Physiologic Effects Of Insulin
Stand on a streetcorner and ask people if they know what insulin is, and many will reply, “Doesn’t it have something to do with blood sugar?” Indeed, that is correct, but such a response is a bit like saying “Mozart? Wasn’t he some kind of a musician?”
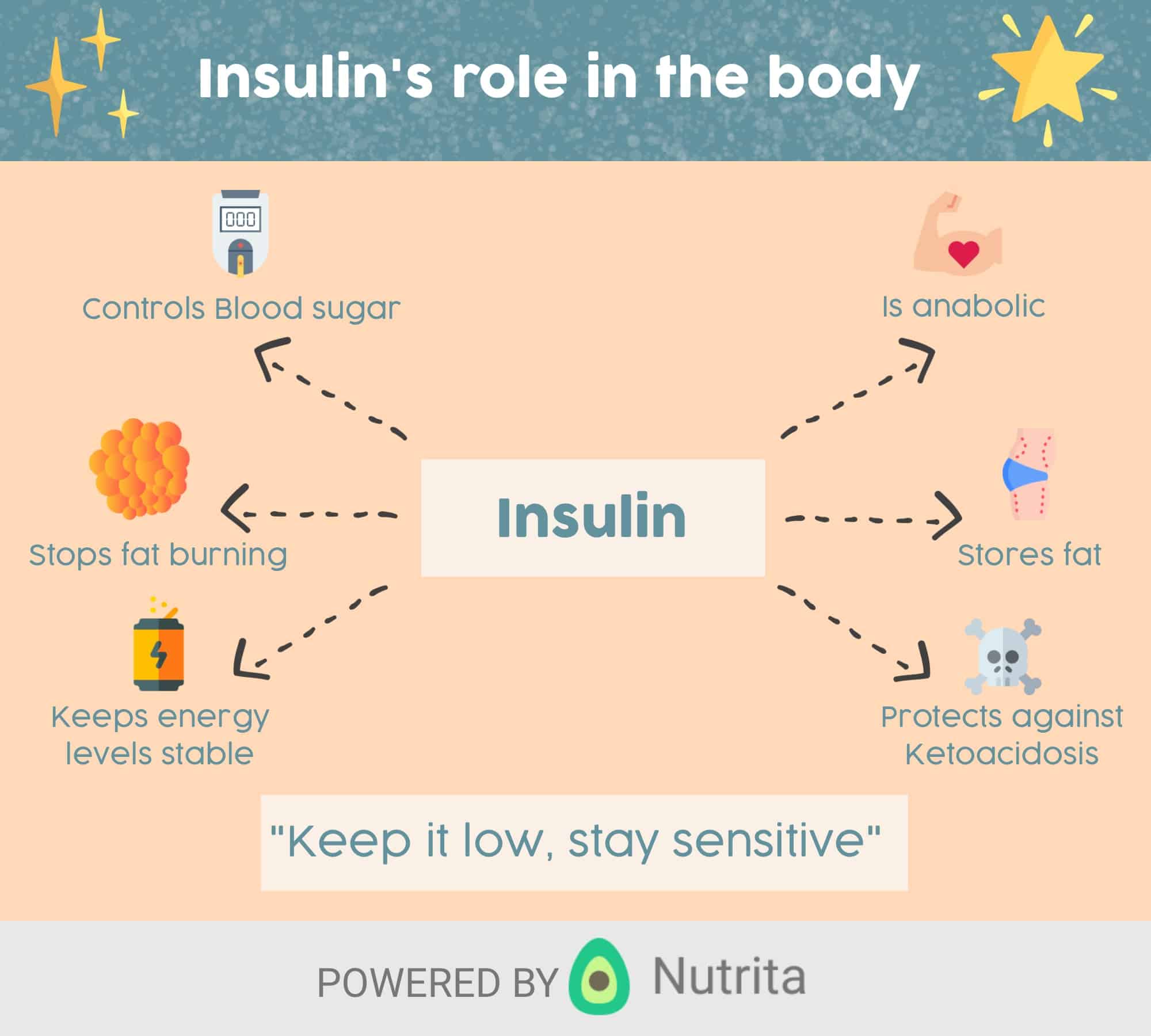
Insulin is a key player in the control of intermediary metabolism, and the big picture is that it organizes the use of fuels for either storage or oxidation. Through these activities, insulin has profound effects on both carbohydrate and lipid metabolism, and significant influences on protein and mineral metabolism. Consequently, derangements in insulin signalling have widespread and devastating effects on many organs and tissues.
