General Sick Day Rules
- patients are advised to drink lots of fluids to stay hydrated. To avoid dehydration, patients should have small sips every 15 minutes or so throughout the day if they are having trouble keeping water down
- hands should be washed, and injection/infusion and finger-stick sites should be cleaned with soap and water or rubbing alcohol
- recommendations of local authority should be followed if suspected of COVID-19 symptoms.
Table : The Five Is That Cause Diabetic Ketoacidosis And Hyperosmolar Hyperglycemic State
Infection
Non-compliance with diabetic diet
Insulin lack
Pump failure, skipping insulin doses
The most common external cause of DKA is infectionusually a urinary tract infection, but diabetics are also at risk for pneumonia, cellulitis and more invasive skin infections.3
Infarction of any type of tissue can also lead to DKA. These include myocardial infarctions and cerebral infarctions . Less commonly, bowel ischemia can lead to DKA. Thus, adult patients over the ages of 3040 with suspected DKA should be questioned for any symptoms consistent with myocardial ischemia or infarction.
Type 1 diabetics may not have chest pain with acute MI, and may present with shortness of breath, weakness or other subtler symptoms, such as isolated nausea and vomiting, and should have a 12-lead ECG performed when appropriate.
A rapid stroke exam should also be performed in patients with weakness, visual changes, and any other stroke-like symptoms or altered mental status.
Pregnancy can cause DKA due to an increased insulin requirement. All females of childbearing age should be questioned about their pregnancy status.
Indiscretion with sugar, going off a diabetic diet, or use of alcohol can cause DKA when patients take in too many calories without accounting for them with appropriate doses of increased insulin.
As insulin levels decline, blood glucose levels increase, because cells cant transport glucose across their membranes without insulin.
How Should One Approach The Care Of A Minimally Responsive Patient
No matter how likely a psychiatric cause for unresponsiveness may seem, the life-threatening causes of stupor and coma must be considered first. The basic tenets of emergency care should be followed. If there is any indication of trauma, the cervical spine should be immobilized. Administration of thiamine, glucose, and naloxone should be strongly considered as rapid empiric treatments for the unresponsive patient.
One should then consider a broad differential diagnosis of stupor and coma that includes the following:
In the case of Ms. H, some, but not all, of these potential causes of stupor were evaluated. The primary treatment team might have considered checking thyroid function, arterial blood gas, cardiac enzymes, and carboxyhemoglobin level, as well as a human immunodeficiency virus test. A lumbar puncture could have been considered , especially if the patient was immunocompromised.
Given that Ms. H’s symptoms thus far involved primarily the CNS, more extensive evaluation of the brain was necessary. A magnetic resonance imaging scan, to evaluate more effectively the possibility of acute cortical stroke , would have been an important investigation. An electroencephalogram would also have been helpful.
Recommended Reading: Perfect A1c Level
Other Major Symptoms Include:
Blurred vision – a change in glucose absorption can bring about a change in the shape of the lens in the eye, leading to an altered vision quality. This can cause blurred vision, a common complaint that can indicate type 1 or type 2 diabetes.
Diabetic ketoacidosis – diabetic ketoacidosis occurs when the body begins to break down stores of fat as an alternative source of energy, leading to a build-up of acids in the blood known as ketones. This can result in weight loss and muscle wasting. Diabetic ketoacidosis is a rare and acute complication of diabetes, often requiring admission to ITU / HDU. Diabetic Ketoacidosis can result in coma and possibly death if left untreated. Symptoms of type 1 diabetes can develop quickly, over weeks or even days.
Type 1 & Type 2 Diabetes
The pathophysiology of Type 1 and Type 2 diabetes are actually quite different, although their names suggest two subtypes of the same disease.
Type 1 diabetes, previously called juvenile-onset diabetes, usually begins in childhood and is often familial. In Type 1 diabetes, the body has an absolute lack of insulin.
Type 2 diabetes, previously referred to as adult-onset diabetes, is distinct from Type 1 in that cells in the body become resistant to insulin, but there are still some cells that still produce insulin. Most patients with Type 2 diabetes are older and have comorbid conditions such as obesity and hypertension.1,2 Unfortunately, there are a growing number of obese adolescents who are developing this adult-onset disease relatively early in their lives.
Patients with Type 2 diabetes usually take oral medications vs. insulin for treatment, whereas patients with Type 1 diabetes require insulin replacement therapy. In both types of diabetes, uncontrolled hyperglycemia is damaging to virtually all body tissue.
Severe hypoglycemia usually occurs when glucose is < 50 mg/dL and can lead to rapid deterioration and death if not corrected promptly.
