How Is Alcoholic Ketoacidosis Treated
Treatment for alcoholic ketoacidosis is typically administered in the emergency room. Your doctor will monitor your vital signs, including your heart rate, blood pressure, and breathing. They will also give you fluids intravenously. You may receive vitamins and nutrients to help treat malnutrition, including:
- thiamine
- phosphorus
- magnesium
Your doctor may also admit you to the intensive care unit if you require ongoing care. The length of your hospital stay depends on the severity of the alcoholic ketoacidosis. It also depends on how long it takes to get your body regulated and out of danger. If you have any additional complications during treatment, this will also affect the length of your hospital stay.
One complication of alcoholic ketoacidosis is alcohol withdrawal. Your doctor and other medical professionals will watch you for symptoms of withdrawal. If you have severe symptoms, they may give you medication. Alcoholic ketoacidosis may lead to gastrointestinal bleeding.
Other complications may include:
- pancreatitis
- pneumonia
- encephalopathy
Enhancing Healthcare Team Outcomes
Diabetes, once diagnosed, is mostly managed with changes in diet, lifestyle, and medication adherence. The goal is to prevent high glucose levels, which helps prevent diabetic complications. To prevent the complications of diabetes like ketoacidosis, the condition is best managed by an interprofessional team that includes the diabetic nurse educator, dietician, nurse practitioner, pharmacist, primary care provider, and an endocrinologist all these clinicians should educate the patient on glucose control at every opportunity.
Empowering the patient regarding management is hence of the utmost importance. Diabetes self-management education and diabetes self-management support are recommended at the time of diagnosis of prediabetes or diabetes and throughout the lifetime of the patient. DSMS is an individualized plan that provides opportunities for educational and motivational support for diabetes self-management. DSME and DSMS jointly provide an opportunity for collaboration between the patient and health care providers to assess educational needs and abilities, develop personal treatment goals, learn self-management skills, and provide ongoing psychosocial and clinical support.
The social worker should be involved to ensure that the patient has the support services and financial assistance to undergo treatment. The members of the interprofessional team should communicate to ensure that the patient is receiving the optimal standard of care.
Transition To Subcutaneous Insulin
Patients with moderate to severe DKA should be treated with continuous intravenous insulin until ketoacidosis is resolved. Criteria for resolution of ketoacidosis include a blood glucose < 200 mg/dl, a serum bicarbonate level 18 mEq/L, a venous pH > 7.3, and a calculated anion gap 12 mEq/L. The criteria for resolution of HHS include improvement of mental status, blood glucose < 300 mg/dL, and a serum osmolality of < 320 mOsm/kg.
When these levels are reached, subcutaneous insulin therapy can be started. If patients are able to eat, split-dose therapy with both regular and intermediate-acting insulin may be given. It is easier to make this transition in the morning before breakfast or at dinnertime.
Patients with known diabetes may be given insulin at the dosage they were receiving before the onset of DKA. In patients with newly diagnosed diabetes, an initial insulin dose of 0.6 unit/kg/day is usually sufficient to achieve and maintain metabolic control. Two-thirds of this total daily dose should be given in the morning and one-third in the evening as a split-mixed dose. If patients are not able to eat, intravenous insulin should be continued while an infusion of 5% dextrose in half-normal saline is given at a rate of 100200 mL/h.
Recommended Reading: How Many Points Does Metformin Lower Blood Sugar
What Should I Do
If you have any of the above symptoms, the first thing to do is to check your blood glucose.
If your blood glucose is higher than 15 mmol/L , you should test for blood ketones.A ketone level of under 0.6 is normal.If your ketone level is 0.61.5 this is a warning sign that you are starting to produce ketones. Anything higher than 1.5 and you are at risk of diabetic ketoacidosis. Your local diabetes care team may have advised of slightly different glucose levels so if you are in any doubt about when you should test for ketones, please speak to your team directly.
When should I seek help?
- If you are unwell and feel like you need some support you should contact your diabetes care team. If you cannot contact them, you can phone your GP or an out-of-hours service.
