What Else Can I Do To Control My Blood Glucose Levels
Food, sleep, and exercise are all of vital importance for regulating your blood sugar when you have diabetes.
What Are Alternative Medications For People With Diabetes That Arent Insulin
- Metformin a pill that stops sugar production in the liver
- Glitazones pills that remove sugar from the bloodstream
- Sufonylureas and glinides pills that increase the release of insulin from your pancreas
- Starch blockers pills that slow starch absorption
- Incretin therapies and amvlin analogs pills and injections that reduce sugar production in the liver and slow food absorption. Types of the former include DPP4 inhibitors and GLP1 analogs .
- SGLT2 inhibitors pills that are taken before meals that prevent the reabsorption of glucose
Faq: Frequently Asked Questions
1. Why is insulin so expensive?
Though reforms are underway in many parts of the US, insulin costs are still prohibitively expensive for many people with diabetes. Reasons include the complexity of the pharmaceutical supply chain and lack of generic substitutes.;;
2. What is sliding scale insulin?
Sliding scale therapy is a regimen that prescribes a progressive increase in insulin doses before meals and at bedtime, based on your blood sugar levels.
3. What is an insulin index?
The insulin index gives foods a rating based on how much your blood insulin concentration rises in the two hours after consumption.
4. What is an insulin resistance diet?;
An insulin resistance diet incorporates foods that will help maintain your bodys balance of insulin and blood sugar. Think nourishing calories from veggies, fruit, lean proteins, and healthy fats.
You May Like: How Many Points Does Metformin Lower Blood Sugar
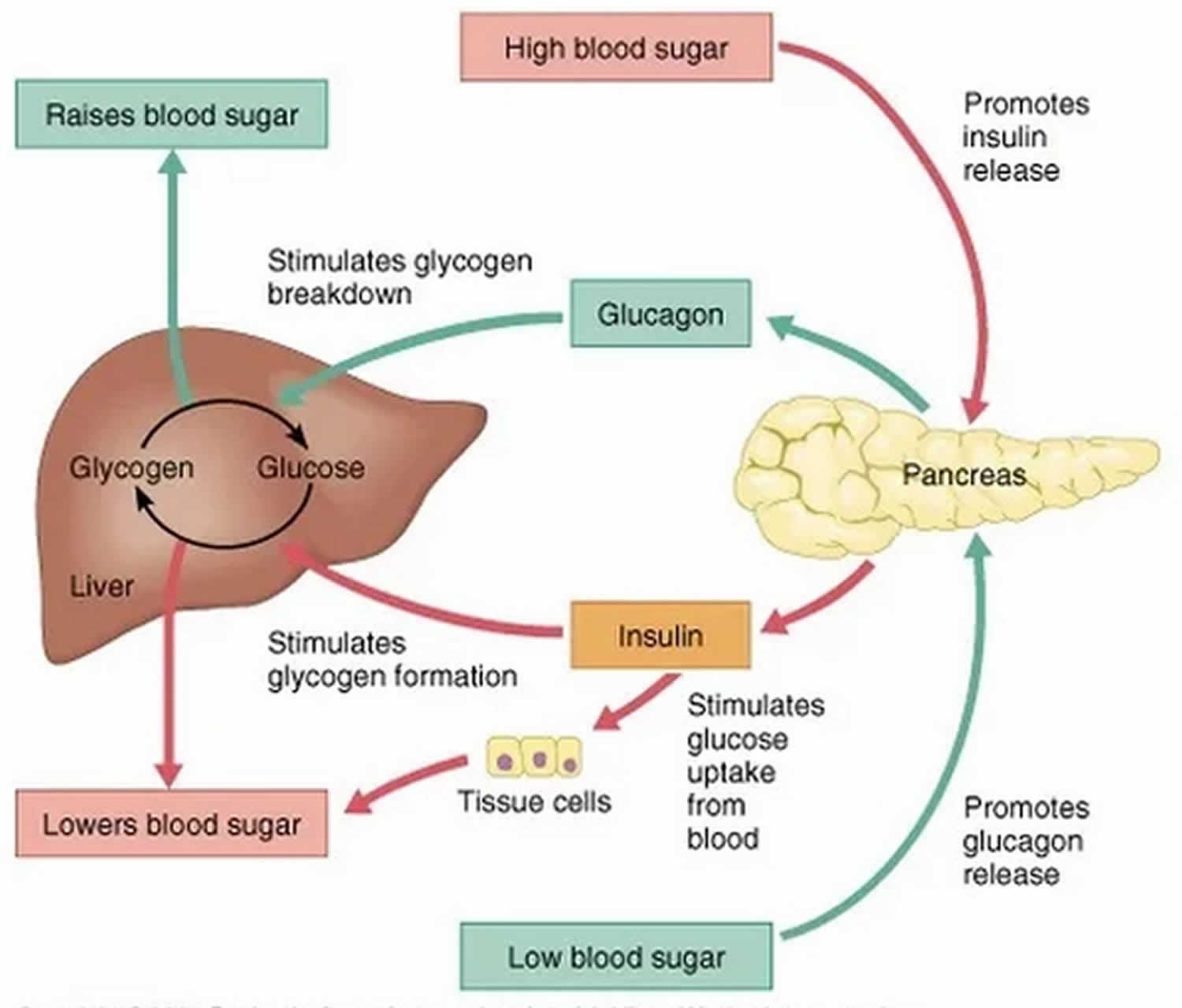
Regulation Of Blood Glucose Levels By Insulin And Glucagon
Glucose is required for cellular respiration and is the preferred fuel for all body cells. The body derives glucose from the breakdown of the carbohydrate-containing foods and drinks we consume. Glucose not immediately taken up by cells for fuel can be stored by the liver and muscles as glycogen, or converted to triglycerides and stored in the adipose tissue. Hormones regulate both the storage and the utilization of glucose as required. Receptors located in the pancreas sense blood glucose levels, and subsequently the pancreatic cells secrete glucagon or insulin to maintain normal levels.
