History And Clinical Examination
History and clinical examination occasionally yield useful diagnostic clues. A history of lithium therapy may raise the possibility of NDI, whereas previous brain injury or neurosurgical intervention may indicate CDI. A careful family history is important, not only to identify members of rare kindreds with inherited DI, but also to identify autoimmune endocrine disease, which could suggest autoimmune CDI. Erectile dysfunction, menstrual disturbances and fatigue may be clinical manifestations of hypopituitarism. Examination is usually normal, but clinical signs of hypogonadism, such as loss of body hair and atrophy of sexual secondary characteristics, could indicate pituitary disease and loss of temporal visual fields would raise the possibility of an intracranial tumour, most likely a craniopharyngioma.
The first step in diagnosis is to confirm the presence of hypotonic polyuria. Approximately 15% of patients referred for investigation of polyuria have normal urine volume, but present with urinary frequency, due to infection, prostatism or irritable bladder. In an adult patient, if the daily urine volume is <2.5Â L, no further investigations of osmoregulatory function are required, though urological referral may be indicated.
The Arginine Stimulation Test
Recent data revealed the amino acid arginine as another stimulator of the posterior pituitary . Arginine is an endogenous precursor to nitric oxide, an important signalling molecule in several endocrine pathways, and is used in clinical practice as a standard test for stimulating growth hormone . The current prospective study included 92 healthy adults and children and 96 patients with polyuriaâpolydipsia syndrome . The arginine infusion led to a rise in the median copeptin levels from 5.2Â pmol/L to 9.8Â pmol/L in the healthy participants. Meanwhile, a copeptin level of 3.8Â pmol/L taken 60Â min after start of the infusion had a high diagnostic accuracy of 93% to distinguish the 38 central DI from the 58 PP patients. Another advantage of the arginine infusion test is that it is well-tolerated, with adverse effects mainly involving mild nausea. If a patient experiences severe nausea or vomiting, test results should be interpreted with caution as vomiting is a potent trigger for AVP/copeptin release.
In summary of the above-mentioned tests, it can be said that copeptin measurement has become an important biomarker for the diagnosis of DI. Whilst basal copeptin measurement easily diagnoses nephrogenic DI, two copeptin stimulation tests with a high diagnostic accuracy are available to differentiate central DI from PP patients.
What Is The Difference Between Diabetes Insipidus And Diabetes Mellitus
Diabetes insipidus should not be confused with the much more common type of diabetes called diabetes mellitus. The two conditions are not related. Diabetes mellitus can also make you feel thirsty and pass lots of urine. It occurs when the level of sugar in your blood becomes higher than normal. In diabetes insipidus, there is no problem with the level of glucose in your blood. See the separate leaflets called Type 1 Diabetes and Type 2 Diabetes for more details.
Find Out Your Personal Necessities Regarding The Result Offering
We possess secure requirements for a result before we purchase it. As I mentioned on top, there are some circumstances where even the supplements for diabetes insipidus would not include all the characters you are spot. So, before buying any, I suggest you discovered a list of necessities and created sure that the choice you possess picked has it.
What Are The Symptoms Of Diabetes Insipidus
The following are the most common symptoms of diabetes insipidus. However, each individual may experience symptoms differently. Symptoms may include:
- excessive thirst
- excessive urine production
- dehydration
The symptoms of diabetes insipidus may resemble other conditions or medical problems. Always consult your physician for a diagnosis.
What Happens If You Have Diabetes Insipidus
The main symptoms of diabetes insipidus include:
- Passing large volumes of urine. You may find that you can pass somewhere between 3 and 20 litres of urine per day.
- Passing urine frequently during the day.
- Getting up to pass urine frequently during the night.
- Feeling excessively thirsty, despite the fact that you seem to be drinking lots of fluids.
- A lack of fluid in your body . This can become a problem if you do not drink enough fluids to compensate for the amount of urine that you are passing. Severe dehydration is a medical emergency and immediate medical attention is needed.
- Symptoms of dehydration can include:
- Headaches.
- Confusion.
- in severe cases, collapse.
- Tiredness and reduced concentration. This may be due to lack of sleep because of repeated night-time trips to the toilet.
Poor growth and weight loss may be noticed in babies with diabetes insipidus. They may also appear irritable and difficult to settle. Older children may have problems with bedwetting at night and also incontinence of urine during the daytime. They may also have poor growth and a loss of appetite, as well as tiredness.