- If your ketones are over 1.5 you should contact your on-call diabetes doctor or diabetes specialist nurse, or call an out-of-hours service. You should never feel that you are bothering medical staff unnecessarily its much easier to deal with high blood glucose levels and small amounts of ketones if found early, rather than leaving it until you feel very unwell and need more intensive treatment.
- If you have any level of ketones and are feeling sick, are vomiting, have stomach pains or are feeling drowsy you should go to your nearest A& E department immediately.
The Sick Day Guidance Flowchart gives clear guidance on what to do if ketones are raised.
Treating High Blood Sugar Levels
Treating high blood sugar levels involves correcting the underlying cause. The diabetes health care team will give you specific advice on how to keep your childs blood sugar levels in a healthy range, but here are some suggestions for managing some causes of hyperglycemia:
| Underlying Cause | What to Do |
| Not getting enough insulin or other diabetes medication |
|
| Not following the meal plan |
|
| Not getting enough exercise |
|
| Illness or stress |
|
| Use of medications that increase blood sugar |
|
Read Also: What Is The Lowest Dose Of Metformin
How Can You Care For Diabetic Ketoacidosis At Home
Home care is generally directed toward preventing diabetic ketoacidosis and treating moderately to elevated to high levels of blood sugar. If you have type 1 diabetes, you should monitor your blood sugars as instructed by your healthcare proffesional. Check these levels more often if you feel ill, if you are fighting an infection, or if you have had a recent illness or injury.
Your health care professinal may recommend treating moderate elevations in blood sugar with additional injections of a short-acting form of insulin. Working with their health care practitioner, people with diabetes should have previously arranged a regimen of extra insulin injections and more frequent blood glucose and urinary ketone monitoring for home treatment as blood sugar levels begin to rise. Be alert for signs of infection and keep yourself well hydrated by drinking sugar free fluids throughout the day.
Major Syndromes Of Dka
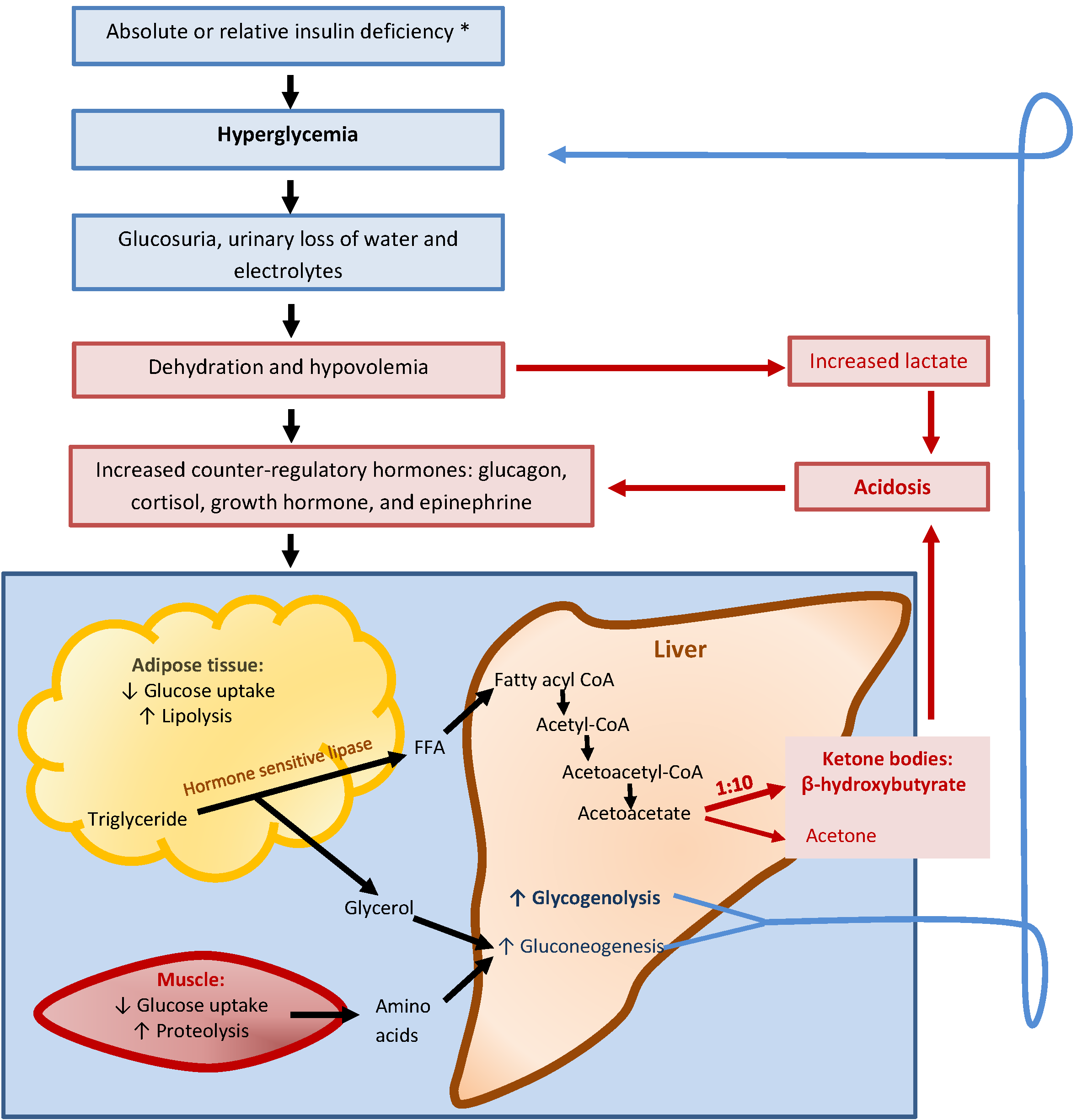
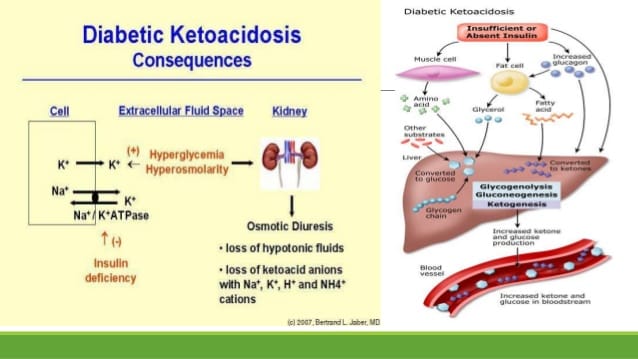
The term diabetic ketoacidosis literally explains what the patient is experiencing. The term diabetes is often thought of as dealing with a glucose derangement or imbalance. However, this is not true. Diabetes simply means an increase in urine output. Thus, diabetic in DKA implies an increase in urine output that occurs from osmotic diuresis.The term ketoacidosis is fairly self explanatory. It refers to the metabolic acidosis resulting from ketone production from fat metabolism. The DKA patient is therefore prone to metabolic acidosis from:
These three pathophysiologic syndromes produce the signs and symptoms exhibited by the patient.
You May Like: Signs Of Hyperglycemia In Adults
Dka Emergency Care And Management
As with any patient in the prehospital environment, ensure an adequate airway, ventilation, oxygenation and circulation. Based on the physiologic syndromes of osmotic diuresis leading to dehydration, ketoacidosis and electrolyte disturbances the primary goal of prehospital treatment of a DKA patient is rehydration with isotonic fluids. Normal saline is an acceptable fluid. Administer the normal saline based on the blood pressure and other indicators of tissue perfusion. It would be acceptable to bolus the fluid in cases of severe hypovolemia and hypotension. Also be sure to place the patient on a continuous cardiac monitor and obtain and record the blood glucose level. Continuously reassess the patient for improvement or deterioration.By understanding the pathophysiology of diabetic ketoacidosis, you should be better prepared to recognize the clinical presentation more promptly, differentiate the condition from other diabetic emergencies and have a good foundation for understanding the emergency care necessary to manage the patient effectively.References
- Dalton AL, Limmer D, Mistovich JJ, Werman HA. Advanced Medical Life Support: A Practical Approach to Adult Medical Emergencies, 3nd edition. Upper Saddle River, NJ: Prentice Hall, 2007.
- Guyton, A.C., and J.E. Hall. Textbook of Medical Physiology. 10th ed. Philadelphia: W.B. Sauders, 2001.