The Pathogenesis Of T1d
A decrease in both mass and insulin secretary function of -cells is the common characteristic shared in both type 1 and type 2 diabetic patients. Autoimmunity plays a critical role in the development of T1D. The classical T1D is characterized by the presence of antibody and T-cell responses to self-islet proteins . Histological analysis of the pancreas from patients with T1D shows the presence of immunological activity . Drugs that suppress the immune response such as cyclosporine and azathioprine can slow the progression of -cell destruction pointing to the critical role of immune activity in development of type 1 diabetes . Development of T1D may be influenced by dietary factors including early infant feeding status , Vitamin D and omega 3 polyunsaturated fatty acid intake , and duration of exposure to gluten . People with genetic predispositions have a higher risk to develop overt T1D. Human leukocyte antigen encodes cell surface proteins that interact with immune cells and are an important gene family that contributes up to 40% of T1D risk. The HLA Class II region is considered to be the most influential. In Caucasians, HLA types DR3-DQA 0501-DQB1 0201 and DR4-DQA1 0301-DQB1 0302 are strongly associated with risk, while DQB1 0602 is associated with protection .
Don’t Miss: How Many Points Does Metformin Lower Blood Sugar
What Happens If I Have Too Little Glucagon
Unusual cases of deficiency of glucagon secretion have been reported in babies.;This results in severely low blood glucose which cannot be controlled without administering glucagon.;
Glucagon can be given by injection to restore blood glucose lowered by insulin .;It can increase glucose release from glycogen stores more than insulin can suppress it. The effect of glucagon is limited, so it is very important to eat a carbohydrate meal once the person has recovered enough to eat safely.