Forums Facebook Groups Instagram Reddit
Some of the best practice to identify a good result without doing a many research is to join on communities regarding supplements for diabetes insipidus. You can easily go to and type in: “supplements for diabetes insipidus” and access the groups category.
Other ways, you can find active forums regarding the trade you are catch, create a profile and post a inquiry. You’d be surprised to possess discovered a abounding insightful information by visiting diffrent threads.
Reddit is a social media website including a lot of operating consumer, you can simply go to a subreddit correlated to supplements for diabetes insipidus you’re getting and publish a post there, many community including years of judgment would help you choose the right choice.
Estrodiol Testosterone Sex Hormone Binding Globulin
These should be assessed early morning and in the early follicular phase and off the contraceptive pill in women.
Sex hormone binding globulin is necessary to calculate free androgen index in some cases, for example where the decision to start testosterone replacement is not clear cut.
Further investigations – selected cases only
There Are Various Forms Of Diabetes Insipidus
- Neurogenic – the brain doesn’t produce enough of the hormone vasopressin. Some of the events that could cause this form of diabetes insipidus include head injury, infection , brain tumour, ruptured aneurysm or brain surgery. In about half of cases, the cause remains unknown .
- Nephrogenic – the kidneys aren’t sensitive to vasopressin and fail to respond. This comparatively rare form of diabetes insipidus is caused by an inherited disorder that affects the tubules, the tiny structures inside the kidneys that absorb water. Men are more prone to this condition than women. In adults nephrogenic diabetes insipidus can be caused by treatment with lithium and by hypercalcemia.
Assessment Of Adipsic Di
Adipsic DI usually occurs in patients who have structural damage to the anterior hypothalamus where the osmoreceptors are situated. It has most often been reported following after clipping of anterior communicating aneurysms or after extensive surgery for craniopharyngiomas, though a wide variety of aetiologies have been reported in the literature. The hypothalamic damage is not confined to the osmoreceptors; a number of other hypothalamic abnormalities co-exist with the DI, including obstructive sleep apnoea, hypothalamic obesity, abnormal temperature regulation and seizure disorders.
A More Reliable Method For Diagnosing The Subtype Of Diabetes Insipidus
The easiest and most reliable method for evaluating a patient with suspected diabetes insipidus is the following:2,3
Collect a 24-hour urine
If the volume is abnormally high and osmolarity is low
Measure basal plasma AVP or copeptin
If this measure is low or undetectable, the Diabetes Inspidius is likely not nephrogenic
Order MRI of the brain without contrast in order to determine the presence or absence of the normal pituitary.A bright spot on T-1 weighted images will determine if the patient has:
· Primary polydipsiabright spot present
· Central diabetes insipidusbright spot small or absent3
The copeptin test, Dr. Robertson said, ”may be a reliable tool for differentiating nephrogenic diabetes insipidus from the other types of DI. Although the information on the reliability of this method is inadequate for full confidence, it may be easier to obtain and with proper improvements in the methods of interpretation may eventually prove to be a good alternative.”
Dr. Christ-Crain reports receiving personal fees from Thermofisher Scientific; Dr. Robertson has no financial disclosures relevant assessing this study.
Complications Of Diabetes Insipidus
Diabetes insipidus that isnât under control can make you more likely to have complications like:
- Dehydration. Diabetes insipidus makes it hard for your body to hold on to water. Itâs easy to get dehydrated.
- Electrolyte imbalance. Electrolytes are minerals in your body with a tiny electric charge. When you lose too much water, your electrolyte levels can go up. This might cause:
- A headache
Excluding Other Causes Of Polyuria
Once polyuria is confirmed, the next step would be to assess for urinary osmolality. The urine in cases of DI/primary polydipsia is hypotonic. A urine osmolality of >800 mOsm/Kg indicates optimal plasma AVP levels and appropriate renal response to AVP, therefore ruling out any form of DI . In most cases, polyuria with isotonic/hypertonic urine is driven by glucose, sodium, urea, or medications such as diuretics or mannitol . Glycosuria can result either from uncontrolled diabetes mellitus , general hyperglycemia , or by the use of SGLT-2 inhibitors . Administration of normal saline in large volumes for intravascular volume expansion can lead to sodium-induced polyuria . Sodium-induced polyuria is also seen with release of bilateral bladder obstruction . Urea-induced solute diuresis can be seen with high amounts of protein intake, tissue catabolism, steroid administration, all of which result in production of urea from breakdown of proteins . Administration of urea for treatment of hyponatremia, and recovery from azotemia can also result in urea-solute diuresis . Mannitol-induced diuresis can result from treatment of increased intracranial pressure with mannitol .