Also Check: Diabetics And Cheese
Disposition Of Patients With Hypoglycemia
In order to reasonably ensure no recurrence of hypoglycemia, all of the following criteria should be met prior to discharge of the patient from the Emergency Department:
-
The episode of hypoglycemia was:
-
Isolated
-
Completely and rapidly reversed without the need for a continuous dextrose infusion The result of an identified cause that is unlikely to cause recurrence
-
Accidental
-
Not caused by an oral hypoglycemic medication or long-acting insulin
And the patient:
Has completed an uneventful 4-hour observation period with serial blood glucose measurements in the normal range and not trending downward
Has eaten a full meal during the observation period
Has no comorbid conditions that interfere with proper administration of medications and intake of food
Understands how to prevent future episodes of hypoglycemia
Can accurately monitor blood glucose at home
Will be with a responsible adult who will monitor the patient
Has close, reliable follow-up with a primary care provider
Expert opinion states that patients who meet these criteria and are discharged from the emergency department should reduce their insulin dose by 25% for at least the next 24 hours to reduce the risk of recurrent hypoglycemia. Coordination with the patients primary care provider is essential.
Type 2 Diabetes And Insulin
People with Type 2 diabetes on insulin must:
- be provided with equipment to test their own blood glucose levels at home or/and once in the hospital
- aim to keep their blood glucose levels between 6 and 12mmol/L
- If their glucose levels remain above 12mmol/L when they are ill, they must follow advice on increasing insulin doses from the Diabetes Specialist
- extra blood glucose testing will be necessary. Glucose levels will need to be tested every four hours especially if blood glucose levels are high .
Don’t Miss: How To Lower Blood Sugar Overnight
Hyperosmolar Hyperglycemic Nonketotic Coma
HHNK is a true medical emergency, it usually occurs in older patients with type II or non-diagnosed diabetes. The syndrome is easily mistaken for diabetic ketoacidosis. But, HHNK differs from DKA in that their may be enough insulin present to prevent fat metabolism and the development of ketocacidosis as seen with DKA. However the amount of insulin may not be enough to prevent ;glucose use by the peripheral tissues or reduce glycogenesis by the liver.HHNK develops from sustained hyperglycemia that produces a hyperosmolar state. This is followed by an osmotic diuresis that results in marked dehydration and electrolyte losses. These patients often have an excessively high blood sugar level, up to 1000 mg/dl. This is considerably higher than DKA, simply because patients with HHNK are more dehydrated and have less ketone formation.;HHNK tends to develop slowly, often over the course of several days and has a higher mortality rate than other diabetic conditions.The early signs and symptoms ;of HHNK include:
- Volume depletion including polydipsia and polyuria
- Orthostatic hypotension
Precipitating factors of HHNK coma may include:
- Advanced age
- Inadequate insulin secretion
- Increased insulin requirements
- Certain medication
What Should Be The Aim For Blood Glucose Levels When A Person With Diabetes Is Ill
Aim:;Blood glucose target between 6-10mmol/L
Testing;
- if the blood glucose levels stay above 10mmol/L follow the individual prescribed guideline by the Diabetes Specialist for increasing their insulin dose
- extra blood glucose testing will be necessary. Glucose levels will need to be tested every two to four hours and every two hours if blood glucose levels remain high.
Also Check: How A Diabetic Can Lose Weight Fast
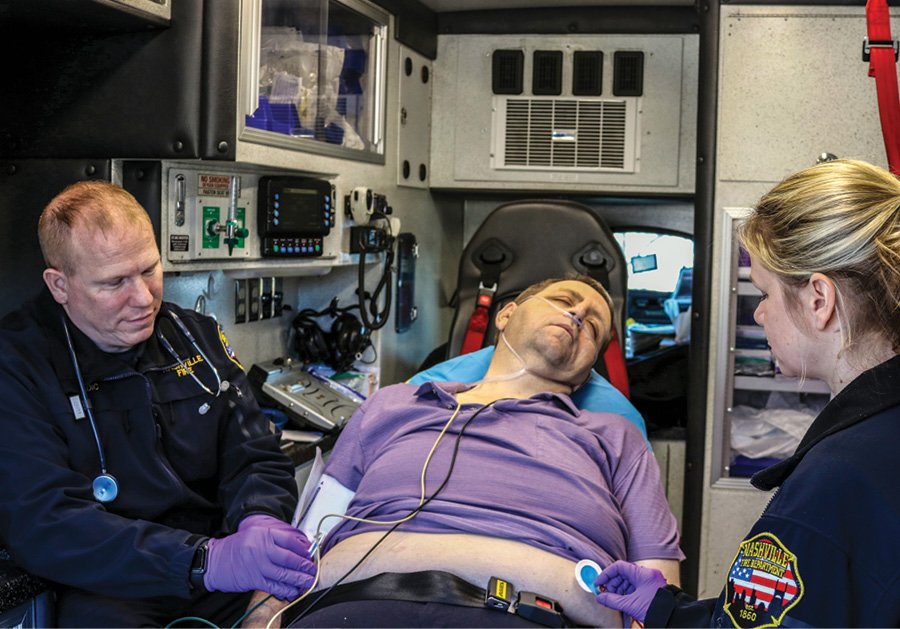
How Often Are Patients Transported After Hypoglycemia Treatment
Hypoglycemia is one of the patient encounters that often concludes with a non-transport after on-scene treatment. In this dataset of 50,000 diabetic emergency calls , just over half of patients were transported after on-scene treatment.
