Can Diabetes Cause Hair Loss
Yes, its possible for diabetes to cause hair loss. Uncontrolled diabetes can lead to persistently high blood glucose levels. This, in turn, leads to blood vessel damage and restricted flow, and oxygen and nutrients cant get to the cells that need it including hair follicles. Stress can cause hormone level changes that affect hair growth. If you have Type 1 diabetes, your immune system attacks itself and can also cause a hair loss condition called alopecia areata.
What Oral Medications Are Approved To Treat Diabetes
Over 40 medications have been approved by the Food and Drug Administration for the treatment of diabetes. Its beyond the scope of this article to review all of these drugs. Instead, well briefly review the main drug classes available, how they work and present the names of a few drugs in each class. Your healthcare team will decide if medication is right for you. If so, theyll decide which specific drug are best to treat your diabetes.
Diabetes medication drug classes include:
Many oral diabetes medications may be used in combination or with insulin to achieve the best blood glucose control. Some of the above medications are available as a combination of two medicines in a single pill. Others are available as injectable medications, for example, the GLP-1 agonist semaglutide and lixisenatide .
Always take your medicine exactly as your healthcare prescribes it. Discuss your specific questions and concerns with them.
Animal Models In Dm Type 1 Research
Animal models are used in autoimmune diabetes research to understand the pathogenesis and etiology of this disease, and to find and test predictive biomarkers and therapeutic interventions. Currently available models of T1D can be divided into spontaneously autoimmune, chemically induced, virus induced and genetically induced.
Spontaneous autoimmune
- Non-obese diabetic mouse
The NOD mouse is the best known and most widely used animal model for type 1 DM research. It is an inbred, genetically well characterized mouse strain that spontaneously develops T1D. The onset of insulitis occurs at 3â4 weeks of age. The islets of Langerhans are infiltrated by CD4+, CD8+ T lymphocytes, NK cells, B lymphocytes, dendritic cells, macrophages and neutrophils, similar to the disease process in humans. Insulitis leads to destruction of β-cells, resulting in the apparent occurrence of T1D, which varies by sex. The incidence is about 60-80% in females and 10-30% in males. In addition to sex, breeding conditions, gut microbiome composition or diet also influence the onset of T1D. NOD Mice are used to understand the pathogenesis and etiology of the disease, to identify novel autoantigens and biomarkers or to test new intervention strategies.
- BioBreeding Diabetes-Prone rat
- LEW -1AR1 / -iddm rat
Chemically induced
Genetically induced
Virally induced
You May Like: Dee Dee Blanchard Diabetes
What Are The Symptoms Of Type 1 Diabetes
Symptoms of type 1 diabetes are serious and usually happen quickly, over a few days to weeks. Symptoms can include
- increased thirst and urination
- trouble breathing
- trouble paying attention or feeling confused
DKA is serious and dangerous. If you or your child have symptoms of DKA, contact your health care professional right away, or go to the nearest hospital emergency room.
Other Specific Types Of Diabetes
Genetic defects of the -cell.
Several forms of diabetes are associated with monogenetic defects in -cell function. These forms of diabetes are frequently characterized by onset of hyperglycemia at an early age . They are referred to as maturity-onset diabetes of the young and are characterized by impaired insulin secretion with minimal or no defects in insulin action. They are inherited in an autosomal dominant pattern. Abnormalities at six genetic loci on different chromosomes have been identified to date. The most common form is associated with mutations on chromosome 12 in a hepatic transcription factor referred to as hepatocyte nuclear factor -1. A second form is associated with mutations in the glucokinase gene on chromosome 7p and results in a defective glucokinase molecule. Glucokinase converts glucose to glucose-6-phosphate, the metabolism of which, in turn, stimulates insulin secretion by the -cell. Thus, glucokinase serves as the glucose sensor for the -cell. Because of defects in the glucokinase gene, increased plasma levels of glucose are necessary to elicit normal levels of insulin secretion. The less common forms result from mutations in other transcription factors, including HNF-4, HNF-1, insulin promoter factor -1, and NeuroD1.
Genetic defects in insulin action.
Diseases of the exocrine pancreas.
Endocrinopathies.
Drug- or chemical-induced diabetes.
Infections.
Uncommon forms of immune-mediated diabetes.
You May Like: What Happens In Type 1 Diabetes
What Should I Expect If I Have Been Diagnosed With Diabetes
If you have diabetes, the most important thing you can do is keep your blood glucose level within the target range recommended by your healthcare provider. In general, these targets are:
- Before a meal: between 80 and 130 mg/dL.
- About two hours after the start of a meal: less than 180 mg/dL.