What Are The Longer
With appropriate treatment, patients with diabetes insipidus should be able to pursue a normal lifestyle. However, it is possible they will require long-term monitoring by their GP and/or endocrinologist. Patients need to be careful to avoid dehydration. In cranial diabetes insipidus, desmopressin is a life-sustaining therapy and should only be stopped following specialist advice, especially when patients are admitted to hospital for any reason.
What Are The Signs And Symptoms Of Diabetes Insipidus
The symptoms of diabetes insipidus include:
These symptoms are similar to those of diabetes mellitus, but there is no sugar present in the urine and blood sugar levels are normal.
Providing there is adequate provision of water to satisfy the excess thirst, the signs of diabetes insipidus can be minimal. Dehydration can occur if fluid intake cannot keep pace with the amount of urine passed. This can result in an imbalance of electrolytes in the blood, possibly causing symptoms such as headache, fatigue or muscle pain.
How Common Is Diabetes Insipidus
Diabetes insipidus is rare in the general population, affecting approximately one in 25,000 people. In patients who have had pituitary surgery, 1020% can experience symptoms temporarily after the operation. A similar percentage of patients who have had a severe head injury develop short-term diabetes insipidus. A minority of individuals have persistent symptoms after pituitary surgery and head injury.
Genetic causes of diabetes insipidus are very rare.
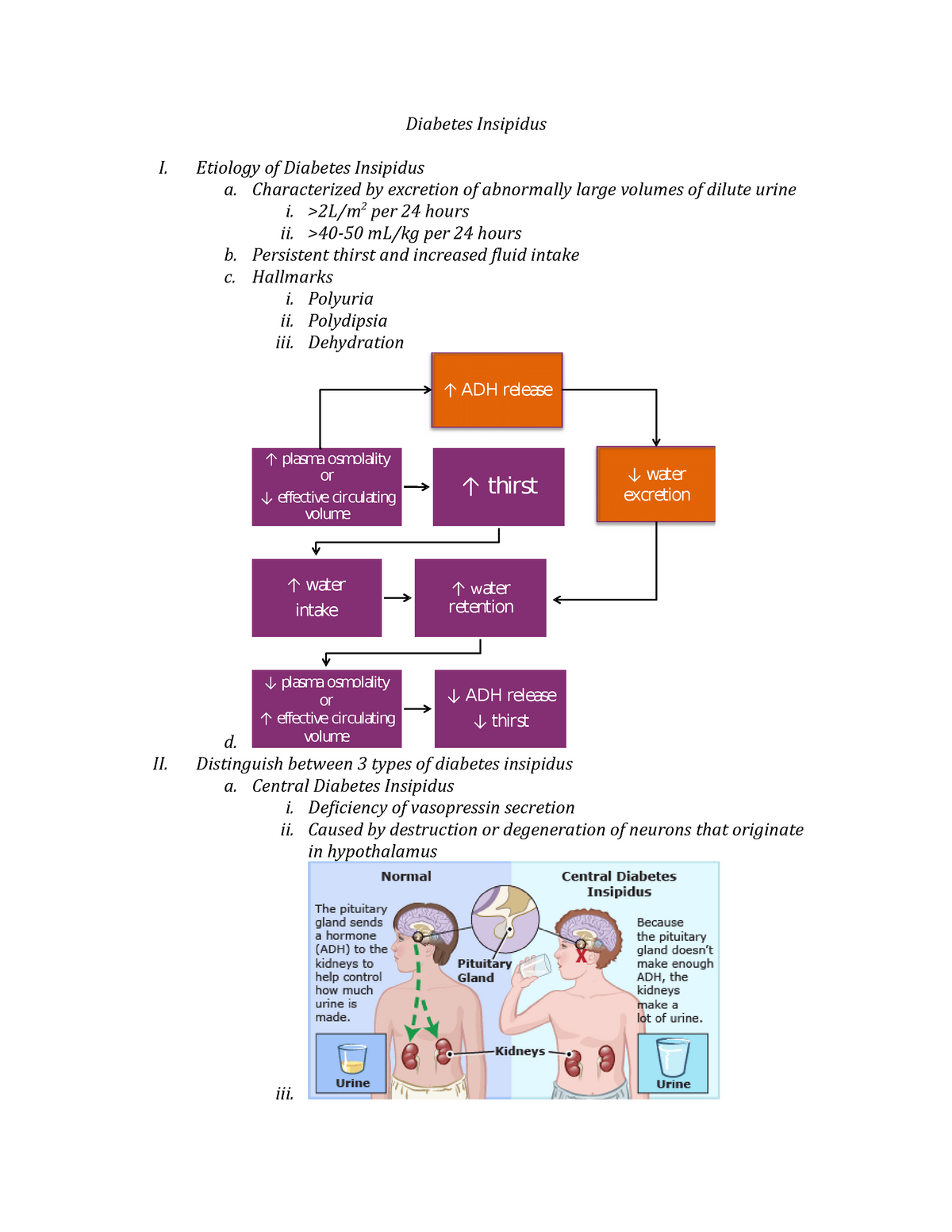
How Is Fluid Regulated In The Body
A person’s body regulates fluid by balancing liquid intake and removing extra fluid. Thirst usually controls a persons rate of liquid intake, while urination removes most fluid, although people also lose fluid through sweating, breathing, or diarrhea. The hormone vasopressin, also called antidiuretic hormone, controls the fluid removal rate through urination. The hypothalamus, a small gland located at the base of the brain, produces vasopressin. The nearby pituitary gland stores the vasopressin and releases it into the bloodstream when the body has a low fluid level. Vasopressin signals the kidneys to absorb less fluid from the bloodstream, resulting in less urine. When the body has extra fluid, the pituitary gland releases smaller amounts of vasopressin, and sometimes none, so the kidneys remove more fluid from the bloodstream and produce more urine.
Causes Of Diabetes Insipidus