The Insulin Receptor and Mechanism of Action
Like the receptors for other protein hormones, the receptor for insulin is embedded in the plasma membrane. The insulin receptor is composed of two alpha subunits and two beta subunits linked by disulfide bonds. The alpha chains are entirely extracellular and house insulin binding domains, while the linked beta chains penetrate through the plasma membrane.
Insulin and Carbohydrate Metabolism
It should be noted here that there are some tissues that do not require insulin for efficient uptake of glucose: important examples are brain and the liver. This is because these cells don’t use GLUT4 for importing glucose, but rather, another transporter that is not insulin-dependent.
Insulin and Lipid Metabolism
Other Notable Effects of Insulin
Insulin Resistance Effected By Hexosamines
The details of the hexosamine biosynthesis pathway and its role in metabolism and development can be found in the;Glycoproteins;page.
Numerous proteins involved in insulin signaling and the downstream targets of these signaling cascades have been shown to be;O-GlcNAcylated. With respect to insulin receptor signaling proteins, insulin receptor substrate-1 , phosphatidylinositol-3-kinase , protein kinase B/AK strain transforming , PIP3-dependent kinase 1 , and glycogen synthase kinase 3 are all known to be;O-GlcNAcylated. These modifications have all been observed in adipocytes which are a major target for the actions of insulin.
Insulin-stimulated glucose uptake into adipocytes occurs via insulin-mediated mobilization of GLUT4 to the plasma membrane. Increased glucose uptake, in response to insulin, can therefore, significantly modify the rate of flux through the HBP. Evidence linking the correlation between the HBP and insulin resistance in adipocytes was demonstrated at least 20 years ago. Using cultured rat adipocytes experiments demonstrated that chronic exposure to both insulin and glucose was required for the adipocytes to become insulin-resistant. This is now a common theme underlying insulin resistance in other insulin-sensitive tissues such as skeletal muscle.
Insulin And Type 2 Diabetes
Type 2 diabetes is characterised by the body not responding effectively to insulin. This is termed insulin resistance. As a result the body is less able to take up glucose from the blood. In the earlier stages of type 2 diabetes, the body responds by producing more insulin than it would normally need to.
If type 2 diabetes develops over a number of years, the extra demands on the pancreas to produce insulin can lead to a loss of insulin producing cells as they wear out.
Depending on their level of insulin resistance, people with type 2 diabetes; may also need to take insulin injections to manage their blood sugar levels.
You May Like: Does Type 1 Diabetes Skip A Generation
Why Does Insulin Need To Be Injected
Many people with diabetes often wonder why insulin, unlike many other common medications, cant simply be taken as a pill. The problem is because insulin is a complex protein, unlike most medications. The human digestive system is basically built around the task of breaking proteins down into simpler components, so trying to take an insulin pill would result in the insulin being broken down by the body before it enters the bloodstream.
Still, there is hope, and many companies and researchers are working on build a mechanism which would allow insulin in pill form to bypass the digestive process and not break down before it can be absorbed. Some of these efforts are reportedly quite close, and we might see insulin pills hit the market in the next decade or so, much to the delight of anyone who hates having to constantly stick themselves.
In the meantime, managing insulin doses with technology like the Timesulin insulin pen replacement cap can go a long way in helping to simplify the dosage process. And with diabetes technology expanding at a record pace, who knows where well be in ten years we may not have to worry about insulin doses at all!
The Release Of Insulin In Response To A Meal
The neat and tidy insulin responses described above only occur in laboratory settings. In the real world, the secretion of insulin stimulated by food intake proves far more difficult to predict due to the multitude of variables involved, such as:
- Presence of specific nutrients, including amino acids
- Physical makeup of the foods
- Rate of gastric emptying
- Speed of gastrointestinal motility
Furthermore, neural input as well as other digestive hormones such as incretin affect insulin response.