You will need to closely follow a treatment plan, which will likely include following a customized diet plan, exercising 30 minutes five times a week, quitting smoking, limiting alcohol and getting seven to nine hours of sleep a night. Always take your medications and insulin as instructed by your provider.
Older People With Diabetes
Older people need to follow the same general principles of diabetes managementâeducation, diet, exercise, and drugsâas younger people. However, risking hypoglycemia by trying to strictly control blood glucose levels may actually be harmful for people with multiple medical problems.
Managing diabetes can be more difficult for older people. Poor eyesight may make it hard for them to read glucose meters and dose scales on insulin syringes. They may have problems manipulating the syringe because they have arthritis or Parkinson disease or have had a stroke.
You May Like: Drugs To Lower A1c
How Are Type 1 And Type 2 Diabetes Diagnosed
The primary test used to diagnose both type 1 and type 2 diabetes is known as the A1C, or glycated hemoglobin, test.
This blood test determines your average blood sugar level for the past 2 to 3 months. Your doctor may draw your blood or give you a small finger prick.
The higher your blood sugar levels have been over the past few months, the higher your A1C level will be. Test results are expressed as a percentage. An A1C level of 6.5 percent or higher indicates diabetes.
The A1C test isnt accurate for people with sickle cell anemia or the sickle cell trait. If you have this condition or trait, then your doctor will have to use a different test.
What Are The Possible Complications
- Cardiac and blood vessel-related diseases
- Neuropathy
If you are wondering what is the most common diabetes the answer is diabetes type 2. People with type 2 diabetes do not make use of insulin well. Their body makes insulin but the cells dont use it the way it supposed to.
That is why type 2 diabetes is called insulin resistance diabetes or non-insulin dependent diabetes mellitus. It commonly affects middle-aged people although it can develop at any age.
You May Like: Can You Donate Blood If Your Diabetic
Newly Diagnosed With Type 1 Diabetes
It can be difficult to know where to get started with your new type 1 diagnosis, but were here to help you find the information you need.
As well as reading through the guidance and advice on this page, why not try our Learning Zone? With videos, quizzes and interactive tools tailored just for you, its the perfect way to discover more about your diabetes.
“She made me feel normal, when my normal had completely changed.”
– Laura, on being diagnosed with type 1 diabetes. Read her story.
What Should My Blood Glucose Level Be
Ask your healthcare team what your blood glucose level should be. They may have a specific target range for you. In general, though, most people try to keep their blood glucose levels at these targets:
- Before a meal: between 80 and 130 mg/dL.
- About two hours after the start of a meal: less than 180 mg/dL.
Read Also: What Regulates Insulin
Testing For Type 1 Diabetes
A simple blood test will let you know if you have diabetes. If youve gotten your blood sugar tested at a health fair or pharmacy, follow up at a clinic or doctors office to make sure the results are accurate.
If your doctor thinks you have type 1 diabetes, your blood may also be tested for autoantibodies that are often present with type 1 diabetes but not with type 2. You may have your urine tested for ketones , which also indicate type 1 diabetes instead of type 2.
Why Is My Blood Glucose Level High How Does This Happen
The process of digestion includes breaking down the food you eat into various different nutrient sources. When you eat carbohydrates , your body breaks this down into sugar . When glucose is in your bloodstream, it needs help a “key” to get into its final destination where it’s used, which is inside your body’s cells . This help or “key” is insulin.
Insulin is a hormone made by your pancreas, an organ located behind your stomach. Your pancreas releases insulin into your bloodstream. Insulin acts as the key that unlocks the cell wall door, which allows glucose to enter your bodys cells. Glucose provides the fuel or energy tissues and organs need to properly function.
If you have diabetes:
- Your pancreas doesnt make any insulin or enough insulin.
- Your pancreas makes insulin but your bodys cells dont respond to it and cant use it as it normally should.
If glucose cant get into your bodys cells, it stays in your bloodstream and your blood glucose level rises.
Recommended Reading: What Happens If You Stop Taking Diabetes Medication
How Is Diabetes Diagnosed
Diabetes is diagnosed and managed by checking your glucose level in a blood test. There are three tests that can measure your blood glucose level: fasting glucose test, random glucose test and A1c test.
- Fasting plasma glucose test: This test is best done in the morning after an eight hour fast .
- Random plasma glucose test: This test can be done any time without the need to fast.
- A1c test: This test, also called HbA1C or glycated hemoglobin test, provides your average blood glucose level over the past two to three months. This test measures the amount of glucose attached to hemoglobin, the protein in your red blood cells that carries oxygen. You dont need to fast before this test.