Our kidney functions by filtering the blood multiple times. Only a little amount of concentrated urine is released and most of the water is reabsorbed. Diabetes insipidus happens when the kidneys are not able to concentrate the urine appropriately due to which a lot of dilute urine is excreted.
Antidiuretic hormone controls the amount of water that is excreted in the urine. ADH is also known as vasopressin. It is made in the part of the brain known as the hypothalamus. Then it is stored and secreted by the pituitary gland which lies just beneath the base of the brain.
DI that is occurred by the lack of ADH is known as central diabetes insipidus. When DI occurred due to the failure of kidneys to respond towards ADH, this particular condition is known as nephrogenic diabetes insipidus.
Thyroid Stimulating Hormone Free Thyroxine
It is essential to assess levels of both thyroxine and TSH in patients with potential pituitary pathology, since a normal TSH level is frequently associated with loss of thyroid function in this patient group.
Levels of both TSH and thyroxine are typically at the lower end of the normal range in hypopituitary patients.
What Health Problems Are Associated With Diabetes Insipidus
Most people urinate one to two liters of urine a day, but a person with diabetes insipidus might urinate three liters or more. Patients often wake up in the middle of the night to urinate. Because they are losing a lot of water in the urine, these patients are at risk for dehydration.
Patients who have diabetes insipidus have increased thirst and tend to drink a great deal of water. If the patient has no access to drinking water, he or she cannot make up for the loss of water, and the chemicals in the body get concentrated. The person may have increased levels of sodium in the blood , which cause confusion and other changes in mental status.
Symptoms Of Central Diabetes Insipidus
Symptoms may begin gradually or suddenly at any age. Often the only symptoms are
-
Excessive thirst
-
Excessive urine production
The person urinates excessively and often wakes during the night to urinate. A person may drink huge amounts of fluid4 to 40 quarts a dayto compensate for the fluid lost in urine. Ice-cold water is often the preferred drink. When compensation is not possible, dehydration can quickly follow, resulting in low blood pressure and shock. The person continues to urinate large quantities of dilute urine, and this excessive urination is particularly noticeable during the night.
