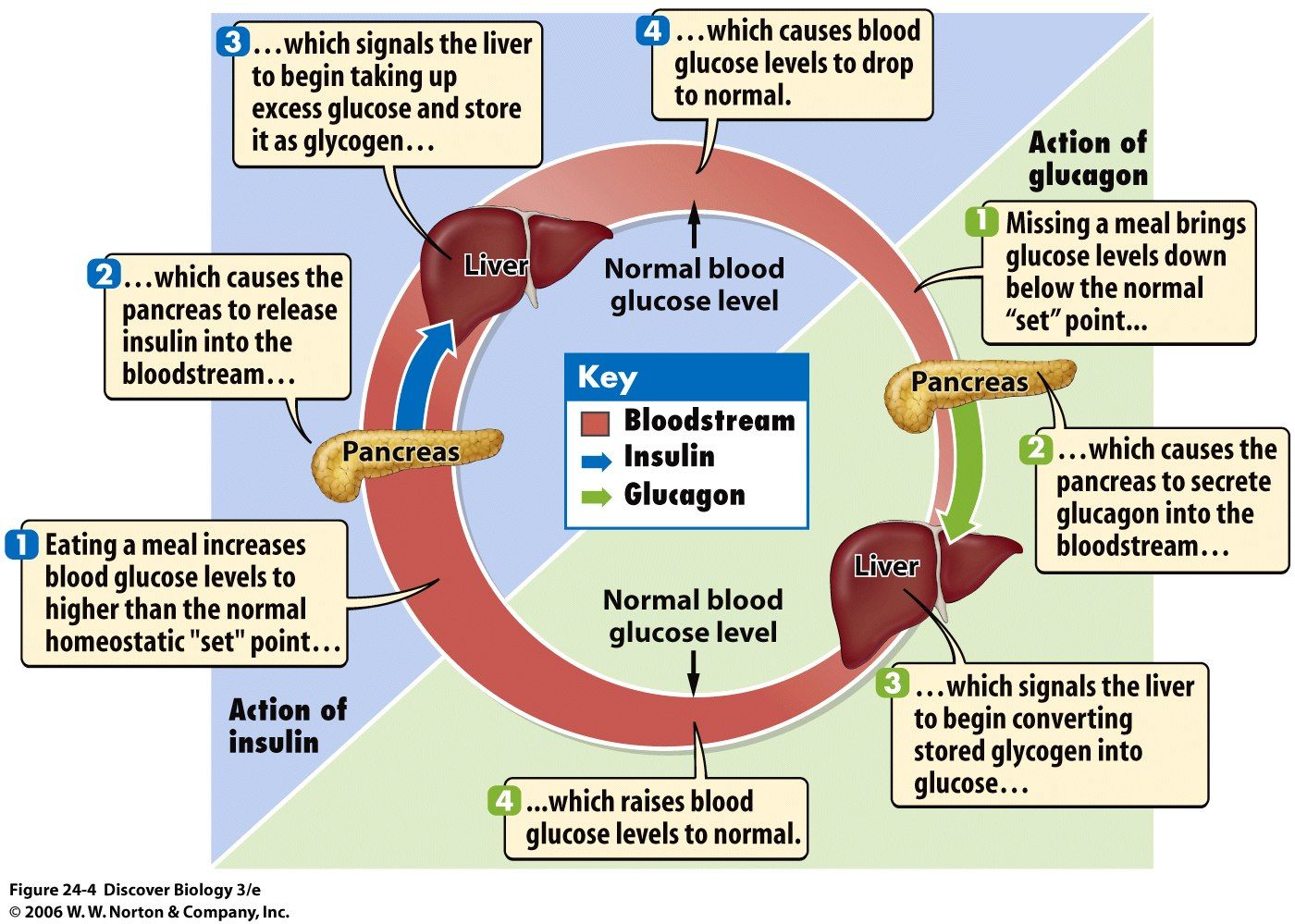
Regulation Of Blood Glucose Levels By Insulin And Glucagon
This animation describe the role of insulin and the pancreas in diabetes.
Figure 1. The main symptoms of diabetes are shown.