Factors Influencing Insulin Biosynthesis And Release
Insulin secretion may be influenced by alterations in synthesis at the level of gene transcription, translation, and post-translational modification in the Golgi as well as by factors influencing insulin release from secretory granules. Longer-term modification may occur via influences on cell mass and differentiation. Given insulins pivotal role in glucose utilisation and metabolism, it is not surprising that glucose has multiple influences on insulin biosynthesis and secretion. However, other factors such as amino acids, fatty acids, acetylcholine, pituitary adenylate cyclase-activating polypeptide , glucose-dependent insulinotropic polypeptide , glucagon-like peptide-1 , and several other agonists, together in combination, also influence these processes.
Recommended Reading: Whats A Normal A1c
Oscillatory Responses And Cell
Over the physiological range of glucose concentrations, cell electrical activity consists of oscillations in membrane potential between depolarised plateaux, on which bursts of action potentials are superimposed, separated by repolarized electrically silent intervals. These oscillations in electrical activity are accompanied by changes in the cytoplasmic Ca2+ concentration , as demonstrated in Figure 2, which in turn give rise to brief pulses of insulin secretion .
These oscillations reflect a balance between activation of VDCCs and K+ channel activity . The depolarizing component predominates at the beginning of the burst, but the resultant influx of Ca2+ during the plateau leads to a progressive Ca2+-induced increase in K+ channel activity. This occurs both via a direct effect on small conductance Ca2+-activated K+ channels , and via an indirect effect on KATP channels by lowering of the cytoplasmic ATP:ADP ratio due to increased Ca2+ ATPase activity . The increase in K+ channel activity eventually becomes large enough to repolarize the cell, ending the burst. In this scenario, the slow pacemaker depolarization between two successive bursts results from the gradual restoration of i and the ATP:ADP ratio until SK and KATP channels are again closed and the background depolarizing conductance becomes sufficiently large to trigger a new burst of action potentials.
What Happens If I Have Too Little Insulin
People with diabetes have problems either making insulin, how that insulin works or both. The main two types of diabetes are type 1 and type 2 diabetes, although there are other more uncommon types.
People with type 1 diabetes produce very little or no insulin at all. This condition is caused when the beta cells that make insulin have been destroyed by antibodies , hence they are unable to produce insulin. With too little insulin, the body can no longer move glucose from the blood into the cells, causing high blood glucose levels.;If the glucose level is high enough, excess glucose spills into the urine.;This drags extra water into the urine causing more frequent urination and thirst.;This leads to dehydration, which can cause confusion. In addition, with too little insulin, the cells cannot take in glucose for energy and other sources of energy are needed to provide this energy.;This makes the body tired and can cause weight loss. If this continues, patients can become very ill. This is because the body attempts to make new energy from fat and causes acids to be produced as waste products.;Ultimately, this can lead to coma and death if medical attention is not sought. People with type 1 diabetes will need to inject insulin in order to survive.
Recommended Reading: Insulin Or D50 First For Hyperkalemia
Regulation Of Glucagon Action
Clearly, insulin replacement therapy has been an important step towardrestoration of glucose homeostasis. But it is only part of the ultimatesolution. The vital relationship between insulin and glucagon has suggestedadditional areas for treatment. With inadequate concentrations of insulin andelevated concentrations of glucagon in the portal vein, glucagon’s actions areexcessive, contributing to an endogenous and unnecessary supply of glucose inthe fed state. To date, no pharmacological means of regulating glucagon existand the need to decrease postprandial glucagon secretion remains a clinicaltarget for future therapies.
Other Causes Of High Insulin
The most common cause of high insulin is high blood sugar. But in rare cases, hyperinsulinemia can be caused by conditions that affect the pancreas. One of these conditions is a rare type of pancreatic tumor called an insulinoma, according to Johns Hopkins Medical Center.
Hyperinsulinemia can also be caused by a condition called nesidioblastosis, in which the pancreas makes too many insulin-producing cells, according to the U.S. National Library of Medicine.
In both of these cases, hyperinsulinemia can cause symptoms of low blood sugar, aka hypoglycemia. Hypoglycemia symptoms can include hunger, irritability, confusion, blurred vision and feeling weak, faint, shaky or fatigued, according to the Mayo Clinic. Be sure to consult with your doctor if you are experiencing these symptoms.