Diagnosis Of The Type Of Diabetes Insipidus
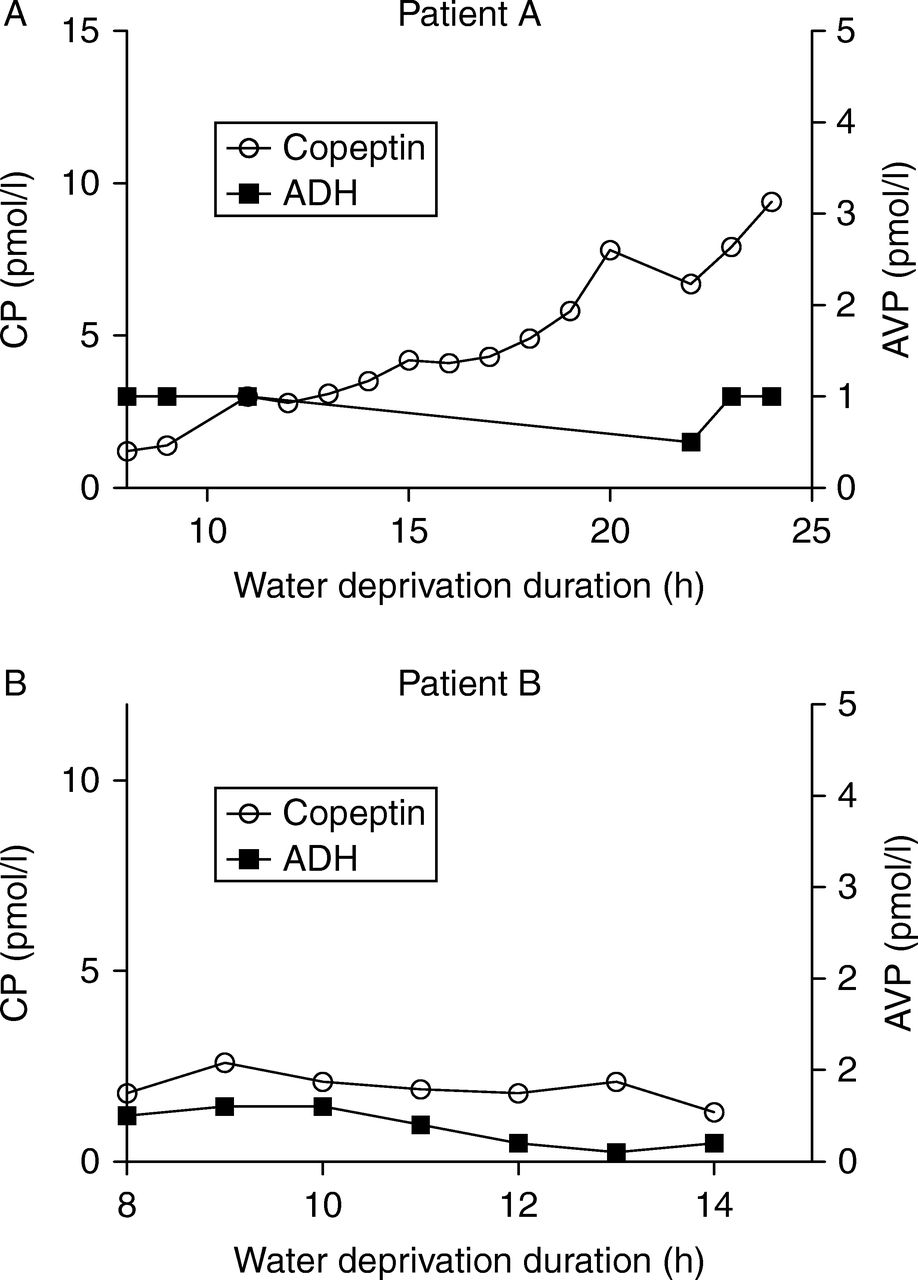
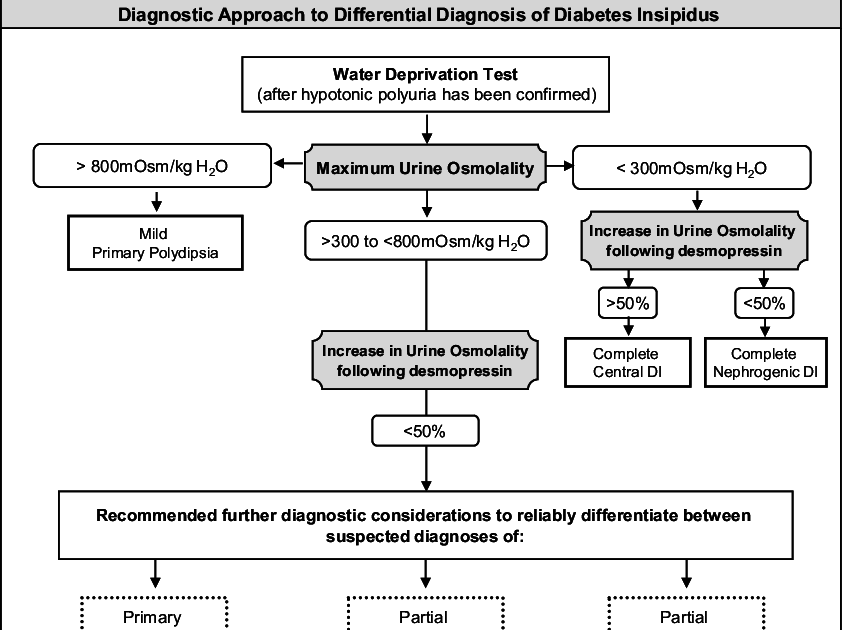
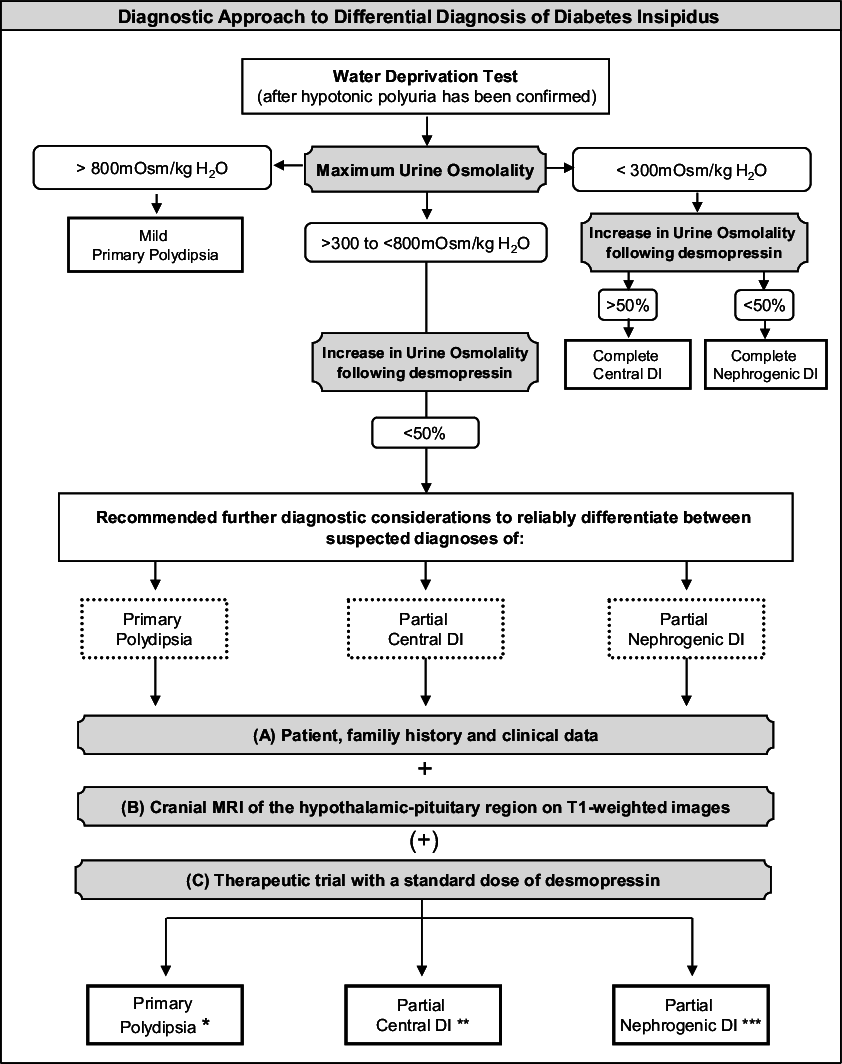
Probably the most challenging step in the work-up of a suspected case of DI is to assign an accurate diagnosis: central DI vs. nephrogenic DI vs. primary polydipsia. These polyuric-polydipsic states can demonstrate substantial overlap, both in their clinical presentation and in their response to diagnostic testing. It is also possible for one or more forms of polyuria-polydipsia syndrome to co-exist in a single individual. An algorithm for the diagnostic approach for DI is described in .