Impaired insulin function can lead to a condition called diabetes mellitus, the main symptoms of which are illustrated in Figure 1. This can be caused by low levels of insulin production by the beta cells of the pancreas, or by reduced sensitivity of tissue cells to insulin. This prevents glucose from being absorbed by cells, causing high levels of blood glucose, or hyperglycemia . High blood glucose levels make it difficult for the kidneys to recover all the glucose from nascent urine, resulting in glucose being lost in urine. High glucose levels also result in less water being reabsorbed by the kidneys, causing high amounts of urine to be produced this may result in dehydration. Over time, high blood glucose levels can cause nerve damage to the eyes and peripheral body tissues, as well as damage to the kidneys and cardiovascular system. Oversecretion of insulin can cause hypoglycemia, low blood glucose levels. This causes insufficient glucose availability to cells, often leading to muscle weakness, and can sometimes cause unconsciousness or death if left untreated.
Figure 2. Insulin and glucagon regulate blood glucose levels.
Common Conditions Associated With Insulin Resistance
Type 2 Diabetes
Following pioneering work by Bornstein and the Nobel Prize-winning work of Yalow and Berson, the first insulin assays became widely available in the late 1960s it was subsequently confirmed that diabetic patients with so-called or maturity onset or type 2 diabetes had normal or increased plasma insulin levels. Insulin resistance was reported to be a characteristic feature of T2DM in the early 1970s. A progressive inability of the cells to compensate for the prevailing insulin resistance by sufficient hyperinsulinaemia, heralds the clinical onset of this disorder. While twin studies and linkage analyses are consistent with a strong genetic component in the development of type 2 diabetes, several decades of research have failed to identify a predominant genetic abnormality in the majority of cases. The aetiology of T2DM is thought to be polygenic, with environmental factors being superimposed upon this basic predisposition.
Insulin resistance typically predates the development of diabetes and is commonly found in unaffected first-degree relatives. The morbidity of the disorder relates both to the severity of hyperglycaemia and the metabolic consequences of insulin resistance itself. The primary defects in insulin action appear to be in muscle cells and adipocytes, with impaired GLUT 4 translocation resulting in impaired insulin-mediated glucose transport.
Metabolic Syndrome
-
Abdominal obesity
Men < 40 mg/dL
Women < 50 mg/dL
Dyslipidaemia
Hypertension
PCOS
OSA
How Do You Take Insulin Without A Syringe
- Insulin pens look like large writing pens and can help prevent under- and overdosing. They also dont require refrigeration, are conveniently prefilled, and are more durable than syringes.
- Insulin pumps are attached to a thin tube thats implanted under your skin. Pumps are computerized or motorized, and some models also act as glucose monitors. They deliver insulin before each meal along with small amounts through the course of the day. In the US, about 60% of people with diabetes use some form of insulin pump.
- Jet injection devices are a good option if you hate needles. A jet injector holds several doses of insulin. After placing it against your skin, you press a button, and the insulin is pushed through.
- Inhalable insulin comes in a premeasured inhaler and was first approved in 2014. Its short-acting and usually not covered by insurance, which makes it more cost prohibitive than other types of insulin for most people with diabetes.
Unless you have an insulin pump that also works as a glucose monitor, insulin dosing is based on self-monitoring your blood glucose levels. You can check them by doing finger pricks or wearing a device that continuously monitors them for you.
Also Check: Prediabetes And Hypoglycemia
How Insulin Works In The Body
Insulin, a functional health balancing, and an essential hormone in the body play a vital role in regulating glucose levels in the blood. The organs make it called the pancreas. It helps the body to change blood sugar or glucose into energy. It also helps to store the excess glucose in the muscles, fat cells, and liver. This stored glucose can be used later whenever there is a lack of glucose in the body.
The lack of insulin or the bodys inability to respond to insulin will lead to a change in the quantity of sugar in the blood, leading to a condition called diabetes. In addition to the support in maintaining glucose level, it also helps to store fat.
Physiological Roles Of Insulin
The major purpose of insulin is to regulate the bodyâs energy supply by balancing micronutrient levels during the fed state . Insulin is critical for transporting intracellular glucose to insulin-dependent cells/tissues, such as liver, muscle, and adipose tissue. Any imbalance in exogenous energy supplies results in the breakdown of fats stored in adipose tissue and eventually accelerates insulin secretion. In the following sections, we discuss the major role of insulin in regulating several insulin-dependent tissue/organ functions.
