What Causes Gestational Diabetes Mellitus
Although the cause of GDM is not known, there are some theories as to why the condition occurs.
The placenta supplies a growing fetus with nutrients and water, and also produces a variety of hormones to maintain the pregnancy. Some of these hormones can have a blocking effect on insulin. This is called contra-insulin effect, which usually begins about 20 to 24 weeks into the pregnancy.
As the placenta grows, more of these hormones are produced, and the risk of insulin resistance becomes greater. Normally, the pancreas is able to make additional insulin to overcome insulin resistance, but when the production of insulin is not enough to overcome the effect of the placental hormones, gestational diabetes results.
Type 1 And Type 2 Diabetes
The risk of pregnancy complication for women with type 1 and type 2 diabetes is significantly greater than that of the general obstetric population and in women with gestational diabetes.12
Most importantly, the nadir for the rate of stillbirth for women with type 1 and type 2 diabetes was seen between 37 weeks and 38 weeks 6 days.13
Earlier delivery should be considered when end-organ complications are present, such as nephropathy, neuropathy and vasculopathy, or, when there is a poor obstetric history such as prior stillbirth.
Where significant fetal macrosomia is suspected in the presence of maternal diabetes, it is incumbent on clinicians to discuss the alternative of caesarean section, especially in light of the Montgomery v Lanarkshire case.14 While no guidelines go so far as to recommend caesarean delivery for any particular birth weight, the option of caesarean to prevent traumatic delivery could be considered when birth weight is estimated at greater than 4000â4500g.15
Planning For Labour And Delivery
Your diabetes in pregnancy team will work with you towards the ultimate goal of having a healthy baby. They will discuss what to expect during labour and birth, including a plan for managing blood glucose levels, insulin adjustment and who to contact if you go into labour earlier than expected.
Your diabetes in pregnancy team will work with you to aim for a natural birth close to your due date. It is usually recommended, that a woman with diabetes has her baby at around 3738 weeks gestation . If you do not come into spontaneous labour by then, your labour will be induced, or possibly an elective caesarean section will be suggested. The obstetrician in your diabetes in pregnancy team will discuss delivery options with you, with the goal usually being a vaginal birth. It is important that you feel comfortable discussing these birthing options with your team of health professionals.
If you go into labour spontaneously, it is best to go to hospital early for close monitoring of your diabetes and the babys well-being.
Sometimes, an earlier birth may be recommended if there are concerns during your pregnancy, such as:
- high blood pressure
- your baby becoming too big or not growing enough
- a substantial fall in your insulin requirements
- change in your babys patterns of movement.
You May Like: How Many Points Does Metformin Lower Blood Sugar
Risks Associated With Labor Induction
The increasing rate of labour induction, involving more than 20% of pregnancies in developed countries,, has stimulated the investigation of possible risks associated with this intervention. Perhaps, the most suitable model for assessing the effects of labour induction per se on pregnancy outcome is elective labor induction which refers to induction in the absence of any maternal or fetal indications. The main focus of most of the studies addressing this issue was the effect of labour induction on risk of CS. Other potential concerns associated with labour induction include fetal distress due to uterine hyperstimulation, chorioamnionitis and neonatal respiratory morbidity when induction takes place prior to 39 weeks of gestation.,,
Maternal Outcomes With Elective Induction Vs Expectant Management
The largest study to look at maternal outcomes included over 8,000 pregnant people with GDM. They found that inducing labor at 38 or 39 weeks for GDM is linked to a lower rate of Cesareans, less pre-eclampsia/hypertension, and more epidural use compared to expectant management at those times . When they looked exclusively at first-time mothers, there was no benefit to inducing labor at 38 weeks only 39-week induction was linked to a lower rate of Cesareans compared to following expectant management to 40+ weeks .
In another study, researchers also reported cervical ripeness and whether the mother had given birth before . These researchers found that people with GDM who had had a previous vaginal birth significantly increased their risk of Cesarean by attempting induction before 39 weeks, especially with an unripe cervix. Therefore, based on this and the Melamed et al. study, it appears that 38-week elective induction for gestational diabetes should not be routinely recommended to first-time or experienced mothers. In the Feghali et al. study, induction at 39 weeks gestation resulted in a similar Cesarean rate compared to expectant management at that time. After 40 weeks gestation, everyone experienced an increase in Cesareans, regardless of whether their labors were induced or spontaneous.
Why might Cesareans go up after 40 weeks?
Don’t Miss: How Many Points Does Metformin Lower Blood Sugar
Planned Birth At Or Near Term For Pregnant Women With Gestational Diabetes And Their Infants
What is the issue?
The aim of this Cochrane review was to find out if planning an elective birth at or near the term of pregnancy, compared to waiting for labour to start spontaneously, has an impact on the health of women with gestational diabetes and the health of their babies. Planned early birth means either induction of labour or caesarean birth, and ‘at or near term’ means 37 to 40 weeks’ gestation. To answer this question, we collected and analysed all relevant studies conducted up to August 2017.
Why is this important?
Women with gestational diabetes and their babies are at increased risk of health complications . Because of the complications sometimes associated with birthing a big baby, many clinicians have recommended that women with gestational diabetes have an elective birth at or near term rather than waiting for labour to start spontaneously, or until 41 weeks’ gestation if all is well. Induction has disadvantages of increasing the incidence of forceps or ventouse births, and women often find it difficult to cope with an induced labour. Caesarean section is a major operation which can lead to blood loss, infections and increased chance of problems with subsequent births. Early birth can increase the chance of breathing problems for babies. It is important to know which approach to birth has a better impact on the health outcomes of women with gestational diabetes and their babies.
What evidence did we find?
What does this mean?
Considerations Regarding Timing Of Delivery
The recommendations on timing of delivery, and thus induction, are informed primarily by cohort studies examining the risk of a particular outcome, such as caesarean section or stillbirth, occurring in a population of women with diabetes at each week of gestation, compared to women without any pregnancy complication.
Also Check: What Is A Normal A1c For A Non Diabetic
Who’s At Risk Of Gestational Diabetes
Any woman can develop gestational diabetes during pregnancy, but you’re at an increased risk if:
- your body mass index is above 30 use the healthy weight calculator to work out your BMI
- you previously had a baby who weighed 4.5kg or more at birth
- you had gestational diabetes in a previous pregnancy
- 1 of your parents or siblings has diabetes
- you are of south Asian, Black, African-Caribbean or Middle Eastern origin
If any of these apply to you, you should be offered screening for gestational diabetes during your pregnancy.
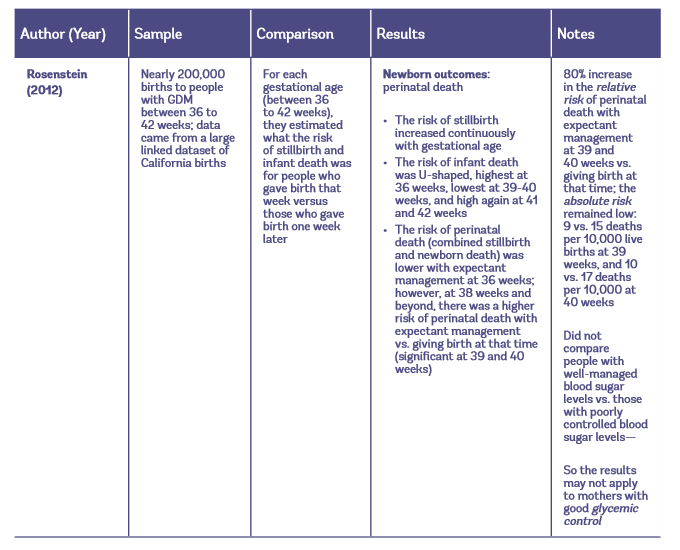
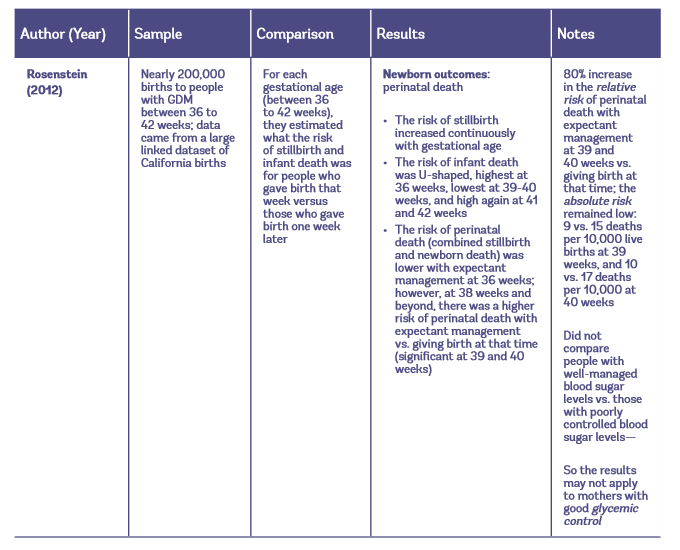
Labor Induction Versus Expectant Management In Diabetic Pregnancies Current Evidence
We discussed above the possible benefits of induction of labour in pregnancies complicated by diabetes, however, prior to translation into clinical practice this needs to be confirmed with experimental data. Furthermore, the general risks associated with labour induction that were described above may be less applicable to diabetic pregnancies that are confounded by higher birth weight and maternal obesity, which are likely to affect the risk of CS in cases of labour induction. In addition, the risk of neonatal respiratory morbidity when induction takes place prior to 39 weeks may be even higher in diabetic pregnancies, especially in the presence of poor glycemic control. Thus, the optimal balance between the benefits and risks of labour induction in diabetic pregnancies can be only determined empirically. Unfortunately, few studies on labour induction versus expectant management in diabetic pregnancies are available , only one of which is an RCT.