Diabetes Insipidus Is A Rare Disorder That Can Occur As A Consequence Of Histiocytosis Involving The Pituitary Gland
It should not be confused with the more common diabetes mellitus, also known as sugar diabetes, which results from too much sugar in the blood. Although both disorders have similar symptoms, in every other way including the cause and treatment, they are completely unrelated diseases.
The rate of occurrence for DI is not known, because there has been no organized method to count the number of patients.
Diabetes insipidus is a result of damage to the pituitary gland, a small gland at the base of the brain which stores and releases a hormone called ADH , also known as vasopressin. This hormone normally causes the kidney to control the amount of water released as urine from the body. When the pituitary is damaged, the kidneys lose too much water , which then leads to increased thirst.
The connection between histiocytosis and diabetes insipidus was first reported in the late 1800s. Since then, DI has been recognized as a characteristic feature of LCH. It is known to also occur in other histiocytic disorders, such as Rosai Dorfman and JXG.
It is believed that approximately between 5% and 50% of LCH patients develop DI depending on the extent of disease. The risk of developing DI in patients with multisystem LCH is 4 to 6 times more than those with single-system disease. Patients with skull, facial, and/or eye bone lesions are at much higher risk of developing DI. This risk is increased further if LCH remains active for a longer period or if it recurs.
The 10 Best Supplements For Diabetes Insipidus On 2021 According To Experts
As I talked about on top, I dedicate a a lot of days consulting with management specialists who have dotage of experience and have used a copious days using assorted supplements for diabetes insipidus. Also, to discovered this index nonpartisan, we made sure that none of the consultants we interviewd were part of any logotype.
Confirmation Of Hypotonic Polyuria
Polyuria is defined as excretion of a urinary volume >150 ml/Kg/24 hours at birth, >100-110 ml/Kg/24 hours up to the age of 2 years, and >50 ml/Kg/24 hours in older children or adults. A hypotonic urine is typically defined as a urine with an osmolality of <300 mOsm/Kg. The primary objective in this step involves differentiating between conditions that give rise to polyuria resulting from osmotic diuresis and DI/primary polydipsia, in which polyuria predominantly involves water diuresis.
What Is The Difference Between Diabetes Mellitus And Diabetes Insipidus
There are two types of diabetes in dogs. Diabetes mellitus is also called sugar diabetes and results from a disruption of pancreas function and abnormal regulation of blood sugar. The term, meaning ‘sweetened with honey’, originated from the fact that the urine of these patients was ‘sweet’ due to high amounts of sugar excreted from the body.
Diabetes insipidus gets its name from the fact that the urine of these patients is dilute enough to be ‘tasteless’ or ‘insipid’. Diabetes insipidus is rare in dogs, and is characterized by excessive thirst/drinking and the production of enormous volumes of extremely dilute urine. Some dogs may produce so much urine that they become incontinent . The irony of this disease is that despite drinking large volumes of water, the dog can become dehydrated from urinating so much.
How Are They Treated
Thereâs no cure for diabetes mellitus or diabetes insipidus, but you can manage them.
If you have type 1 or type 2 diabetes, youâll usually manage your blood sugar with insulin shots or other medications. Check it daily to make sure itâs in a safe range. Youâll need to eat a healthy diet and get regular exercise to keep your weight, cholesterol, and blood pressure down. See your doctor for regular checkups.
Treatment for diabetes insipidus depends on which of the four types you have:
- Central: A synthetic hormone called desmopressin can replace the vasopressin your body doesnât make to manage your symptoms. It comes as a nasal spray, shot, or pill.
- Nephrogenic:Diuretics and aspirin or ibuprofen can help with symptoms of nephrogenic diabetes insipidus. Your doctor also may check to make sure that the calcium and potassium in your body are in balance. Sometimes this type can go away once you treat it.
