How Does Type 1 Diabetes Affect The Digestive System
diabetesaffectOnedigestion
. People also ask, can Type 1 diabetes cause stomach problems?
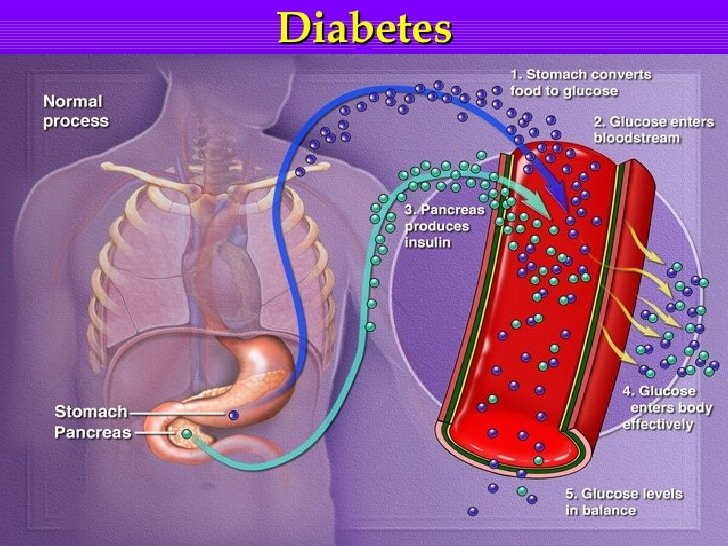
Many children and adolescents with Type 1 diabetes suffer with delayed gastric emptying. exclusively in those individuals with long- standing diabetes. Gastroparesis can be evident early in the diagnosis of diabetes. Various regions of the diabetic stomach may be affected or hampered.
Furthermore, can high blood sugar cause digestive problems? Diabetes and GastroparesisHigh blood sugar from diabetes can cause chemical changes in the vagus nerve, which connects the brainstem to the gastrointestinal tract. Gastroparesis symptoms include nausea, vomiting, reduced appetite, feeling full after eating small amounts of food, abdominal pain, and heartburn.
Besides, how does Type 1 diabetes affect the urinary system?
Diabetics are prone to urinary tract infections , bladder issues and sexual dysfunction. Diabetes can often make your urologic conditions even worse because it can impact blood flow, nerves and sensory function in the body. But, in people with type 1 diabetes, the body doesn’t make insulin at all.
How does diabetes affect other body systems?
The excess blood sugar in diabetes can wreak havoc on blood vessels all over the body and cause complications. It can severely damage the eyes, kidneys, nerves, and other body parts; cause sexual problems; and double the risk of heart attack and stroke.
How Diabetes Affects The Stomach
According to doctors, the other term for gastroparesis is diabetic stomach. Autonomic neuropathy that is the damaging of the vagus nerve, makes the movement of the food slow, thus retaining it for an extended period. This accumulation of solid mass in the stomach leads to awful pain and discomfort.
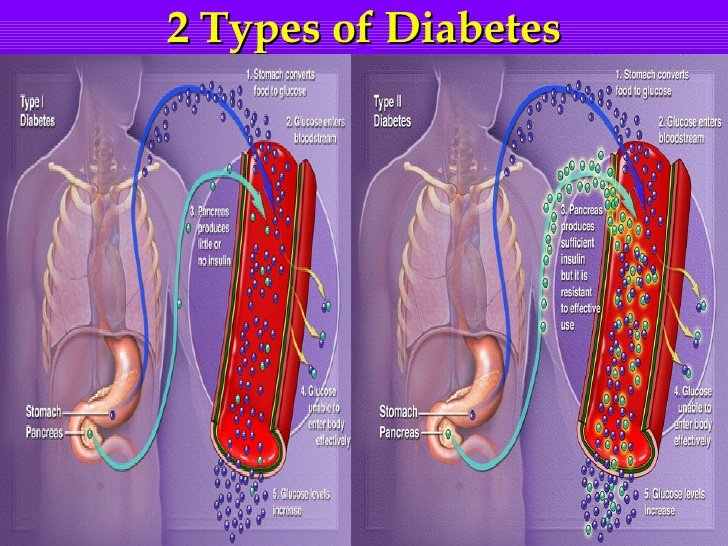
The principal cause of this has been owed to diabetes. Although it occurs in both type 1 and type 2 diabetes, but according to WHO, type 1 patients are more frequented by it. Type 1 diabetes stomach problems include irregular bowel movements, accidental bowel leakage, prolonged removal of the stomachs content and bloating of the stomach.
Normally, the surplus glucose in the body, if any, is flushed out through urine. However, a diabetic patient with high glucose level can acquire urinary tract infection due to the bacterial development in the excretory system. It can also result in the damage of nerves and kidney.
Gi Symptoms And Glucose
Several diabetes-specific medications, including metformin, -glucosidase inhibitors, and, more recently, the amylin analog pramlintide and GLP-1 RAs are strongly associated with GI adverse effects . As discussed, these studies have almost exclusively assessed symptoms by self-report, compromising data interpretation. Whether preexisting GI symptoms increase the propensity for adverse GI effects from these drugs remains to be determined.
Prevalent GI symptoms in type 1 and 2 diabetes, and medications for diabetes with which they may be associated.
The -glucosidase inhibitors frequently induce GI symptoms, including flatulence, loose stools, abdominal distension, and diarrhea , reflecting the presence of undigested complex carbohydrates in the large intestine, which undergoes bacterial fermentation with production of short-chain fatty acids and hydrogen . In clinical trials, the prevalence of GI symptoms with acarbose has varied widely; symptoms tend to subside with continued treatment and adherence to dietary restrictions . Lipase inhibitors such as orlistat and sugar alcohols such as sorbitol and mannitol also may cause diarrhea .
Pramlintide, a synthetic analog of amylin was FDA approved in 2005 for use in both type 1 and 2 diabetes and slows gastric emptying markedly . Nausea occurs in 1060% of cases, particularly with higher doses, but is usually transient .
You May Like: How Long Can You Live With Type 2 Diabetes
Preventing Digestive Issues In Diabetes: The Bottom Line
Keeping blood sugar under control is key to prevent gastrointestinal issues from occurring, Cline says.
If you have any symptoms, make sure to reach out to your medical team: With gastroparesis, its especially important to treat it early, Cline explains. With time and if left untreated, more nerve damage to the intestine occurs. By communicating with your providers, you can settle on a course of treatment and help prevent any severe complications.
Diabetes Symptoms And Diagnosis
The most common symptoms of any type of diabetes are extreme thirst and frequent urination, increased appetite, fatigue or exhaustion, dry skin, and vision changes . In more severe cases, symptoms can include unexplained weight loss or gain, slow-healing injuries, frequent illness or infections , and pain or numbness in the hands or feet. Long-term complications of diabetes can include kidney disease, cardiovascular disease, vision loss, and lower limb amputation.4 Those with type 2 diabetes might not experience any symptoms at first, or just one symptom, such as feeling slightly thirstier than previously. Type 1 diabetes tends to be more severe, especially in young children, who can experience weight loss and failure to thrive.
Your physician will order blood tests to assess fasting glucose as well as your average glucose levels over the last two to three months and, depending on your results, will determine whether you have normal levels, prediabetes, or some form of diabetes.
You May Like: What Makes Insulin In The Body
How Is Gastroparesis Treated
Like most complications of diabetes, the first thing is to get your blood glucose levels under control. Doctors may instantly adjust insulin levels and provide you with medication
Your diet may also need to be changed, including portions and meal frequency.
Some doctors recommend parenteral nutrition direct delivery of nutrition to the blood stream.
There are several types of gastroparesis drugs, including:
- Metoclopramide
- Antiemetics
This might include eating 6 small meals per day instead of 3, eating liquid meals, avoiding fatty foods, and avoiding high-fibre foods.
Are There Any Other Treatments For Gastroparesis
A newer treatment for gastroparesis is called per oral pyloromyotomy . This is a nonsurgical procedure in which the doctor inserts an endoscope into the patients mouth and advances it to the stomach. The doctor then cuts the pylorus, the valve that empties the stomach, which allows food to move from the stomach to the small intestine more easily.
In a severe case of gastroparesis, your doctor may decide you would benefit from a feeding tube, or jejunostomy tube. The tube is inserted in a surgical procedure through your abdomen into your small intestine. To feed yourself, you put nutrients into the tube, which go directly into your small intestine; this way, they go around the stomach and get into your bloodstream more quickly. The jejunostomy tube is usually a temporary measure.
Another treatment option is intravenous, or parenteral, nutrition. This is a feeding method in which nutrients go directly into your bloodstream through a catheter placed into a vein in your chest. Like a jejunostomy tube, parenteral nutrition is meant to be a temporary measure for a severe case of gastroparesis.
Read Also: What Should Be Fasting Blood Sugar Level
How Diabetic Neuropathy Can Lead To Heartburn And Other Issues
So how might diabetes affect the digestive system? Advanced diabetes, whether its from type 1 or type 2 diabetes, can affect any organ in the body including those organs in the digestive tract, says James C. Reynolds, MD, a gastroenterology specialist and clinical medicine professor at the University of Pennsylvania in Philadelphia.
Dr. Reynolds notes digestive problems may be caused by the very factors that led to diabetes in the first place, such as obesity, but its also possible that digestive problems are the result of diabetes-related complications, such as hyperglycemia, or high blood sugar.
One of the most serious diabetes complications that can result from consistent high blood sugar is diabetic neuropathy, or nerve damage. Neuropathy may lead to weakness, pain, and numbness, affecting feeling in your feet, legs, and hands, but the condition can also affect digestive functions like swallowing and constipation, Reynolds explains.
If you have diabetes, this potential complication is just another reason its crucial to pay attention to your A1C, the average level of glucose over the past two to three months, Reynolds says.
Gastrointestinal Symptoms In Diabetes: Prevalence Assessment Pathogenesis And Management
If you havent measured something, you really dont know much about it.
Karl Pearson
Recommended Reading: What Benefits Are Diabetics Entitled To
Pathogenesis Of Gi Symptoms In Diabetes
In the broadest sense, GI symptoms in diabetes can be regarded as the outcome of a disordered gut-brain axis. Potential pathogenic factors include autonomic and peripheral neuropathy, structural and functional central nervous system changes , acute and chronic dysglycemia, psychological dysfunction, and pharmacotherapy. Specific pathogenic factors relevant to each section of the GI tract are discussed subsequently.
The putative association of GI symptoms with disordered GI motor function arising from irreversible autonomic neuropathy is long-standing . The few tests that specifically evaluate GI autonomic function are not widely available , and standardized tests of cardiovascular reflexes typically are used as a surrogate . Autonomic neuropathy, as assessed by these tests, is closely associated with symptoms and signs of peripheral neuropathy in diabetes . However, the relationships between GI symptoms and the presence of autonomic or peripheral neuropathy are weak .
Structural and functional changes in the CNS may influence the perception and generation of symptoms, with evidence of both gastric hypersensitivity and rectosigmoid hyposensitivity . Brock et al. investigated neurophysiological changes in a predominantly type 1 diabetes cohort and reported evidence of rectosigmoid hyposensitivity and bilateral anterior shifting of the insula and cingulate sources of brain activity, which correlated positively with postprandial fullness and nausea.
Lauras Story My First Symptoms
My first symptoms started six years prior to my diagnosis, Laura Marie told Diabetes Strong. Laura has lived with type 1 diabetes since 2002, when she was 16 years old. Her diabetic gastroparesis diagnosis was in 2014.
My symptoms of gastroparesis included nausea and vomiting, often feeling nauseous in the mornings and vomiting undigested food hours or ever even days after Id eaten it.
Laura says she had gradually become incredibly bloated. The bloating was severe enough that her clothing felt remarkably uncomfortable by the end of each day. And on top of bloating, she had started experiencing severe cramping and pain in her stomach.
My blood sugar levels also proved to be very erraticI would have a low blood sugar after eating, and a high blood sugar hours later, especially throughout the night.
By eventually wearing a Continuous Glucose Monitor , Laura says she could see the full evidence of her erratic overnight blood sugars.
The scariest part of her symptoms, though, was the increasingly frequent visits to the Emergency Room for DKA . Laura says she was usually admitted to the hospital about every 6 months because her unmanageable blood sugars would lead to DKA.
It was after being in DKA for what seemed like the hundredth time that I became so burnt-out, frustrated, and scared, that I told my healthcare professionals I was desperate for tests and a diagnosis.
Read Also: How Long After Eating To Test Blood Sugar
Complications Of Diabetic Gastroparesis
When your body isnt able to properly digest food, a variety of complications can developeven before youve been properly diagnosed with gastroparesis.
- Dehydration due to frequent vomiting
- Malnutrition due to poor absorption of nutrients in the food you eat
- Difficulty managing your blood sugar levels after eating
- Low-calorie intake or difficulty getting enough calories
- Bezoars
- Difficulty maintaining a healthy weight due to inability to eat enough
- Overall lower quality of life due to malnutrition and pain
Celiac Disease And Type 1 Diabetes

While it is unclear exactly what the relationship is, some research has found that those with celiac disease are more likely than the general population to develop type 1 diabetes. One 2015 study found that type 1 diabetes affected only 0.4% of the control subjects, but 3.2% of those with celiac disease.7
Read Also: How To Get Blood Sugar Down In A Hurry
The Kidneys And Urinary System
Over time, high blood sugar levels can damage blood vessels in the kidneys. This damage prevents the kidneys from filtering waste out of the blood. In time, kidney failure can result.
The NIDDK describe diabetes as one of the main causes of kidney disease. It affects 1 in 4 people with diabetes.
Diabetic nephropathy is kidney disease that affects people with diabetes. Learn more here.
Diabetes increases the risk of a number of eye problems, some of which can lead to vision loss.
Short-term problems include blurred vision, due to high blood sugar. Long-term complications include:
Symptoms Of Diabetic Gastroparesis
- Impaired oral drug absorption
- Spasms and cramping of the stomach wall
Its really important to discuss any distinct stomach or digestion issues with your healthcare team, says Susan Weiner, MS, RDN, CDE, CDN, FAADE and 2015 AADE Diabetes Educator of the Year. This may include chronic constipation, bloating, and recent spikes in your blood sugar levels that you dont understand or cant explain with the usual everyday challenges of diabetes management.
Weiner notes that she would hope any healthcare professional would create an open and non-judgmental environment for their patients because this can be a very uncomfortable situation for people with diabetes. Struggling with blood sugar management comes with its own inevitable layer of guilt and frustration, which means you need a healthcare team that can support you properly through a potential gastroparesis diagnosis.
Recommended Reading: Can You Be Born With Type 2 Diabetes
How Is Diabetic Gastroparesis Diagnosed
Your healthcare provider will feel your abdomen and ask about your diabetes. Tell him or her about all medicines you currently take. Certain medicines can affect how your digestive system works. Examples include opioids, tricyclic antidepressants, and certain COPD or asthma medicines. Some medicines used to treat type 2 diabetes may also affect your digestive system. Make sure your provider knows about all your current medicines. You may also need any of the following tests:
What Causes Gastroparesis
Gastroparesis is caused by nerve injury, including damage to the vagus nerve. In its normal state, the vagus nerve contracts the stomach muscles to help move food through the digestive tract. In cases of gastroparesis, the vagus nerve is damaged by diabetes. This prevents the muscles of the stomach and intestine from working properly, which keeps food from moving from the stomach to the intestines.