| Primary Impression | |
|---|---|
| Total | Not provided |
The decision to not transport a patient after treatment of hypoglycemia should be based on reassessment of:
- Patient’s blood sugar level after treatment.
- Patient’s mental status and capability for self-care and monitoring.
- Presence of friends and family capable of and willing to monitor patient.
- Local protocols allowing non-transport after on-scene treatment.
- Documentation of non-transport within the ePCR or as an addendum.
How Can Nursing Professionals Support Women With Diabetes To Plan Pregnancies
Pregnancy in diabetes should always be planned. This allows the MDT to protect mum and her baby from complications during pregnancy, delivery and beyond. Whilst all risk cannot be removed, planning a pregnancy allows mums and babys health to be protected before trying to conceive and so reduces these risks.
Pre-conception counselling should be a routine part of diabetes care for all women of childbearing age. They should all be advised to use contraception according to their preference and to approach their health care team before stopping contraception.
Preconception care for diabetes includes:
- reducing the risk of congenital abnormalities and miscarriage
- screening mum for complications of diabetes to manage them during the pregnancy
- managing blood glucose to a target HbA1c of 48 mmol/mol. One barrier to this is that hypoglycaemia becomes harder to avoid as blood glucose levels are reduced
- finding alternatives to medications known to be, or suspected of being harmful to the foetus
- and preparing mum for the time, effort and lifestyle adjustments required for pregnancy and diabetes.
Blood and urine tests should be organised. These will include:
- HbA1c
- U+Es and urinary ACR
The woman will need a medication review before conception. This will include:
Further resources
- tiredness.
Read Also: Is Milk Bad For Type 2 Diabetes
Interpreting A Pain Stimulus
If the patient doesn’t respond to a verbal stimulus attempt a pain stimulus with a pinch, squeeze or sternum rub.;
A sternum rub is the application of a painful stimulus with the knuckles of a closed fist to the center chest of a patient who is not alert and does not respond to verbal stimuli. The sternum rub is the most common painful stimulus practiced in the field by EMTs and paramedics. However, it is possible to misinterpret the patients response to the stimuli depending on the duration the pressure is applied.;
Learn how to correctly apply and interpret a sternum rub.;
What You Need To Do

Step 1 of 5: Open the airway
- Place one hand on the person’s forehead and gently tilt their head back. As you do this, the mouth will fall open slightly.
- Place the fingertips of your other hand on the point of the person’s chin and lift the chin.
Step 2 of 5: Check breathing
- Look, listen and feel for normal breathing – chest movement, sounds and breaths on your cheek. Do this for no more than ten seconds.
Step 3 of 5: Put them in the recovery position
- This will keep their airway open.
- Kneel down next to them on the floor.
- The next three steps are for if you find the person lying on their back. If you find them lying on their side or their front you may not need all three.
Step 4 of 5: If you suspect spinal injury
Step 5 of 5: Call for help
Read Also: How To Prepare For Gestational Diabetes Test
Which Patients Need Abcde
The ABCDE approach is applicable for all patients, both adults and children. The clinical signs of critical conditions are similar regardless of the underlying cause. This makes exact knowledge of the underlying cause unnecessary when performing the initial assessment and treatment. The ABCDE approach should be used whenever critical illness or injury is suspected. It is a valuable tool for identifying or ruling out critical conditions in daily practice. Cardiac arrest is often preceded by adverse clinical signs and these can be recognized and treated with the ABCDE approach to potentially prevent cardiac arrest. The ABCDE approach is also recommended as the first step in postresuscitation care upon the return of spontaneous circulation.