Also Check: Diabetes And Bananas
Types Of Insulin Administration With Needles Pumps Pens And Why Insulin Is So Expensive
What does insulin do? Help your body turn food into energy, for starters. When youre diabetic, and youre either not producing insulin, or your insulin function is off, all sorts of things can go wrong. From needles, to pens, to pumps, to types of insulin, were here to empower you with clear answers to all your pressing Qs.
In This Article:;
Alvin Powers MD,;Mihail Zilbermint MD, and;Irl Hirsch MD
Glucose Metabolism And Regulation: Beyond Insulin And Glucagon
Don’t Miss: Which Pancreatic Cells Release Insulin And Glucagon
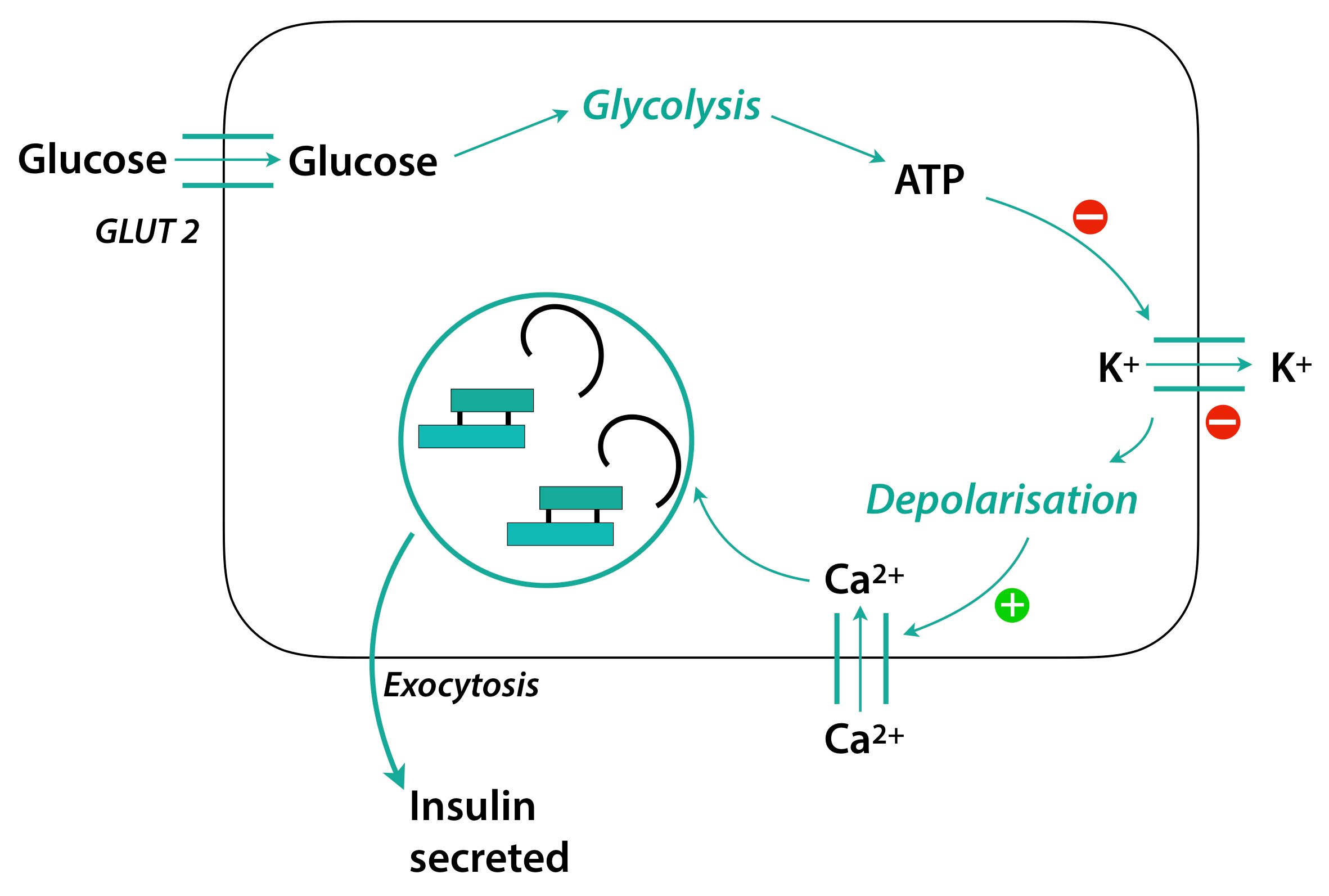
Coupling Glucose Metabolism And Atp Production In Cells
Because the membrane voltage is sensitive to changes in ATP levels within the cell, perturbations of the metabolic pathways that generate ATP can have a strong effect on insulin secretion. ATP is generated in mitochondria through the electron transport chain, and is dependent upon the presence of a proton gradient across the mitochondrial membrane. In cells, expression of uncoupling protein-2 can disrupt the generation of ATP in mitochondria by permitting protons to leak across the mitochondrial membrane. When UCP2 is overexpressed, the generation of ATP is bypassed , while loss of UCP2 expression results in increased ATP levels and also enhanced insulin release by islets . Accordingly, there may exist a correlation between expression levels of UCP2 and diabetes or obesity.
Although UCP2 clearly plays a role in regulating ATP production, the molecular pathways controlling its expression are not well understood. Bordone et al. uncovered one potential regulator of UCP2 expression in their studies of Sirt1 expression and function in murine islets. The authors found that Sirt1, a homologue of Sir2 is expressed in cells, and that it downregulates UCP2 expression in these cells. This identifies Sirt1 as a positive regulator of insulin secretion from cells.
Regulation Of Insulin Transcription