- Oral glucose tolerance test: In this test, blood glucose level is first measured after an overnight fast. Then you drink a sugary drink. Your blood glucose level is then checked at hours one, two and three.
| Type of test |
|---|
Complications Of Untreated Type 1 Diabetes
- kidney damage
- increased likelihood of infections such as thrush and also more serious infections
- damage to the eyes
- poor blood circulation in the legs and feet, potentially leading to lower limb amputation
- damage to the nerves of the feet
- much higher risk of heart disease and stroke
- sexual impotence.
Read Also: Glucagon Beta Cells
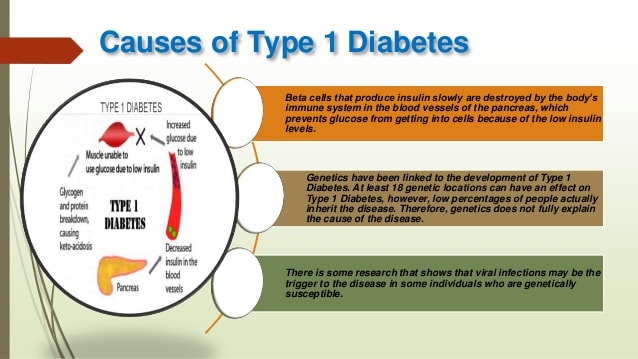
What Causes Type 1 Diabetes
Type 1 diabetes is thought to be caused by an autoimmune reaction that destroys the cells in the pancreas that make insulin, called beta cells. This process can go on for months or years before any symptoms appear.
Some people have certain genes that make them more likely to develop type 1 diabetes, though many wont go on to have type 1 diabetes even if they have the genes. Being exposed to a trigger in the environment, such as a virus, is also thought to play a part in developing type 1 diabetes. Diet and lifestyle habits dont cause type 1 diabetes.
How Can I Help My Child Live With Type 1 Diabetes
A type 1 diabetes diagnosis can be stressful for a child and his or her family. A younger child may not understand all the life changes, such as glucose monitoring and insulin injections. A child may feel:
- As if he or she is being punished
- Guilty
- Fearful of death
- Angry toward the parent
Parents can help their child by treating him or her as a normal child with diabetes management as just one aspect of their daily life.
Many areas have diabetes camps, support groups, and other organizations for children with type 1 diabetes and their families. Talk with your childs healthcare provider for more information.
Read Also: How Long Do Type 1 Diabetics Live
What Are The Possible Complications Of Type 1 Diabetes In A Child
Type 1 diabetes can cause:
- Ketoacidosis. This is when blood sugar levels are very high and the body starts making ketones. This is a very serious condition that needs to be treated right away in the hospital, sometimes in the intensive care unit. If your child is not treated right away, they are at risk for diabetic coma. A child with a diabetic coma loses consciousness because of brain swelling. The brain swells because of the very high blood sugar levels.
- Low blood sugar . This is also sometimes called an insulin reaction. This occurs when blood glucose drops too low.
Your childs healthcare provider will tell you how to avoid these problems.
Over time, high blood sugar levels can damage blood vessels. Balancing insulin, diet, and activity can help keep blood sugar levels in the target range and help prevent complications such as:
- Eye problems
- Heart and blood vessel disease
How Else Can I Manage Type 1 Diabetes
Along with insulin and any other medicines you use, you can manage your diabetes by taking care of yourself each day. Following your diabetes meal plan, being physically active, and checking your blood glucose often are some of the ways you can take care of yourself. Work with your health care team to come up with a diabetes care plan that works for you. If you are planning a pregnancy with diabetes, try to get your blood glucose levels in your target range before you get pregnant.
Don’t Miss: Metformin Maximum Dose Per Day
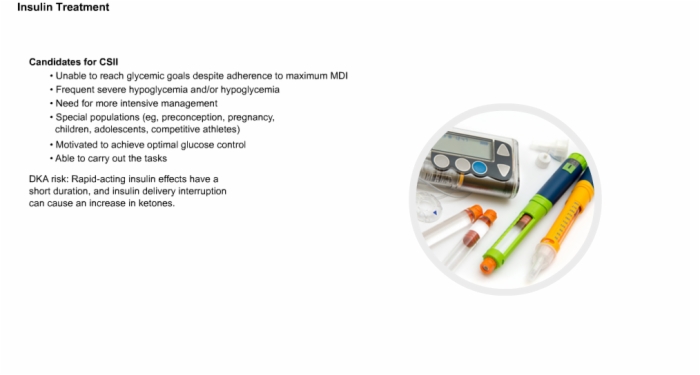
Treatment Of Type 1 Diabetes
- taking insulin daily by injections or by insulin pump
- self-monitoring of blood sugar levels by regularly testing droplets of blood in a glucose meter
- self-testing of urine with a test strip for high levels of ketones not routinely, but when problems are suspected
- regulating diet so intake is matched to insulin and exercise
- increasing the amount of slow carbohydrates in the diet, such as beans and fruit, which take longer to be absorbed by the body
- regular exercise
- maintaining regular checks for diabetes complications.
What Types Of Diabetes Require Insulin
People with Type 1 diabetes need insulin to live. If you have Type 1 diabetes, your body has attacked your pancreas, destroying the cells that make insulin. If you have Type 2 diabetes, your pancreas makes insulin, but it doesnt work as it should. In some people with Type 2 diabetes, insulin may be needed to help glucose move from your bloodstream to your bodys cells where its needed for energy. You may or may not need insulin if you have gestational diabetes. If you are pregnant or have Type 2 diabetes, your healthcare provider will check your blood glucose level, assess other risk factors and determine a treatment approach which may include a combination of lifestyle changes, oral medications and insulin. Each person is unique and so is your treatment plan.
You May Like: How Much Will Metformin Lower Blood Sugar
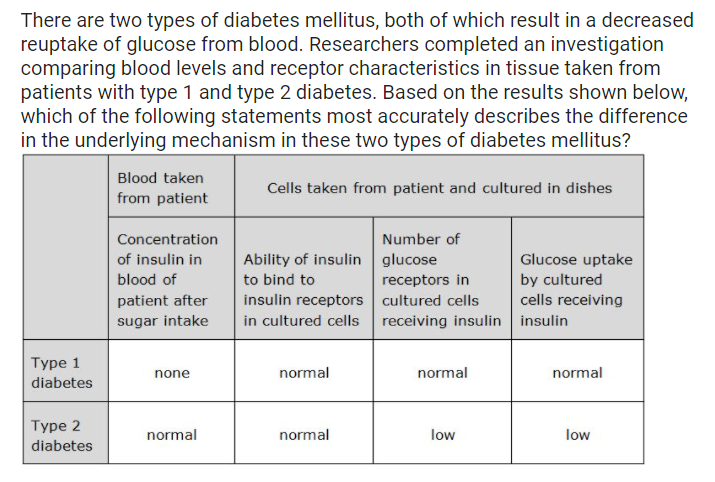
Definition And Description Of Diabetes Mellitus
Diabetes mellitus is a group of metabolic diseases characterized by hyperglycemia resulting from defects in insulin secretion, insulin action, or both. The chronic hyperglycemia of diabetes is associated with long-term damage, dysfunction, and failure of various organs, especially the eyes, kidneys, nerves, heart, and blood vessels.
Several pathogenic processes are involved in the development of diabetes. These range from autoimmune destruction of the -cells of the pancreas with consequent insulin deficiency to abnormalities that result in resistance to insulin action. The basis of the abnormalities in carbohydrate, fat, and protein metabolism in diabetes is deficient action of insulin on target tissues. Deficient insulin action results from inadequate insulin secretion and/or diminished tissue responses to insulin at one or more points in the complex pathways of hormone action. Impairment of insulin secretion and defects in insulin action frequently coexist in the same patient, and it is often unclear which abnormality, if either alone, is the primary cause of the hyperglycemia.
Symptoms of marked hyperglycemia include polyuria, polydipsia, weight loss, sometimes with polyphagia, and blurred vision. Impairment of growth and susceptibility to certain infections may also accompany chronic hyperglycemia. Acute, life-threatening consequences of uncontrolled diabetes are hyperglycemia with ketoacidosis or the nonketotic hyperosmolar syndrome.
How Are Type 1 And Type 2 Diabetes Treated
Theres no cure for type 1 diabetes. People with type 1 diabetes dont produce insulin, so it must be regularly injected into the body.
Some people take injections into soft tissue, such as the stomach, arm, or buttocks, several times per day. Other people use insulin pumps. Insulin pumps supply a steady amount of insulin into the body through a small tube.
Blood sugar testing is an essential part of managing type 1 diabetes, because levels can go up and down quickly.
Type 2 diabetes can be managed and even reversed with diet and exercise alone, but many people need extra support. If lifestyle changes arent enough, your doctor may prescribe medications that help your body use insulin more effectively.
Monitoring your blood sugar is an essential part of type 2 diabetes management too. Its the only way to know if youre meeting your target levels.
Your doctor may recommend testing your blood sugar occasionally or more frequently. If your blood sugar levels are high, your doctor may recommend insulin injections.
Read Also: Which Pancreatic Cells Release Insulin And Glucagon