Specific nutrients produce distinct insulin responses. For instance, non-esterified fatty acids , which may come directly from high-fat foods or from the synthesis of excess carbohydrates, lead to increased output of glucose and reduce insulin sensitivity. There’s some indication, too, that they alter glucose-stimulated insulin secretionin the short-term, elevated levels of NEFA in the blood have been linked to increased glucose-stimulated insulin secretion, but chronically high levels of NEFA result in decreased glucose-stimulated insulin secretion as well as decreased insulin synthesis.
You May Like: How Do You Get Type 1 Diabetes
Regulation And Mechanisms Of Insulin Secretion At The Cellular Level
Synthesis and secretion of insulin is regulated by both nutrient and non-nutrient secretagogues, in the context of environmental stimuli and the interplay of other hormones. Nutrient secretagogues such as glucose appear to trigger insulin secretion from the cell by increasing intracellular ATP and closing of K+-ATP channels as outlined above. Generation of cyclic AMP and other cellular energy intermediates is also augmented, further enhancing insulin release. Glucose does not require insulin action to enter the cell . Non-nutrient secretagogues may act via neural stimuli such as cholinergic and adrenergic pathways, or through peptide hormones and cationic amino acids.
Neural Stimuli
1. Cholinergic Transmission
It has been well recognised that vagus nerve stimulation results in pancreatic insulin secretion. This is thought to mediate the so-called cephalic phase of insulin secretion, occurring when food is seen, smelled or acutely ingested. Islet cell cholinergic muscarinic receptors activate phospholipase C, with subsequent intracellular events activating protein kinase C, phospholipase A2 and mobilizing intracellular calcium. Insulin secretion by these mechanisms does not occur in the fasting state or if blood glucose levels are low, but may augment the anabolic response to feeding.
2. Adrenergic Pathway
Peptide Hormones
Amino Acids
Schematic presentation of insulin secretory pathways. Adapted from references: &.
Footnotes: Figure Abbreviations
DAG = diacylglycerol
What Causes Someone To Be Prescribed Insulin
If your body doesnt make insulin or doesnt make enough, you are eventually diagnosed with type 1 diabetes. It used to be called juvenile diabetes, but new estimates show that as many as half of people with type 1 diabetes are not diagnosed until adulthood. On the other hand, if your body doesnt use insulin properly, you have type 2 diabetes.
While people with type 1 diabetes need to take insulin to survive, many people with type 2 are able to stave off insulin use or even avoid it altogether by exercising, losing weight, adapting healthier eating habits, or using other prescription medications.
Also Check: What Is The Best Alcohol To Drink For A Diabetic
Insulin As Treatment For Diabetes
Injections of insulin can help treat both types of diabetes. The injected insulin acts as a replacement for or supplement to your bodys insulin. People with type 1 diabetes cant make insulin, so they must inject insulin to control their blood glucose levels.
Many people with type 2 diabetes can manage their blood glucose levels with lifestyle changes and oral medication. However, if these treatments dont help to control glucose levels, people with the condition may also need insulin to help control their blood glucose levels.
What Is The Function Of Insulin In The Human Body
Insulin helps in the metabolism of the body and without this hormone, we cannot live.
It depresses blood glucose levels in different ways including glycogen synthesis and increasing the cell consumption of glucose. It also stimulates the conversion of glucose into proteins and lipids, which reduces the level of glucose.
Insulin also inhibits the hydrolysis of glycogen in the liver and muscles.
Read Also: Is Whole Wheat Pasta Good For Diabetics
Clinical Syndromes Associated With Insulin Resistance
Type 2 diabetes and the Metabolic Syndrome would be the most common clinical syndromes associated with insulin resistance. Others include hypertension, PCOS, non-alcoholic fatty liver disease, certain forms of cancer and OSA, which some authors consider a component of the metabolic syndrome per se. There are also relatively common conditions where insulin resistance is a secondary phenomenon; these include acute illness, hepatic cirrhosis, renal failure, pregnancy, hyperthyroidism, Cushings disease and Cushings syndrome as well as acromegaly and phaeochromocytoma which are less common. In many of these, the insulin resistance is due to increased production of counter-regulatory hormones.