Insulin biosynthesis is regulated both at transcriptional and translational levels. In a mouse -cell, there are roughly 13,000 insulin granules. They occupy more than 10% of the total cell volume . Each granule contains approximately 200,000 insulin molecules . However, insulin content in -cells is highly dynamic. Insulin accumulates in the presence of nutrients and decreases in response to nutrient deprivation. The ability of -cells to quickly respond to cellular signals is generally due to transcriptional regulation. A number of discrete sequence elements within the promoter region of insulin gene, named A, C, E, Z, and CRE elements determine localization of insulin in -cells and also serve as binding sites for several -cell transcription factors to regulate insulin gene expression . The transcription factor binding sites that are located within a region spanning ~-400 base pairs relative to the TSS are determinants of -cell-specific expression of insulin .
A number of cis- and trans- transcriptional factors are associated with the activation of the insulin enhancer region. In all characterized insulin enhancer sequences the A, C, and E elements are contained in core binding motifs .
A elements
C element
E element
Z element
Cyclic AMP response element
Also Check: Diabetes Type 2 Life Expectancy
Insulin Secretion Diabetes And Ketone Body Metabolism
Insulin secretion occurs through two mechanisms. The first is a process that involves closing of the cell-surface ATP-sensitive potassium channels in response to increases in the circulating glucose concentrations, which stimulates exocytosis of insulin-containing vesicles from the -islet cells through an increase in the cytosolic calcium concentration. The second mechanism is dependent on pyruvate carboxylase, which is highly expressed in -islet cells; it has been estimated that 3545% of pyruvate enters the citric acid cycle through this anaplerotic pathway in -islet cells. Inhibition of pyruvate carboxylase with phenylacetic acid decreases glucose-stimulated insulin release from -islet cells. Furthermore, there is evidence that pyruvate carboxylase plays an important role in the early stages of type 2 diabetes. Specifically, in Zucker fatty rats with insulin resistance, the hyperfunctioning -islet cells increase insulin production in part through increases in pyruvate carboxylase activity.