Read Also: What Happens If You Stop Taking Diabetes Medication
How Gestational Diabetes Can Affect Your Pregnancy
Most women with gestational diabetes have otherwise normal pregnancies with healthy babies.
However, gestational diabetes can cause problems such as:
- your baby growing larger than usual this may lead to difficulties during the delivery and increases the likelihood of needing induced labour or a caesarean section
- polyhydramnios too much amniotic fluid in the womb, which can cause premature labour or problems at delivery
- premature birth giving birth before the 37th week of pregnancy
- pre-eclampsia a condition that causes high blood pressure during pregnancy and can lead to pregnancy complications if not treated
- your baby developing low blood sugar or yellowing of the skin and eyes after he or she is born, which may require treatment in hospital
- the loss of your baby though this is rare
Having gestational diabetes also means you’re at an increased risk of developing type 2 diabetes in the future.
Screening For Gestational Diabetes
During your first antenatal appointment at around week 8 to 12 of your pregnancy, your midwife or doctor will ask you some questions to determine whether you’re at an increased risk of gestational diabetes.
If you have 1 or more risk factors for gestational diabetes you should be offered a screening test.
The screening test is called an oral glucose tolerance test , which takes about 2 hours.
It involves having a blood test in the morning, when you have not had any food or drink for 8 to 10 hours . You’re then given a glucose drink.
After resting for 2 hours, another blood sample is taken to see how your body is dealing with the glucose.
The OGTT is done when you’re between 24 and 28 weeks pregnant. If you’ve had gestational diabetes before, you’ll be offered an OGTT earlier in your pregnancy, soon after your booking appointment, then another OGTT at 24 to 28 weeks if the first test is normal.
Find out more about an OGTT.
Read Also: Metformin Overdose How Much
Obstetrical Considerations In Women With Pre
The goal of fetal surveillance and planned delivery in women with pre-existing diabetes in pregnancy is the reduction of preventable stillbirth. However, not all stillbirths can be avoided due to the fact that many stillbirths in pre-existing diabetes occur prior to 36 weeks of gestation and that in a large number of cases no obvious cause is noted . Despite this, it is reasonable to apply surveillance strategies to pre-existing diabetes pregnancies that are similar to those in other pregnancies at high risk of fetal complications, such as intrauterine growth restriction , chronic hypertension, and systemic lupus erythematosis . Although there is no single strategy for antenatal surveillance for pre-existing diabetes pregnancies, the initiation of some form of fetal surveillance in all women with pregnancies complicated by pre-existing diabetes while applying more intensive protocols for fetal surveillance in pregnancies with additional risk factors is required. These risk factors include: evidence of poor glycemic control, prepregnancy retinopathy , LGA, polyhydramnios or the presence of other comorbidities or high-risk conditions . As a general rule, intensified fetal surveillance should begin at a period in gestation when intervention is possible and acceptable to both the parents and the neonatal care providers.
Significance Of Decreasing Insulin Requirements
In contrast, results from other studies found no association with decreasing insulin requirements and birthweight, and neonatal weight distribution . However, 1 study observed a trend for greater LGA neonates in women with decreasing insulin requirements . Caution is required when interpreting the findings as researchers used differing calculation methods to indicate fall in insulin requirements or perhaps due to heterogeneity in the population of women with type 2 diabetes included in the studies. The use of advanced sonographic and fetal doppler assessment in the surveillance of the fetus at risk, as in other high-risk pregnancies, may allow further stratification of risk in this population, but the optimal indicator of feto-placental compromise, particularly in women with diabetes, remains unclear.
In summary, the impact of decreasing insulin requirements is still not certain. While fetal monitoring in this situation can provide reassurance of current fetal well-being, it should not be viewed as a substitute for a well thought out plan for timing of delivery that takes into consideration other risks for perinatal mortality, such as gestational age, maternal glycemic control , prepregnancy retinopathy , maternal age, obesity and smoking history.