However there are also a large number of generally rare disorders where insulin resistance is a major clinical feature., Though individually rare, these conditions may provide insight into the mechanisms of insulin resistance in other settings. Typically they are characterised by disturbances in organ systems where insulin action plays a critical role.
Insulin And The Circulatory System
Insulin is secreted into the bloodstream and helps the cells of the body make use of glucose. It is the responsibility of the circulatory system to provide the insulin for all the cells of the body.; As long as enough insulin is produced by the body, the glucose is able to be used and the cells of the body thrive.
If there isnt enough insulin in the circulatory system, glucose levels go up and there can be complications, such as diabetic nephropathy , diabetic retinopathy , diabetic neuropathy , and heart disease.
A lack of insulin in the bloodstream results in starvation of the cells.; As the cells cant make use of glucose, they start to break down fat to be used as cellular fuel.; If glucose in the bloodstream becomes extremely high, ketones can build up in the body. Ketones are the metabolic byproduct of other sources of fuel the body is using.;; When ketones build up, there can be obvious symptoms, such as a dry mouth, nausea, vomiting, and a sweetness in the breath.; When this happens, it is called diabetic ketoacidosis.
Read Also: How Many Grams Of Sugar Can A Diabetic Have
Insulin And Fatty Acids
Insulin helps synthesize fatty acids in the liver cells.; If the glycogen levels make up at least 5 percent of the mass of the liver, the glycogen synthesis is suppressed and fatty acids are instead made by the liver to be used to make the lipid layer of the cells of the body.; The fatty acids are then taken out of the liver and are transferred to lipoproteins, which allow for the transportation of the fatty acids to make cells or to be stored inside fat cells as fat.
Factors Influencing Insulin Biosynthesis And Release

Insulin secretion may be influenced by alterations in synthesis at the level of gene transcription, translation, and post-translational modification in the Golgi as well as by factors influencing insulin release from secretory granules. Longer-term modification may occur via influences on cell mass and differentiation. Given insulins pivotal role in glucose utilisation and metabolism, it is not surprising that glucose has multiple influences on insulin biosynthesis and secretion. However, other factors such as amino acids, fatty acids, acetylcholine, pituitary adenylate cyclase-activating polypeptide , glucose-dependent insulinotropic polypeptide , glucagon-like peptide-1 , and several other agonists, together in combination, also influence these processes.
Also Check: Can You Be Born With Type 2 Diabetes
What Are The Different Types Of Insulin
The American Diabetes Association characterizes insulin by how fast it works. But everyones body is different. If you have diabetes, you should expect deviations in the amount of time any medication takes to reach your bloodstream.;
Here are 8 different types of Insulin and how they work.
- Onset;is defined as the length of time before insulin hits your bloodstream and begins to lower blood glucose.
- Peak;is the time during which insulin is at its maximum effectiveness at lowering your blood glucose levels.
- Duration;is the length of time insulin continues to lower your blood glucose levels.
- Rapid-acting insulin begins to affect blood glucose approximately 15 minutes after injection. It peaks in about an hour, and then continues to work for a few more.
- Short-acting insulin reaches your bloodstream within 30 minutes of injection. It peaks in the 2-3-hour range and stays effective for 3-6 hours.
- Intermediate-acting insulin includes NPH insulin which helps control glucose for 10-12 hours.;A;protamine;is a type of protein that slows the action of this insulin.
- Long-acting insulin enters the bloodstream 1-2 hours after injection and may be effective for as long as 24 hours. An advantage to long-acting insulin is there is no pronounced peak, and it works more like typical pancreatic insulin.
- Premixed/combination insulin contains a mix of rapid- or short-acting insulin combined with an intermediate-acting insulin. This eliminates the need to draw insulin from more than one bottle.
What Severe Complications Can Occur Because Of Rationing Or Running Out Of Insulin
Diabetic ketoacidosis is an emergency condition that results if you dont have enough insulin to regulate your blood sugar. DKA causes your body to break down fat for energy in the absence of insulin. This leads to a dangerous accumulation of acids known as ketones in your blood that can cause your brain to swell and your body to go into shock.