Regulation Of Insulin Translation
In response to nutrients, -cells enhance their overall speed of protein translation, which is at least partly controlled by dephosphorylation of eukaryotic initiation factor 2a via protein phosphatase 1 . For example, exposure of -cells to high glucose for 2 hours significantly decreases the ratio of phosphorylated eIF2a to eIF2a . However, there are additional mechanisms to regulate glucose-induced insulin translation, since the overall protein translation induced by glucose compared to the fasting state in -cells was only 3-fold compared with an up to 8-fold induction in proinsulin translation .
Also Check: Nph Regular Insulin Mixing
Types Of Insulin Treatments
All types of insulin produce the same effect. They mimic the natural increases and decreases of insulin levels in the body during the day. The makeup of different types of insulin affects how fast and for how long they work.
- Rapid-acting insulin: This type of insulin begins working approximately 15 minutes after injection. Its effects can last between three and four hours. Its often used before a meal.
- Short-acting insulin: You inject this insulin before a meal. It starts working 30 to 60 minutes after you inject it and lasts five to eight hours.
- Intermediate-acting insulin: This type of insulin starts working in one to two hours after injection, and its effects may last 14 to 16 hours.
- Long-acting insulin: This insulin may not start working until about two hours after you inject it. Its effects can last up to 24 hours or longer.
Viii Pharmacologic Modulators Of Insulin Response
There is a plethora of pharmcologic agents designed to target various aspects of glucose metabolism. In this chapter, we provide examples of pharmacologic agents that directly or indirectly modulate insulin response.
A. Incretin mimetics
Diabetes therapeutics have recently utilized the role of incretin hormones for pharmacologic benefit. Due to the desirable effect of GLP-1 on hemoglobin A1c reduction and weight loss , GLP-1 receptor agonists and inhibitors of its degradation via dipeptidyl peptidase-4 inhibitors, have been used to treat type 2 diabetes since 2005.
Short-acting GLP-1 receptor agonists , and long-acting GLP-1 receptor agonists potentiate insulin secretion and reduce gastric motility . Given that GLP-1 receptor agonists potentiate glucose-induced insulin gene transcription, they, alone, do not induce hypoglycemia when used as monotherapy .
DPP-4 inhibitors can significantly increase the peak post-prandial concentration of GLP-1 . Additionally, sitagliptin has been found to potentiate GSIS independently of GLP-1 via islet peptide tyrosine tyrosine .
B. Sulfonylureas
C. Insulin Sensitizers
D. Diazoxide
Diazoxide is a sulfonamide pharmacological agent used in treatment of hyperinsulinism, insulinoma, and hypoglycemia due to overtreatment with sulfonylureas. It works by opening b cell membrane potassium ATP channels, hyperpolarizing the b cells, thus decreasing intracellular calcium concentration and inhibiting insulin secretion .
Recommended Reading: Does Diet Soda Raise Insulin Levels
The Effects Of Insulin On The Body
Insulin is a natural hormone produced by your pancreas that controls how your body uses and stores blood sugar . Its like a key that allows glucose to enter cells throughout your body.
Insulin is a vital part of metabolism. Without it, your body would cease to function.
When you eat, your pancreas releases insulin to help your body make energy out of glucose, a type of sugar found in carbohydrates. It also helps you store energy.
In type 1 diabetes, the pancreas is no longer able to produce insulin. In type 2 diabetes, the pancreas initially produces insulin, but the cells of your body are unable to make good use of the insulin. This is called insulin resistance.
Unmanaged diabetes allows glucose to build up in the blood rather than being distributed to cells or stored. This can wreak havoc with virtually every part of your body.
Blood tests can quickly indicate whether your glucose levels are too high or too low.
Complications of diabetes include kidney disease, nerve damage, heart problems, eye problems, and stomach problems.
People with type 1 diabetes need insulin therapy to live. Some people with type 2 diabetes must also take insulin therapy to control their blood sugar levels and avoid complications.
If you have diabetes, insulin therapy can do the job your pancreas cant. The following types of insulin are available:

