas still detects high blood sugar levels. This makes the pancreas produce even more insulin.
The pancreas may eventually wear out from working overtime to produce extra insulin. When this happens, it may no longer be able to produce enough insulin to keep blood sugar levels where they should be. In general, when someone’s blood sugar levels are repeatedly high, it’s a sign that he or she has diabetes.
p
Animal Models In Dm Type 1 Research
Animal models are used in autoimmune diabetes research to understand the pathogenesis and etiology of this disease, and to find and test predictive biomarkers and therapeutic interventions. Currently available models of T1D can be divided into spontaneously autoimmune, chemically induced, virus induced and genetically induced.
Spontaneous autoimmune
- Non-obese diabetic mouse
The NOD mouse is the best known and most widely used animal model for type 1 DM research. It is an inbred, genetically well characterized mouse strain that spontaneously develops T1D. The onset of insulitis occurs at 3â4 weeks of age. The islets of Langerhans are infiltrated by CD4+, CD8+ T lymphocytes, NK cells, B lymphocytes, dendritic cells, macrophages and neutrophils, similar to the disease process in humans. Insulitis leads to destruction of β-cells, resulting in the apparent occurrence of T1D, which varies by sex. The incidence is about 60-80% in females and 10-30% in males. In addition to sex, breeding conditions, gut microbiome composition or diet also influence the onset of T1D. NOD Mice are used to understand the pathogenesis and etiology of the disease, to identify novel autoantigens and biomarkers or to test new intervention strategies.
- BioBreeding Diabetes-Prone rat
- LEW -1AR1 / -iddm rat
Chemically induced
Genetically induced
Virally induced
Also Check: Metformin Description
Analogue Versus Human Insulin
Glucose control, adverse effects, cost, adherence, and quality of life need to be considered when choosing a type of insulin. In general, analogue insulin is similar to human insulin in controlling diabetes, although some trials have found higher mean A1C levels in patients taking analogue insulin compared with human insulin. 17 Analogue insulin usually causes less postprandial hyperglycemia and delayed hypoglycemia. 18,19 In a recent meta-analysis, glycemic control was not improved with analogue insulin compared with human insulin, but nocturnal hypoglycemia was reduced.17
An industry-funded cost-effectiveness analysis found that the increased cost of medication is more than off set by the reduction in hypoglycemic events. 20 However, the analysis assumed a cost differential of 14 percent, which is inconsistent with current pricing . 20,21 Cost-effectiveness analyses have differed regarding the long-term cost savings of using analogue insulin in patients with type 2 diabetes, with industry-sponsored studies finding reduced cost22 and government-sponsored studies finding no cost reduction. 23 Measures of adherence and quality of life have been improved with analogue insulin compared with human insulin. 24,25
What Are The Signs & Symptoms Of Type 2 Diabetes
People who have type 2 diabetes may not know it because the symptoms aren’t always obvious and they can take a long time to develop. Some people don’t have any symptoms at all.
But when a person gets type 2 diabetes, he or she may:
- pee a lot because the body tries to get rid of the extra blood sugar by passing it out of the body in the urine
- drink a lot to make up for all that peeing
- feel tired all the time because the body can’t use sugar for energy properly
Also, people whose bodies are having problems using insulin or who are overweight may notice something called acanthosis nigricans. This can cause a dark ring around the neck that doesn’t wash off, as well as thick, dark, velvety skin under the arms, in between fingers and toes, between the legs, or on elbows and knees. This skin darkening can lighten over time with improvement in insulin resistance.
In addition, girls with insulin resistance may have polycystic ovary syndrome . In PCOS, the ovaries get bigger and develop fluid-filled sacs called cysts. Girls with this condition often have irregular periods or may stop having periods, and they might have excess facial and body hair.
Read Also: Can Type 2 Diabetics Eat Bananas
When Should Insulin Therapy Be Intensified
Because of progressive -cell decline, treatment with once-daily basal insulin alone will eventually fail to maintain glycemic control in a substantial number of patients with type 2 diabetes. When the recommended A1C level of < 7.0% is not reached, or maintained despite successful basal insulin dose titration maintaining fasting plasma glucose 100 mg/dl, or when aggressive titration is limited by hypoglycemia, treatment should be intensified by adding insulin injections.
Common Questions About Type 2 Diabetes:
- Can type 2 diabetes go away?
- Will I need to take insulin?
- Do I have to take it forever?
How do you treat type 2 diabetes?
When you have type 2 diabetes, you first need to eat a healthy diet, stay physically active and lose any extra weight. If these lifestyle changes cannot control your blood sugar, you also may need to take pills and other injected medication, including insulin.
Eating a healthy diet, being physically active, and losing any extra weight is the first line of therapy. Diet and exercise is the foundation of all diabetes management because it makes your bodys cells respond better to insulin and lowers blood sugar levels.
If you cannot normalize or control the blood sugars with diet, weight loss and exercise, the next treatment phase is taking medicine either orally or by injection.
Diabetes pills work in different ways some lower insulin resistance, others slow the digestion of food or increase insulin levels in the blood stream. The non-insulin injected medications for type 2 diabetes have a complicated action but basically lower blood glucose after eating. Insulin therapy simply increases insulin in the circulation.
Many people with type 2 diabetes have elevated blood fats and blood pressure, so you may be given medications for these problems as well.
Can type 2 diabetes go away? And if my blood sugar becomes normal, do I still have diabetes?
Will I need to take insulin if I have type 2 diabetes?
Don’t Miss: What Is A High Blood Sugar Reading
How Is Type 2 Diabetes Diagnosed
Doctors can say for sure if a person has diabetes by testing blood samples for glucose. Even if someone doesn’t have any symptoms of type 2 diabetes, doctors may order blood tests to check for it if the person has certain risk factors .
Some kids and teens with diabetes may go to a pediatric endocrinologist â a doctor who specializes in diagnosing and treating children and teens living with diseases of the endocrine system, such as diabetes and growth problems.
p
Using Insulin With Oral Medications
Many oral medications are safe and effective when combined with insulin therapy. To maximize benefit without causing significant adverse effects, it is important to consider the mechanism of action for different therapies.
Insulin sensitizers have been proven safe and effective when combined with insulin therapy. 36,37 Metformin is usually continued indefinitely after the patient starts insulin therapy because it reduces cardiovascular risk in overweight patients with type 2 diabetes.12 Metformin combined with insulin is also associated with decreased weight gain, a lower insulin dosage, and less hypoglycemia compared with insulin alone. 38 Thiazolidinediones improve insulin sensitivity but may increase weight gain, fluid retention, and risk of congestive heart failure when combined with insulin.36 Thiazolidinediones also have not been shown to reduce macrovascular complications or all-cause mortality.
Alpha-glucosidase inhibitors delay absorption of carbohydrates in the gastrointestinal tract to decrease postprandial hyperglycemia. These medications are safe and effective when combined with insulin.39
Read the full article.
- Get immediate access, anytime, anywhere.
- Choose a single article, issue, or full-access subscription.
- Earn up to 6 CME credits per issue.
Also Check: Is Raisin Bran Cereal Good For Diabetics
What Happens If You Avoid Taking Your Insulin
If you have type 1 diabetes, taking insulin is essential and you cannot live without it. If you avoid taking it, your blood sugar levels can become too high and you risk developing diabetic ketoacidosis . If left untreated, DKA could be life-threatening. Thats why its important to make sure you take your insulin.
If you have type 2 diabetes and use insulin to treat your condition, you should continue to take it as prescribed. If you avoid taking it, your blood sugar levels could become too high and you may become ill. Please speak to your healthcare professional if you have any questions or concerns about taking your insulin.
Insulin is a treatment that helps manage blood sugars, so this also reduces the risk of serious long-term complications as well a shorter-term consequences. Its still important to keep going to your appointments and manage your condition with healthy lifestyle choices. Staying active and eating a healthy diet will reduce the risk of complications from your diabetes, but insulin is also an important part of your treatment.