Signs of diabetic ketoacidosis include:;
- Thirst or a very dry mouth
- Frequent urination
- High levels of ketones in your urine
- Fatigue
- Nausea, vomiting, or stomach pain
- Difficulty breathing
- A fruity or acetone odor on your breath
- Confusion or acting drunk while sober
DKA is so common and can come on so quickly that it is the first sign of Type 1 diabetes in 20% of cases, and the way many type 1 diabetics are first diagnosed with the condition. If you go into diabetic ketoacidosis, dont try to hide it or make light of it. Treat it as the emergency it is and get to a hospital as soon as possible to recover. Ive had people tell me theyre tired of taking insulin, or that theyre rationing it due to cost. In type 1 diabetes, thats all it takes to end up in a life-threatening situation, says Dr. Zilbermint.
Another complication facing diabetics who use insulin is the potential for;hyperglycemia, also known as insulin shock, which involves using too much insulin and causing your blood sugar to drop extremely low. This can cause coma, seizures, and heart attacks, says Dr. Powers.
Read Also: How To Get Rid Of Insulin Resistance
Why Insulin Is Better Than Animals
Human insulin has been shown to have significant advantages over beef and pork extracted insulins. Patients who`ve switched to human insulin have shown significant decreases in anti-insulin antibody levels, making it easier to manage insulin allergies. Many people are also able to absorb it better than animal insulins.
Other Ligands For The Insulin Receptor
Insulin-like growth factors are so-called because they have significant structural homology with proinsulin but mainly mitogenic effects, significantly regulated by growth hormone. IGF-1 and 2 are coded for on the long arm of chromosome 12 and short arm of chromosome 11 respectively. They have specific receptors and bind with different affinities to the various IGF binding proteins. Insulin can bind to the receptors for IGF-1 and 2 but with much lower affinity respectively. IGF-1 binds weakly to the insulin receptor, with only 1.25×103 the affinity for the IGF-1 receptor; it binds the IGF-2 receptor with 1/4 the affinity for the IGF-2 receptor. IGF-2 does not bind to the insulin receptor; it does bind the IGF-1 receptor but with 1/3 the affinity for the IGF-2 receptor. Therefore overlap in physiological functions is more limited in vivo.
Recommended Reading: Which Of The Following Is Most Closely Related To Diabetes
Disorders Of The Endocrine System
Diabetes Mellitus
Dysfunction of insulin production and secretion, as well as the target cells responsiveness to insulin, can lead to a condition called diabetes mellitus. An increasingly common disease, diabetes mellitus has been diagnosed in more than 18 million adults in the United States, and more than 200,000 children. It is estimated that up to 7 million more adults have the condition but have not been diagnosed. In addition, approximately 79 million people in the US are estimated to have pre-diabetes, a condition in which blood glucose levels are abnormally high, but not yet high enough to be classified as diabetes.
There are two main forms of diabetes mellitus. Type 1 diabetes is an autoimmune disease affecting the beta cells of the pancreas. Certain genes are recognized to increase susceptibility. The beta cells of people with type 1 diabetes do not produce insulin; thus, synthetic insulin must be administered by injection or infusion. This form of diabetes accounts for less than five percent of all diabetes cases.
Watch the video to view an animation describing the role of insulin and the pancreas in diabetes.
Produced In The Pancreas
When you eat, food travels to your stomach and small intestines, where its broken down into nutrients that include glucose. The nutrients are absorbed and distributed via your bloodstream.
The pancreas is a gland located behind your stomach that performs an essential role in the digestion process. It creates enzymes that break down the fat, starches, and sugar in the food. It also secretes insulin and other hormones into your bloodstream.
Insulin is created in the beta cells of the pancreas. Beta cells comprise about 75% of pancreatic hormone cells.
Other hormones produced by the pancreas are:
- glucagon, which alerts your liver to raise your blood sugar if it gets too low
- gastrin, which stimulates the production of gastric acid in your stomach
- amylin, which helps control your appetite
Recommended Reading: Is Dragon Fruit Good For Diabetes