The ABCDE approach is not recommended in cardiac arrest. When confronted with a collapsed patient, first ensure the safety of yourself, bystanders, and the victim. Then check for cardiac arrest . If the victim is in cardiac arrest, call for help and start cardiopulmonary resuscitation according to guidelines. If the patient is not in cardiac arrest, use the ABCDE approach.
Glycemic Control After Hospitalization
There is vast discrepancy among Hospitalist regarding glycemic management goals throughout the US. This is despite data supporting improved patient outcomes and hospital stays. Recently studies have suggested that tight glycemic control in the hospital setting may lead to an increase in mortality due to hypoglycemia. However, the level of glycemic control in those studies was much tighter than recommended in the AACE/ADA guidelines for random blood glucose goals. It is common for Hospitalists to allow blood glucose levels to fluctuate during a patients hospital stay. The traditional Hospitalist training, primarily in an Internal Medicine residency program, often consists of treating diabetic patients with a regular insulin sliding scale. Diabetes management was not thought to be an issue of critical importance until blood sugars consistently were above 300 mg/dl or acidosis reared its head. The nature of Hospital Medicine is to be involved in all aspects patient care. Glycemic control should be viewed differently in lieu of data linking improved patient outcomes and eugylcemia.
The American Association of Clinical Endocrinologists and the American Diabetes Association published their revised consensus statement on the inpatient standards for glycemic control in 2009. Overall their guidelines had remained consistent with slight alterations in overall blood sugar levels. The following is a summary of those recommendations:
Non-critically ill patients
You May Like: What Happens If You Have Too Much Insulin
Hyperglycemia Without Obvious Acidosis
Patients with either Type 1 or Type 2 diabetes can present with hyperglycemia without ketosis or signs of HHS. These patients may be encountered early in the course of their DKA or HHS, and thus havent yet developed acidosis or hyperosmolarity, or they may just be chronically hyperglycemic.
Its also possible for patients to be hyperglycemic for a long period of time yet be unaware. For example, an undiagnosed Type 2 diabetic may develop hyperglycemia, polydipsia and polyuria over several weeks; although their blood glucose level may be well over 200 mg/dL, they may have no other symptoms or laboratory abnormalities.
Once diagnosed, its very important for diabetics to maintain euglycemia , since long-term hyperglycemia can lead to multiple complications including heart attack, stroke, blindness, neuropathy and extremity infections leading to amputations.
Causes: The causes of hyperglycemia without acidosis are the same as the causes with acidosisnamely the five Is.
Signs and symptoms: Whats important to note in hyperglycemia without acidosis is the lack of symptoms. Patients wont have Kussmaul breathing and their breath wont take on a fruity odor. Unless theres a CVA, there should be no neurologic abnormality and patients are generally well-appearing. The only clue may be polydipsia and polyuria, or just nonspecific complaints like weakness and fatigue.
Its important to consider whether the patient has signs or symptoms of an infection.
How Frequently Do Ems Providers Encounter Treat Hypoglycemia
Top takeaways for prehospital care of diabetic patients after filtering 2.5 million EMS encounters in the EMS Index
In a 180-day period spanning from late 2017-early 2018, EMS providers from more than 1,000 agencies responded more than 2.5 million times. About 50,000 of those calls were diabetic emergencies.
These response statistics, collected from the ESO EMS Index of real-world data, were shared with EMS1 by the ESO data analysis team to continue a discussion about the prehospital assessment and treatment of hypoglycemia, a common consequence of diabetes. Nearly 10 percent of the U.S. population has diabetes and an additional 84.1 million adults have prediabetes. Many other health conditions, including hypertension, heart disease, vision loss and mobility impairment, are worsened by diabetes. The total direct and indirect costs attributed to diabetes each year totals $322 billion.
Also Check: How To Mix Nph And Regular Insulin
Type I Insulin Dependent Diabetes Mellitus
You guessed it, IDDM Type I is characterized by the bodies inadequate insulin production by the pancreas. This type of diabetic presentation is somewhat rare, afflicting 1 in every 10 diabetic patients. It normally begins in the teens and young adult years but, can occur anytime after the patient is born. The disease is a autoimmune phenomenon resulting from genetic abnormalities that cause the body to destroy its own insulin producing beta cells. Patients with IDDM require life long insulin treatments, special diet , and exercise in order to lead a normal, healthy life.The symptoms of Type I IDDM will usually appear suddenly without warning and includes:
- Polyuria
- Polydipsia
- Dizziness
- Rapid, unexplained weight loss