Don’t Miss: Low Blood Sugar Disease
When To Contact A Medical Professional
- Chest pain or pressure, shortness of breath, or other signs of angina
- Loss of consciousness
Also call your provider if you have:
- Blood sugar levels that are higher than the goals you and your provider have set
- Numbness, tingling, or pain in your feet or legs
- Problems with your eyesight
- Sores or infections on your feet
- Frequent feelings of depression or anxiety
- Symptoms that your blood sugar is getting too low
- Symptoms that your blood sugar is too high
- Blood sugar readings that are below 70 mg/dL
You can treat early signs of hypoglycemia at home by drinking orange juice, eating sugar or candy, or by taking glucose tablets. If signs of hypoglycemia continue or your blood glucose level stays below 60 mg/dL , go to the emergency room.
The Insulin Resistance Syndrome
The insulin resistance syndrome describes the cluster of abnormalities which occur more frequently in insulin resistant individuals. These include glucose intolerance, dyslipidaemia, endothelial dysfunction and elevated procoagulant factors, haemodynamic changes, elevated inflammatory markers, abnormal uric acid metabolism, increased ovarian testosterone secretion and sleep-disordered breathing. Clinical syndromes associated with insulin resistance include type 2 diabetes, cardiovascular disease, essential hypertension, polycystic ovary syndrome, non-alcoholic fatty liver disease, certain forms of cancer and sleep apnoea.
Don’t Miss: Hypertension Related To Diabetes
What Is The Function Of Insulin In The Human Body
Insulin helps in the metabolism of the body and without this hormone, we cannot live.
It depresses blood glucose levels in different ways including glycogen synthesis and increasing the cell consumption of glucose. It also stimulates the conversion of glucose into proteins and lipids, which reduces the level of glucose.
Insulin also inhibits the hydrolysis of glycogen in the liver and muscles.
Regulation And Mechanisms Of Insulin Secretion At The Cellular Level
Synthesis and secretion of insulin is regulated by both nutrient and non-nutrient secretagogues, in the context of environmental stimuli and the interplay of other hormones. Nutrient secretagogues such as glucose appear to trigger insulin secretion from the cell by increasing intracellular ATP and closing of K+-ATP channels as outlined above. Generation of cyclic AMP and other cellular energy intermediates is also augmented, further enhancing insulin release. Glucose does not require insulin action to enter the cell . Non-nutrient secretagogues may act via neural stimuli such as cholinergic and adrenergic pathways, or through peptide hormones and cationic amino acids.
Neural Stimuli
1. Cholinergic Transmission
It has been well recognised that vagus nerve stimulation results in pancreatic insulin secretion. This is thought to mediate the so-called cephalic phase of insulin secretion, occurring when food is seen, smelled or acutely ingested. Islet cell cholinergic muscarinic receptors activate phospholipase C, with subsequent intracellular events activating protein kinase C, phospholipase A2 and mobilizing intracellular calcium. Insulin secretion by these mechanisms does not occur in the fasting state or if blood glucose levels are low, but may augment the anabolic response to feeding.
2. Adrenergic Pathway
Peptide Hormones
Amino Acids
Schematic presentation of insulin secretory pathways. Adapted from references: & .
Footnotes: Figure Abbreviations
DAG = diacylglycerol
Read Also: Liver Glucagon
Maintains Amino Acid Uptake
Another function or role of insulin is that it compels cells the absorb of circulating amino acids. A decrease in insulin levels inhibits this absorption. Individuals with low insulin levels have high blood amino acids. Introducing insulin in their systems brings down amino acid levels in the blood to normal values. In other words, insulin promotes the synthesis or metabolism of protein from circulating amino acids.
What Severe Complications Can Occur Because Of Rationing Or Running Out Of Insulin
Diabetic ketoacidosis is an emergency condition that results if you dont have enough insulin to regulate your blood sugar. DKA causes your body to break down fat for energy in the absence of insulin. This leads to a dangerous accumulation of acids known as ketones in your blood that can cause your brain to swell and your body to go into shock.