Anatomy of the stomach
Other causes of gastroparesis include:
- Viral infections.
- Gastric surgery with injury to the vagus nerve.
- Medications such as narcotics and some antidepressants.
- Amyloidosis and scleroderma .
Recommended Reading: Which Of The Following Insulins Are Used For Basal Dosage
Dm And Gi Smooth Muscle
Contractility of smooth muscle cells is altered in animal models of DM. Myocytes isolated from GI tracts of STZ-induced rat show increased expression Na, K-ATPase, leading to increased intracellular calcium level. In the same animal model, intracellular calcium binding proteins such as calmodulin and protein kinase C in intestinal smooth muscle cells are reduced. Similar changes are found in spontaneous diabetic rats, suggesting that diabetes alters smooth muscle contractility through changing the intracellular signaling pathways of intestinal myocytes. Another study, using both STZ-induced DM and spontaneous DM models, suggested that impairment in the function of GTP-binding proteins might be important in altered contractility of gastric smooth muscles, providing further evidence for the importance of DM induced changes in the intracellular signaling pathways. Myopathy and atrophy of gastric smooth muscle has also been reported,
Diabetes And Its Effect On Digestion
Diabetes can affect digestion in a number of ways. If diabetes has caused nerve damage, this can lead to nausea, constipation or diarrhoea.
An alternative cause of disturbed digestion can be the result of diabetes medication.
Some type 2 diabetes medications for instance are prone to causing digestive issues, although these tend to settle down after the body gets used to them.
You May Like: What Happens If You Have Diabetes
Dm And The Balance Of Excitatory And Inhibitory Neurotransmitters
The main excitatory neurotransmitter of enteric nervous system is acetylcholine followed by neurokinin and substance P that are released by enteric motor neurons and have receptors on ICC-IM, mediating the contraction of smooth muscles. Inhibitory neurotransmission in enteric nervous system happens through non-adrenergic non-cholinergic pathway. Nitric oxide is the main inhibitory neurotransmitter, with neuronal nitric oxide being the rate controlling enzyme in its production within ENS, . Studies of animal models with DM have demonstrated that the sources of nitrergic nerve terminals are both from intrinsic motor neurons and vagal and parasympathetic afferents. The distribution of nitrergic neurons is not equal throughout the GI tract, with them being more prevalent in the stomach and proximal parts of the intestine, .
Few studies in human patients with DM have confirmed the findings from animal models. Studying the gastric tissue obtained from patients with gastric cancer and DM revealed that the expression of nNOS is markedly decreased in the antrum, especially in the areas that have reduced density of ICC. In another study, we examined the colonic tissue obtained during colonoscopy from patients with and without diabetes and demonstrated that the population of nNOS containing enteric neurons is reduced. In addition to NO, other inhibitory neurotransmitters such as neuropeptide Y and vasoactive intestinal peptide are also reported to be reduced in DM.
How Can I Manage My Symptoms
- Walk after you eat. This may help speed digestion.
- Follow the meal plan that your healthcare or dietitian gave you. This meal plan can help decrease your symptoms. The following may also help you manage your symptoms:
- Eat less fat and fiber. High-fat and high-fiber foods may be hard for your stomach to digest. You may need to avoid fruits and vegetables such as oranges and broccoli.
- Eat 4 to 6 small meals a day. Smaller, more frequent meals are easier for your stomach to handle.
- Drink more liquids with your meals. Your healthcare provider may recommend liquid meals, such as soup. Liquid is easier to digest than solid food.
- Ask if you should prepare your food in a blender. Blended foods are easier to digest. Ask for directions on which foods to use and how to blend the food correctly.
- Ask about vitamins you may need and how to add them to your meals.
Recommended Reading: How To Dispose Of Insulin Pens