Request product info from top Ambulance Disposable Supplies companies
Thank You!
How Can Diabetic Ketoacidosis Be Prevented
- If you have diabetes take all of your medications as prescribed by your health-care professional.
- Learn to recognize the symptoms of elevated blood glucose levels.
- Don’t skip insulin doses .
- Test your glucose levels regularly as recommended by your doctor.
- Test your urine at home, especially when you feel ill. This will help detect ketones or elevated sugar in the blood, which should alert you to the possibility of diabetic ketoacidosis.
- Make an appointment with your health-care professional when you feel sick or if your sugar or ketone levels are higher than normal to prevent further worsening or development of diabetic ketoacidosis.
Recommended Reading: How Much Pasta Can A Diabetic Eat
Follow Up: Complications And Discharge
Hypoglycemia and hypokalemia are the most frequent complications and can be prevented by timely adjustment of insulin dose and frequent monitoring of potassium levels.
Non-anion gap hyperchloremic acidosis occurs due to urinary loss of ketoanions which are needed for bicarbonate regeneration and preferential re-absorption of chloride in proximal renal tubule secondary to intensive administration of chloride-containing fluids and low plasma bicarbonate. The acidosis usually resolves and should not affect treatment course.
Cerebral edema is reported in young adult patients. This condition is manifested by appearance of headache, lethargy, papillary changes, or seizures. Mortality is up to 70%. Mannitol infusion and mechanical ventilation should be used to treat this condition.
Rhabdomyolysis is another possible complication due to hyperosmolality and hypoperfusion.
Pulmonary edema can develop from excessive fluid replacement in patients with CKD or CHF.
Discharge planning should include diabetes education, selection of appropriate insulin regimen that is understood and afforded by the patient, and preparation of set of supplies for the initial insulin administration at home.
What Are The Treatment Guidelines For Diabetic Ketoacidosis
Fluid replacement and insulin administration intravenously are the primary and most critical initial treatments for diabetic ketoacidosis. These therapies together reverse dehydration, lower blood acid levels, and restore normal sugar and electrolyte balance. Fluids must be administered wisely – not at an excessive rate or total volume due to the risk of brain swelling . Potassium is typically added to IV fluids to correct total body depletion of this important electrolyte.
Insulin must not be delayed and must be given promptly as a continuous infusion to stop further ketone formation and to stabilize tissue function by driving available potassium back inside the body’s cells. Once blood glucose levels have fallen below 300mg/dL, glucose may be co-administered with ongoing insulin administration to avoid the development of hypoglycemia .
People diagnosed with diabetic ketoacidosis are usually admitted into the hospital for treatment and may be admitted to the intensive care unit.
Some people with mild acidosis with modest fluid and electrolyte losses, and who can reliably drink fluid and follow medical instructions can be safely treated and sent home. Follow-up must be available with a health care practitioner. Individuals with diabetes who are vomiting should be admitted to the hospital or urgent care center for further observation and treatment.
Also Check: Diabetes Meaning
Diabetic Ketoacidosis: Evaluation And Treatment
This is a corrected version of the article that appeared in print.
DYANNE P. WESTERBERG, DO, Cooper Medical School of Rowan University, Camden, New Jersey
Am Fam Physician. 2013 Mar 1 87:337-346.
This version of the article contains supplemental content.
Patient Information: A handout on this topic is available at .
