How To Take Long
Usually, you inject long-acting insulin once a day to keep your blood sugar levels steady. You use a needle or pen device to give yourself the injection. Be sure to inject your long-acting insulin at the same time every day to avoid lags in insulin coverage or stacking your insulin doses. Stacking means taking your doses too close together, causing their activity to overlap.
Your doctor might recommend adding short-acting insulin before a meal to prevent a blood sugar spike after you eat.
If you change brands of long-acting insulin, you may need a different dose. Talk to your doctor for advice if you change brands of any insulin.
As with any medicine you take, insulin injections can cause side effects.
One possible side effect is low blood sugar . Symptoms of low blood sugar include:
- dizziness
- headache
- fainting
Other possible side effects of insulin injections include pain, redness, or swelling of the skin at the injection site.
Sometimes insulin is given in combination with thiazolidinediones. This drug group includes oral diabetic drugs like Actos and Avandia. Taking insulin with thiazolidinediones increases the risk of fluid retention and heart failure.
For those taking degludec, precautions may be necessary because of its long effect in the body. You doctor may need to increase your dose at a very gradual rate, at least three to four days apart. It will also take longer to clear the drug from your body.
Injections Via Pen Or Syringe
This method has been around the longest, since the discovery of insulin in 1921 by Frederick Banting and Charles Best.
Insulin is injected subcutaneously in one of many injection sites on the body: abdomen, thighs, upper arms, or butt. This can be done with a pre-filled insulin pen or by using a syringe to draw up the desired amount of insulin from a traditional vial. Typically, users will need a long-acting basal insulin paired with a rapid-acting insulin for mealtimes.
While insulin pens and syringes cannot offer the extremely precise measured doses a pump or pod can administer, they are certainly the most affordable method of insulin delivery. For those who dont like the bulk of wearing a pump or pod, using a pen or syringe can be just as an effective way of managing blood sugars.
Where Can I Find Help Acquiring Or Paying For Insulin
The ADA has a dedicated page for helping people who need insulin get it, regardless of finances: .
JRDF has a page with a variety of links to organizations who also supply insulin assistance:
Also Check: Can A Diabetic Drink Red Wine
Treating An Overdose Of Rapid
How you treat an overdose will depend on how quickly you realise the error.
If the insulin was administered more than 20 minutes ago, act quickly and take a good source of fast-acting carbohydrate immediately, such as glucose tablets or a very sugary drink. Follow this up with sufficient slower-absorbed carbohydrate, such as bread, to prevent hypoglycemia occurring later.
If you realise an error has been made within 20 minutes of injecting, you may not need to take sugar but you should have carbohydrate that will get absorbed relatively quickly. Avoid having fatty foods, if possible, as fat tends to slow down how quickly the carbohydrate acts.
It is common to need 10g of carbohydrate to counteract each unit of insulin. Its generally safer to have too much than too little carbohydrate when treating an overdose of insulin.
Test your blood glucose levels regularly and be on the lookout for symptoms of a hypo. If you feel hypo symptoms, or think you feel them, perform a blood test.
If the overdose is a large overdose, take carbohydrate first and then call your health team or out- of-hours service for advice.
What About People With Type 1 Diabetes
You might be wondering, Why dont human insulins work as well for people with type 1 diabetes?
Think of it this way: Type 1 diabetes and type 2 diabetes are two different diseases with different causes, and therefore should be treated differently. People with type 1 dont produce insulin at all, while those with type 2 dont respond to insulin or dont produce insulin as effectively as the average person. Type 1 is an autoimmune disease, and type 2 is a result of different genetic and lifestyle factors.
Type 1 patients must take insulin so their bodies are able to process glucose from food. For type 2 patients, insulin is just one of several lifestyle and medication changes to help manage their condition. Because of this, type 2 patients may be less sensitive to insulin changes.
Don’t Miss: Symptoms Of High And Low Blood Sugars
What Was Our Selection Criteria For The 3 Best Diabetes Programs
Factors That Affect Absorption
Factors That Affect Time of Absorption
Considerations for Administration
- Some obese patients may require larger insulin doses due to fewer numbers of peripheral receptor sites.
- Cachectic patients may be very insulin sensitive.
- Certain co-existing endocrinopathies, such as acromegaly and Cushings disease, can increase dosage requirements.
Read Also: Which Pancreatic Cells Release Insulin And Glucagon
Factors That Speed Insulin Absorption
Variation in insulin absorption can cause changes in blood glucose levels. Insulin absorption is increased by:
- injecting into an exercised area such as the thighs or arms
- high temperatures due to a hot shower, bath, hot water bottle, spa or sauna
- massaging the area around the injection site
- injecting into muscle this causes the insulin to be absorbed more quickly and could cause blood glucose levels to drop too low.