Signs of diabetic ketoacidosis include:
- Thirst or a very dry mouth
- Frequent urination
- High levels of ketones in your urine
- Fatigue
- Nausea, vomiting, or stomach pain
- Difficulty breathing
- A fruity or acetone odor on your breath
- Confusion or acting drunk while sober
DKA is so common and can come on so quickly that it is the first sign of Type 1 diabetes in 20% of cases, and the way many type 1 diabetics are first diagnosed with the condition. If you go into diabetic ketoacidosis, dont try to hide it or make light of it. Treat it as the emergency it is and get to a hospital as soon as possible to recover. Ive had people tell me theyre tired of taking insulin, or that theyre rationing it due to cost. In type 1 diabetes, thats all it takes to end up in a life-threatening situation, says Dr. Zilbermint.
Recommended Reading: Can Diabetics Eat Macaroni And Cheese
As An Anabolic Hormone
Remember that insulin is an anabolic hormone as well because it promotes the conversion of small molecules in the blood, such as glucose, fats, and amino acids, into large molecules inside cells. Because of this role, insulin also functions by decreasing proteolysis or the breaking down of protein into smaller polypeptides or amino acids, autophagy or the level of degradation of damaged cellular organelles, and lipolysis or breakdown of fats into glycerol and free fatty acids. While insulin promotes the storage of energy as fats into fat tissues, thus leading to fat accumulation in the body, proper weight management through nutrition and physical training can also promote storage of energy as proteins in the muscles, thus leading to muscle growth.
Structural Analysis And Synthesis
![Glucose Regulation in Human Body [28] Glucose Regulation in Human Body [28]](https://www.livingwithdiabetes.info/wp-content/uploads/glucose-regulation-in-human-body-28-download-scientific-diagram.png)
Purified animal-sourced insulin was initially the only type of insulin available for experiments and diabetics. John Jacob Abel was the first to produce the crystallised form in 1926. Evidence of the protein nature was first given by Michael Somogyi, Edward A. Doisy, and Philip A. Shaffer in 1924. It was fully proven when Hans Jensen and Earl A. Evans Jr. isolated the amino acids phenylalanine and proline in 1935.
The amino acid structure of insulin was first characterized in 1951 by Frederick Sanger, and the first synthetic insulin was produced simultaneously in the labs of Panayotis Katsoyannis at the University of Pittsburgh and Helmut Zahn at RWTH Aachen University in the mid-1960s.Synthetic crystalline bovine insulin was achieved by Chinese researchers in 1965. The complete 3-dimensional structure of insulin was determined by X-ray crystallography in Dorothy Hodgkin‘s laboratory in 1969.
Two other Nobel Prizes have been awarded for work on insulin. British molecular biologist Frederick Sanger, who determined the primary structure of insulin in 1955, was awarded the 1958 Nobel Prize in Chemistry.Rosalyn Sussman Yalow received the 1977 Nobel Prize in Medicine for the development of the radioimmunoassay for insulin.
Read Also: Increasing Metformin Dosage Side Effects
Role Of Insulin In Body
Insulin has a significant role in the metabolism of the body. It mainly regulates the storage of sugar and fat. The body cells mainly depend on glucose for uptaking glucose from the blood for the utilization of energy. Insulin will adjust the bodys glucose level by giving a signal to the fat cells and muscles to take glucose available in the blood. This glucose can be converted to energy. If excess glucose or sufficient glucose needed to be converted to life, insulin signals the liver to absorb the glucose and turn it into glycogen, stored.
The human liver can store up to 5% of its mass as glycogen. Most of the cells need glucose to take insulin, but some can do it even without insulin. It is an anabolic hormone which helps in glycogenesis, glucose uptake, lipogenesis. It also helps in the protein synthesis of skeletal muscle and fat tissue through the tyrosine kinase receptor pathway. In addition to this, it is an essential factor in the optimization of plasma glucose homeostasis. It generally counteracts hormones like Glucagon, other Catabolic Hormones like growth Hormones, Glucocorticoid, and Epinephrine.