Read Also: Squeezing Finger For Blood Sugar Test
Prevention And Risk Factors
The incidence of GDM is increasing worldwide. The global prevalence of hyperglycemia during pregnancy has been estimated at 16.9% using the World Health Organization criteria . A higher proportion of women entering pregnancy at an older age and/or with obesity contribute to this increase in prevalence, along with changes in screening strategies and diagnostic criteria. There is a need for an effective and acceptable intervention that will prevent the development of GDM. Such an approach has the potential to improve maternal and child health, with significant savings to the health-care system.
Understanding the pathophysiology of GDM and its risk factors is important for the development of preventive strategies. The GDM population includes a heterogeneous group of women with different metabolic profiles when exposed to pregnancy hormones. Various presentations include:
- Hyperglycemia that likely preceded the pregnancy , elevated first trimester fasting glucose, overt diabetes in pregnancy, monogenic diabetes)
- Reduced and/or falling insulin secretory capacity
- Significant insulin resistance from early pregnancy
- A combination of factors ).
Can Gestational Diabetes Cause Problems During Pregnancy
Yes. If not treated, GDM can cause pregnancy complications, including:
Gestational diabetes also can cause health complications for your baby after birth, including:
- Breathing problems, including respiratory distress syndrome . This is a breathing problem caused when babies dont have enough surfactant in their lungs. Surfactant is a protein that keeps the small air sacs in the lungs from collapsing.
- Jaundice. This is a medical condition in which a babys eyes and skin look yellow. A baby has jaundice when his liver isn’t fully developed or isnt working well.
- Low blood sugar
- Obesity later in life
You May Like: Type 1 Diabetes Low Blood Sugar What To Do
Targets Of Glycemic Control
Elevated BG levels have adverse effects on the fetus throughout pregnancy. At conception and during the first trimester, hyperglycemia increases the risk of fetal malformations and intrauterine fetal demise . Later in pregnancy, it increases the risk of macrosomia, fetal and infant death as well as metabolic and obstetrical complications at birth . As a result, meticulous glycemic control throughout pregnancy is required for optimal maternal and fetal outcomes.
An important first step in achieving optimal glycemic control is to set target BG levels . However, optimal targets for fasting, preprandial and postprandial BG levels in women with pre-existing diabetes have not been examined in randomized controlled trials and a variety of BG targets are used in clinical practice. Older studies confirm that the lower the mean BG, the better the outcome, with some suggesting a target mean BG < 6.7 mmol/L and, others, a mean < 6.9 mmol/L. A fasting BG target < 5.9 mmol/L is still associated with a 29% macrosomia rate . Recent retrospective data demonstrated that a mean A1C 6.0% in pregnant women with type 2 diabetes was associated with increased risk of neonatal complications compared to women with an A1C < 6.0% . In women with type 1 diabetes and good glycemic control during pregnancy with an A1C of 4.5% to 7.0%, there is still a linear relationship between third trimester A1C and risk of macrosomia .
My Induction Birth Stories Jo Author And Founder Of Gestational Diabetes Uk
I only know gestational diabetes I only know induction and so I cant say whether an induction is more painful etc as it is all I know. But I will share what my personal induction birth stories and experiences have been. Three gestational diabetes pregnancies with early diagnosis, despite losing 5 stone in weight, I still got diagnosed with gestational diabetes at 11 weeks in my second pregnancy and once again my levels shot up as soon as I fell pregnant with my third. I controlled my gestational diabetes each time with fairly high amounts of insulin, around 200 units a day in my first two and just over 400 units in my last pregnancy which I also suffered HG with. I required more fast release insulin in my first pregnancy and more slow release in my second and third.
In my first pregnancy, I struggled more with post meal readings. I was testing at 2 hours post meals and followed poor dietary advice as advised by my dietician.
In my second and third pregnancies, I had researched gestational diabetes in depth, was learning lots about the condition, had set up the Facebook support group and website and was testing my levels before meals, at one hour post meals, before bed, plus additionally to test snacks and for spikes. My post meal levels were very well controlled following my own dietary advice, but I chased my fasting levels throughout, having to increase my night time insulin every couple of days.
You May Like: Can You Be Born With Type 2 Diabetes
Gestational Diabetes Induction Birth Stories
Here we share some of our members gestational diabetes induction birth stories. With gestational diabetes, many ladies may be advised to have an induction of labour . Induction may be the unknown and for many ladies, a scary and daunting, unnatural process. Many ladies hear lots of horror stories surrounding induction and so its important to understand what is involved so that you can make an informed decision over whether you consent to induction or not.