How Do You Treat Type 2 Diabetes
With the onset of type 2 diabetes and even pre-diabetes, the recommendation is to start with being more active, eating a more balanced diet, and losing weight. Then, the first-line medication treatment is metformin, which reduces how much glucose the liver releases throughout the day, lowers how much glucose is absorbed from food, and improves the bodys sensitivity to insulin. Other commonly prescribed medications like sulfonylureas and meglitinides help the pancreas make more insulin.
Insulin is not always necessary to treat type 2 diabetes, and was traditionally only prescribed in later stages of the condition. But now, some doctors believe that insulin should be used sooner by type 2 patients for better glycemic control earlier on. However, patients should still aim to improve the bodys response to insulin, as large injections of insulin over time can lead to injection site reactions, weight gain, and high blood pressure.
Again, the difference here is that type 2 patients can usually produce some insulin on their own, while type 1 patients dont produce any at all and thus depend on insulin injections throughout the day. Because insulin is so fundamental to type 1 patients surviving day to day, more advanced insulin analogs are much more beneficial than human insulins due to their predictability and ability to more closely replicate natural insulin production in the body.
Note: All insulin timelines based on .
Also Check: Diabetic Medication Side Effects
What Are Newer Insulins
Newer insulins refer to insulin analogsessentially, human insulins whose proteins have been tweaked to change how quickly the insulin gets absorbed. Insulin analogs were introduced in the late 90s.
Bolus insulin analogs, or rapid-acting insulins, are absorbed into the bloodstream more quickly than human, short-acting insulins. Taken only 15 minutes before a meal, they peak in 1 2 hours, half the time it takes for human insulins. Because of this sharper peak, they offer more flexibility in routine: You can have an earlier or later meal and adjust injection times accordingly.
On the flip side, long-acting insulin analogs more closely mimic natural basal or background insulin profiles than intermediate-acting insulins as they have a short onset, no real peak, and stay at a steady level for a very long time. They are generally more stable and more predictable than intermediate-acting insulins, and require fewer injections throughout the day.
Rapid-acting insulin brands include Humalog and Novolog, and long-acting insulin brands include Lantus and Levemir. Then theres Tresiba, an ultra long-acting insulin, and Toujeo, which is the same insulin as Lantus, only three times more concentrated. They are both designed to last much longer than other basal insulins, so in theory, youll need a smaller dose each day.
Is Newer Always Better
Newer insulin analogs were developed so patients could worry less about mealtime planning without sacrificing glucose control. Such innovations deserve a higher price tag, but are they absolutely necessary? The JAMA study says maybe not.
Though a more flexible schedule may mean a higher quality of life for some patients, the reality is that many Americans cannot afford these insulins. As the study suggests, older, more cost-efficient insulins may lead to better treatment adherence and overall better health outcomes because people are actually filling and taking their medications as prescribed. After all, you cant take a medication if you dont have the money to purchase it.
There are a couple of other financial considerations. For one, fewer senior participants in the study reached the Medicare coverage gap, or donut hole, since they paid less for the older insulin. However, the relatively unpredictable nature of older insulins should be managed with more frequent testing, which translates to more money spent on test strips.
Also Check: Skinny Diabetics
Insulin Analogs Are Now Replacing Human Insulin In The Us
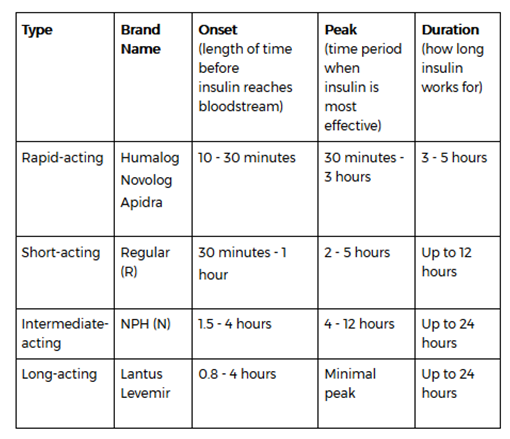
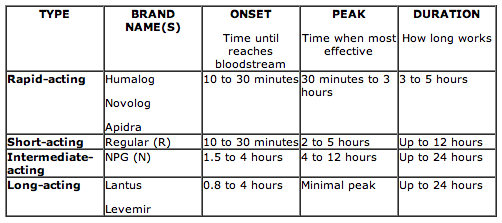
Insulins are categorized by differences in onset, peak, duration, concentration, and route of delivery.
Human Insulin and Insulin Analogs are available for insulin replacement therapy. Insulins also are classified by the timing of their action in your body specifically, how quickly they start to act, when they have a maximal effect and how long they act.Insulin analogs have been developed because human insulins have limitations when injected under the skin. In high concentrations, such as in a vial or cartridge, human clumps together. This clumping causes slow and unpredictable absorption from the subcutaneous tissue and a dose-dependent duration of action . In contrast, insulin analogs have a more predictable duration of action. The rapid acting insulin analogs work more quickly, and the long acting insulin analogs last longer and have a more even, peakless effect.