Produced In The Pancreas
When you eat, food travels to your stomach and small intestines, where its broken down into nutrients that include glucose. The nutrients are absorbed and distributed via your bloodstream.
The pancreas is a gland located behind your stomach that performs an essential role in the digestion process. It creates enzymes that break down the fat, starches, and sugar in the food. It also secretes insulin and other hormones into your bloodstream.
Insulin is created in the beta cells of the pancreas. Beta cells comprise about 75% of pancreatic hormone cells.
Other hormones produced by the pancreas are:
- glucagon, which alerts your liver to raise your blood sugar if it gets too low
- gastrin, which stimulates the production of gastric acid in your stomach
- amylin, which helps control your appetite
You May Like: Does Metformin Increase Insulin Secretion
Insulin And Type 2 Diabetes
Type 2 diabetes is characterised by the body not responding effectively to insulin. This is termed insulin resistance. As a result the body is less able to take up glucose from the blood. In the earlier stages of type 2 diabetes, the body responds by producing more insulin than it would normally need to.
If type 2 diabetes develops over a number of years, the extra demands on the pancreas to produce insulin can lead to a loss of insulin producing cells as they wear out.
Depending on their level of insulin resistance, people with type 2 diabetes may also need to take insulin injections to manage their blood sugar levels.
The Mapk Signaling Pathway
The MAPK pathway is activated when IRS-1 binds to growth factor receptor-bound protein 2 . SOS binds to Grb2 and then to Ras, causing GDPâGTP exchange and the activation of Ras.
Activated Ras recruits c-Raf, which phosphorylates and activates MAPK/Erk kinase . MEK then phosphorylates extracellular signal-regulated kinase . Once activated, Erk is translocated to the nucleus, where its subsequent phosphorylation and transcriptional activation by transcription factors, such as ELK1, ultimately promote cell division, protein synthesis, and cell growth .
You May Like: Glipizide / Metformin Side Effects
What Are The Complications Of Insulin Resistance
The majority of the complications that can result from insulin resistance are related to the development of vascular complications due to elevated blood sugar levels and elevated insulin levels .
Not everyone who has insulin resistance will have complications. If youve been diagnosed with insulin resistance, Type 2 diabetes or metabolic syndrome, its important to see your healthcare provider regularly and follow your treatment plan to try to prevent these complications.
When Should I See My Healthcare Provider About Insulin Resistance
If youve been diagnosed with insulin resistance or conditions related to insulin resistance, its important to see your healthcare provider regularly to make sure your blood sugar levels are in a healthy range and that your treatment is working.
If youre experiencing symptoms of high blood sugar or prediabetes, contact your healthcare provider. They can run simple tests to check your blood sugar levels.
If you have a family history of diabetes or conditions that can cause insulin resistance, talk to your healthcare provider about your risk of developing insulin resistance.
Also Check: High Blood Pressure And Low Blood Sugar Symptoms
Evolution And Species Distribution
Insulin may have originated more than a billion years ago. The molecular origins of insulin go at least as far back as the simplest unicellular eukaryotes. Apart from animals, insulin-like proteins are also known to exist in the Fungi and Protista kingdoms.
Insulin is produced by beta cells of the pancreatic islets in most vertebrates and by the Brockmann body in some teleost fish.Cone snailsConus geographus and Conus tulipa, venomous sea snails that hunt small fish, use modified forms of insulin in their venom cocktails. The insulin toxin, closer in structure to fishes’ than to snails’ native insulin, slows down the prey fishes by lowering their blood glucose levels.
How Insulin Is Made
Insulin is produced by the pancreas, a gland-like organ nestled in the curve of the duodenum , just behind the stomach. The pancreas functions both as an exocrine gland and an endocrine gland.
The exocrine function of the pancreas is to help with digestion. The endocrine function of the pancreas is to produce insulin and another hormone called glucagon that helps regulate blood sugar. The pancreatic cells that produce glucagon are called alpha cells.
Insulin is produced by specialized beta cells in the pancreas, which are clustered into groups called islets of Langerhans, or islets for short. A healthy adult pancreas has approximately one million islets, composing about 5% of the entire organ.
Read Also: Journal Articles On Type 2 Diabetes