Diabetic ketoacidosis continues to have high rates of morbidity and mortality despite advances in the treatment of diabetes mellitus. In a study of 4,807 episodes of DKA, 14 percent occurred in persons older than 70 years, 23 percent in persons 51 to 70 years of age, 27 percent in persons 30 to 50 years of age, and 36 percent in persons younger than 30 years.1 In a second study of 28,770 persons younger than 20 years with diabetes, 94 percent had no episodes of DKA, 5 percent had one episode, and 1 percent had at least two episodes.2 Additionally, DKA occurred more often in females, in persons with a migration background, and in persons 11 to 15 years of age.2 DKA has a case fatality rate of 1 to 5 percent.3,4 Although the highest rate of mortality is in older adults and persons with comorbid conditions, DKA is the leading cause of death in persons younger than 24 years with diabetes, most often because of cerebral edema.1,4
Success Steps For Diagnosing Altered Level Of Consciousness
Focus on assessing and treating the patient’s basic life threats before interrogating bystanders or investigating the scene
Unlike hypoglycemia, where the insulin level is in excess and the blood glucose level is extremely low, DKA is associated with a relative or absolute insulin deficiency and a severely elevated blood glucose level, typically greater than 300 mg/dL. Due to the lack of insulin, tissue such as muscle, fat and the liver are unable to take up glucose. Even though the blood has an extremely elevated amount of circulating glucose, the cells are basically starving. Because the blood brain barrier does not require insulin for glucose to diffuse across, the brain cells are receiving more than an adequate amount of glucose. Basically, the general body tissue is starving while the brain has more than an adequate supply of glucose. Thus, the patient does not experience the sudden onset of signs and symptoms associated with hypoglycemia.
There are three major pathophysiologic syndromes associated with an excessively elevated blood glucose level in DKA:
Recommended Reading: How Long Does It Take To Lower Blood Sugar
How Do I Prevent Diabetic Ketoacidosis From Happening Again
Diabetic ketoacidosis is life-threatening, so preventing it is important. The most important step in prevention is ensuring proper insulin dosing. The importance of home-monitoring of blood glucose levels cannot be overemphasized. If you are not yet performing home blood glucose monitoring, your veterinary healthcare team can help get you started. The necessary blood sample is tiny – just a tiny drop of blood – and the tiny needle that is used will not hurt your dog. Most dogs barely notice the pin-prick.
Your veterinarian will guide you on how often to take readings, when to report the results to the practice, and will explain how the values are interpreted in order to make decisions about modifying your dog’s insulin dose.
“The importance of home-monitoring of blood glucose levels cannot be overemphasized.”
If you are already doing home monitoring of your dog’s blood glucose levels, your veterinarian will guide you as to how often to check glucose levels once your dog returns home. The key to preventing a recurrence of diabetic ketoacidosis is to be very aware of your dog’s glucose levels both throughout the day, as well as the pattern of his blood glucose levels over the span of several days to several weeks. As you report the glucose levels, your veterinarian will be able to help you fine- tune your dog’s insulin doses and set the stage to prevent this crisis from recurring.
What Is Diabetic Ketoacidosis
Diabetic ketoacidosis, also referred to as simply ketoacidosis or DKA, is a serious and even life-threatening complication of type 1 diabetes. DKA is rare in people with type 2 diabetes. DKA is caused when insulin levels are low and not enough glucose can get into the body’s cells. Without glucose for energy, the body starts to burn fat for energy. Ketones are products that are created when the body burns fat. The buildup of ketones causes the blood to become more acidic. The high levels of blood glucose in DKA cause the kidneys to excrete glucose and water, leading to dehydration and imbalances in body electrolytelevels.
Diabetic ketoacidosis most commonly develops either due to an interruption in insulin treatment or a severe illness, including the flu.
You May Like: Which Pancreatic Cells Release Insulin And Glucagon
Which Type Of Doctors Treat Diabetic Ketoacidosis
Patients with diabetic ketoacidosis usually needs to be treated at the hospital. The person will receive treatment at first by an emergency medicine specialist and once admitted to the hospital by an internist, family medicine specialist or intensivist. Endocrinologists are physicians specializing in the endocrine system and diabetes, and often will be involved in the patient’s medical care.
What Causes Alcoholic Ketoacidosis
Alcoholic ketoacidosis can develop when you drink excessive amounts of alcohol for a long period of time. Excessive alcohol consumption often causes malnourishment .
People who drink large quantities of alcohol may not eat regularly. They may also vomit as a result of drinking too much. Not eating enough or vomiting can lead to periods of starvation. This further reduces the bodys insulin production.
If a person is already malnourished due to alcoholism, they may develop alcoholic ketoacidosis. This can occur as soon as one day after a drinking binge, depending on nutritional status, overall health status, and the amount of alcohol consumed.
- ulcers
- ethylene glycol poisoning
These conditions have to be ruled out before a medical professional can diagnose you with alcoholic ketoacidosis.
Read Also: Side Effects Of Taking Insulin