Matching Insulin And Food
In addition to understanding an insulins action curve, its important to understand how the food you eat affects your blood glucose level so that you can match your insulins action to the expected rise in blood glucose level following a meal. In general, people with normal stomach emptying can expect some glucose from the carbohydrate theyve eaten to start raising their blood glucose level within minutes of starting to eat. Blood glucose level tends to peak about one to two hours after the start of a meal and gradually drops over the next three hours.
Some other factors that may cause insulin action to differ from the action curve given in product literature or to vary from person to person include thickness of the subcutaneous fatty layer at an injection site, temperature, blood flow, exercise, and dose size. Injecting into areas that have more subcutaneous fat tends to slow insulin absorption. Widened blood vessels allow insulin to be absorbed more quickly constricted blood vessels can cause slower absorption. Large doses of insulin may also be absorbed somewhat more slowly than smaller doses.
Recommended Reading: Normal A1c Range For Type 2 Diabetes
What Is Onset Peak And Duration Of Insulin
4.3/5Insulinonsetpeakdurationfull answer
Onset is defined as the length of time insulin hits your bloodstream and begins to lower blood glucose. Peak is the time during which insulin is at its peak or maximum effectiveness at lowering blood glucose. Duration is the length of time insulin continues to lower blood glucose.
Additionally, does long acting insulin have a peak? Long–acting insulin does not have a peak time. It works to regulate blood sugar levels at a fairly stable rate throughout the day.
People also ask, which insulin has the shortest onset peak and duration?
Continued
| Type of Insulin & Brand Names | Onset |
|---|---|
| Short-Acting |
Which type of insulin acts most quickly?
The three rapid-acting insulins currently approved by the US Food and Drug Administration lispro, aspart , and glulisine have similar action curves, with an onset occurring in 515 minutes, a peak in 45 90 minutes, and an overall duration of about 34 hours.
Here Are A Few Common Types Of Insulin You Ought To Know About
Insulin is a hormone that the body produces to metabolize glucose. For both type 1 and type 2 diabetes, patients may require insulin therapy to make up for their bodys requirements for the hormone.
Insulin can be administered through injections, intravenous fluids or insulin pumps. In fact, insulin pumps are becoming popular for diabetes treatment. Here are a few common types of insulin used by diabetic patients.
Types of insulinThere are many different types of insulin based on how fast they begin to act inside the body and the duration of their effect in the body. Insulin categories can also be based on how they are derived.
Based on speed
Based on form
- Animal insulin: Derived from animals.
- Human insulin: Made in laboratories.
- Analogue insulin: Lab-grown but modified with different onset and constant times.
Human and analog insulin types are now used for the treatment of both type 1 and type 2 diabetes. Insulin can be injected through syringes and pens, can be administered through intravenous methods under medical supervision or taken in through insulin pumps. Your treatment plan can determine the type of insulin, its dose, and the administration method.
You May Like: High Sugar Symptoms Treatment
What Are The Different Types Of Insulin
The American Diabetes Association characterizes insulin by how fast it works. But everyones body is different. If you have diabetes, you should expect deviations in the amount of time any medication takes to reach your bloodstream.
Here are 8 different types of Insulin and how they work.
- Onset is defined as the length of time before insulin hits your bloodstream and begins to lower blood glucose.
- Peak is the time during which insulin is at its maximum effectiveness at lowering your blood glucose levels.
- Duration is the length of time insulin continues to lower your blood glucose levels.
- Rapid-acting insulin begins to affect blood glucose approximately 15 minutes after injection. It peaks in about an hour, and then continues to work for a few more.
- Short-acting insulin reaches your bloodstream within 30 minutes of injection. It peaks in the 2-3-hour range and stays effective for 3-6 hours.
- Intermediate-acting insulin includes NPH insulin which helps control glucose for 10-12 hours. A protamine is a type of protein that slows the action of this insulin.
- Long-acting insulin enters the bloodstream 1-2 hours after injection and may be effective for as long as 24 hours. An advantage to long-acting insulin is there is no pronounced peak, and it works more like typical pancreatic insulin.
- Premixed/combination insulin contains a mix of rapid- or short-acting insulin combined with an intermediate-acting insulin. This eliminates the need to draw insulin from more than one bottle.
What Else Can I Do To Control My Blood Glucose Levels
Food, sleep, and exercise are all of vital importance for regulating your blood sugar when you have diabetes.
Also Check: Metformin Dosage When To Take
What Can Cause An Insulin Overdose
Insulin overdoses can occur for a number of reasons. Some common reasons are listed below:
- Miscalculating the carb content of a meal
- Missing out or delaying a scheduled meal or snack after having injected
- Accidentally injecting twice for the same meal or snack
- Accidentally injecting the dosage number of a different meal
- Accidentally injecting the wrong insulin for example injecting your rapid acting insulin instead of your long acting insulin
- Having difficulty seeing the numbers or gradation on an insulin pen or syringe