- Dipsogenic: In dipsogenic diabetes insipidus, the problems with your hypothalamus and pituitary gland extend to your thirst mechanism. This means that even though youâre losing a lot of fluid, youâre still not thirsty. Doctors are still at work on a treatment, but for now, they suggest that you suck on ice chips or hard, sour candy to trigger your urge to drink.
- Gestational: This type of diabetes insipidus can happen when youâre pregnant. Doctors often treat this with desmopressin. Most women donât continue to need treatment after they give birth.
Which Lab Tests Are Performed To Confirm The Diagnosis Of Diabetes Insipidus
In a patient whose clinical presentation suggests diabetes insipidus , laboratory tests must be performed to confirm the diagnosis. A 24-hour urine collection for determination of urine volume is required. In addition, the clinician should measure the following:
-
Serum electrolytes and glucose
-
Simultaneous plasma and urinary osmolality
-
Plasma antidiuretic hormone level
Perform testing with the patient maximally dehydrated as toleratedthat is, at a time when ADH release is the highest and his/her urine is the most concentrated. Water deprivation testing may be useful in situations in which the diagnosis is uncertain.
Are There Any Side
Side-effects are very rare. Too much desmopressin can lead to low salt levels in the blood and a gathering of excess fluid in the body. This occurs because the desmopressin prevents the kidneys from excreting enough urine. If the patient is concerned about any side-effects, he or she should talk to their endocrinologist or GP.
Tests For Diabetes Insipidus
Diabetes Insipidus is diagnosed using a number of pointers and symptoms you describe to your doctor. A physical exam is necessary. Your familys medial history as well as your own are also considered. Diagnostic tests for Diabetes Insipidus may then be requested by your doctor. Tests involved in diagnosing Diabetes Insipidus are
- Blood Tests Blood tests for Diabetes Insipidus diagnosis measure the levels of calcium, sodium and bicarbonates in a blood sample collected via venipuncture. Diabetes Insipidus sodium levels are usually higher than average. A blood test also helps identify some types of Diabetes Insipidus.
- Fluid deprivation test The fluid deprivation test uses thirst to see how much fluid you lose from your body. Substitutes of vasopressin may be given by your doctor in the diagnostic process. There are two versions of the fluid deprivation test one long and the other short.
- Urinalysis An analysis of your urine will be done. It checks for concentrations of electrolytes in your blood.
- MRI Scan This imaging test helps your doctor identify anomalies in your body organs. Of interest are your kidneys, the hypothalamus and the pituitary gland.
In laboratory diagnosis of Diabetes Insipidus, urine and plasma are analyzed. You have Diabetes Insipidus if your results are below these minimum diabetes insipidus lab values
How Do I Manage My Symptoms
- Weigh yourself each day. Weigh yourself at the same time each day, on the same scale. Rapid weight loss can be a sign of fluid loss in your body.
- Drink liquids as directed. Follow your healthcare provider’s instructions about how much liquid you should drink and what kinds of liquids to drink.
- Limit sodium as directed. You may need to decrease the amount of sodium you eat if you have NDI. This helps decrease the amount of fluids you lose.
Clinical Consequences Of Avp Deficiency Besides Polyuria
Interestingly, lack of AVPR2 activation with consecutive polyuria has been the only major clinical issue associated with AVP deficiency so far. However, AVP is involved in a wide range of physiological regulatory processes beyond water reabsorption. AVPR1a and AVPR1b are found not only in the periphery, but also in different areas throughout the brain , that is AVP1b receptors are heavily expressed on the anterior pituitary corticotropes. As AVP is a well-known regulator of the hypothalamusâpituitaryâadrenal axis, one would expect altered stress physiology in DI. In fact, several reports have indicated different HPA response patterns after various stimuli in DI patients versus healthy controls . One explanation includes the upregulation of CRH receptors in DI leading to an increased sensitivity of pituitary ACTH-producing cells to CRH stimulus. Although this distinct HPA response pattern in DI is quite consistently described in the literature, the clinical impact of this finding remains completely unknown.
In the periphery, AVPR1a is primarily involved in vasoconstrictive responses in vascular tissue. The regulation of systemic blood pressure, vascular tonus and blood volume is very complex, and the precise contribution of AVPR1a has not fully been defined . Lack of AVPR1a activation in DI patients does not seem to have a major impact on blood pressure regulation.

