Ok But What Do They Have To Do With Each Other
Now you know insulin and glucagon have pretty similar jobs. But how do these hormones work together?
When theyre doing their jobs correctly, they work in perfect balance: Insulin prevents glucose levels from getting too high while glucagon prevents them from getting too low.
Both need to be effective for your blood sugar levels to stay, well, as close to perfect as possible.
When insulin and glucagon arent working correctly, things get complicated. If one or the other isnt properly regulating glucose levels, those levels will get thrown off, which can have some pretty serious side effects.
Regulation Of Glycogen Synthase
Glycogen synthase also has two forms, one active and one inactive form. In contrast to glycogen phosphorylase however, the active form is the dephosphorylated while the inactive form is phosphorylated. That means that phosphorylation of glycogen synthase will deactivate it, and dephosphorylating will activate it.
The regulation of glycogen synthase. CKII is casein kinase II. PP1 is protein phosphatase 1. GSK3 is glycogen synthase kinase 3.
Activators of;glycogen synthase
PP1 works on glycogen synthase as well as glycogen phosphorylase. By dephosphorylates glycogen synthase, PP1 activates it. PP1 is, in turn, activated by factors shown on the illustration to the right. PP1 is therefore the only regulator that directly regulates both;glycogen synthase;and glycogen phosphorylase.
Inactivators of;glycogen synthase
The phosphorylation of;glycogen synthase;is regulated by multiple enzymes. The first one is glycogen synthase kinase 3 , which phosphorylates glycogen synthase, deactivating it. However, GSK3 doesnt work without another kinase, called;casein kinase II;. CKII primes;glycogen synthase, which is necessary for GSK3 to work.
Insulin activates another protein kinase, called protein kinase B . PKB phosphorylates GSK3, inhibiting it. Insulin also activates PP1, which dephosphorylates glycogen synthase, activating it. Insulin therefore activates glycogen synthase, as it inhibits that which inhibits it.
Allosteric regulation of;glycogen synthase
Regulation Of Glucagon Action
Clearly, insulin replacement therapy has been an important step towardrestoration of glucose homeostasis. But it is only part of the ultimatesolution. The vital relationship between insulin and glucagon has suggestedadditional areas for treatment. With inadequate concentrations of insulin andelevated concentrations of glucagon in the portal vein, glucagon’s actions areexcessive, contributing to an endogenous and unnecessary supply of glucose inthe fed state. To date, no pharmacological means of regulating glucagon existand the need to decrease postprandial glucagon secretion remains a clinicaltarget for future therapies.
Also Check: Diabetic Give Blood
Hormones Of The Pancreas
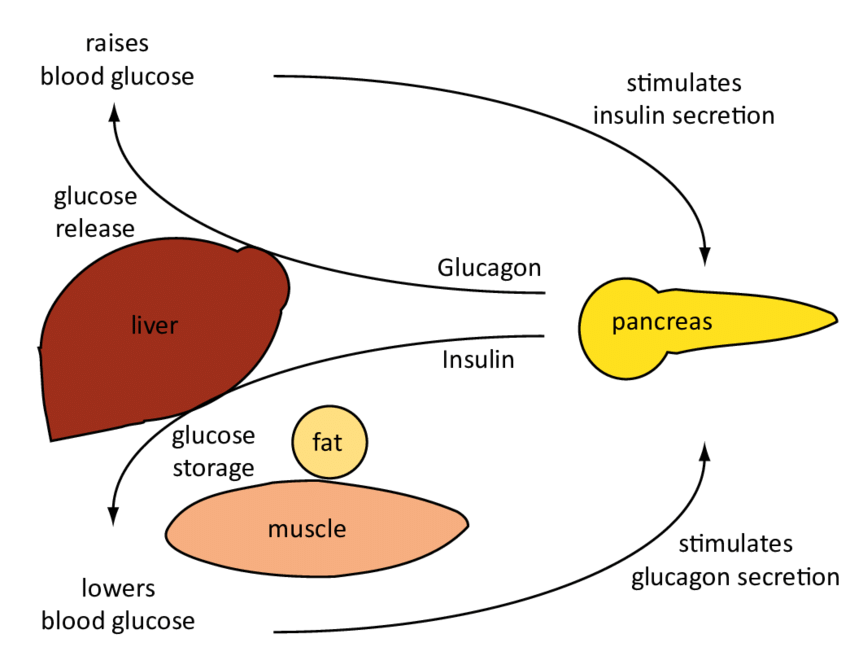
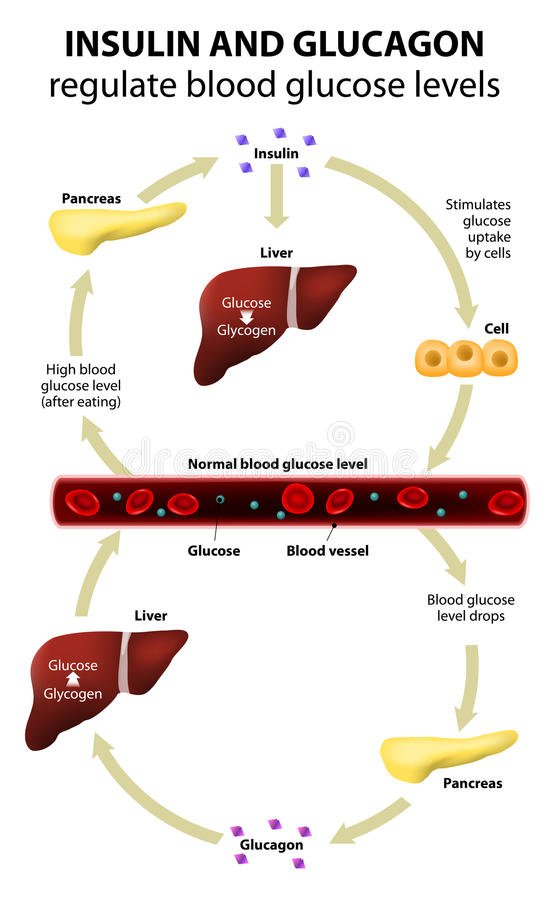
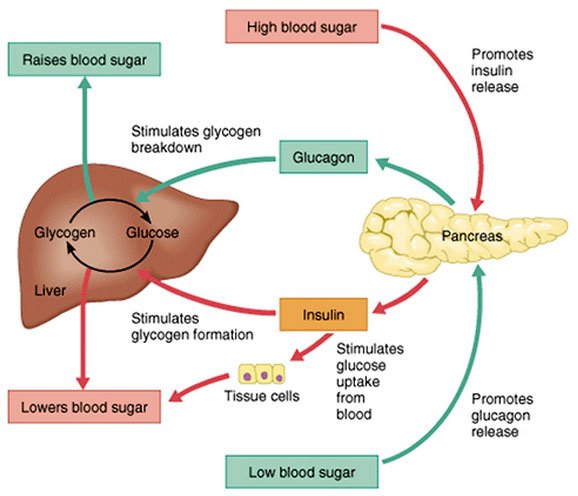
Regulation of blood glucose is largely done through the endocrine hormones of the pancreas, a beautiful balance of hormones achieved through a negative feedback loop. The main hormones of the pancreas that affect blood glucose include insulin, glucagon, somatostatin, and amylin.
Insulin lowers BG levels, whereas glucagon elevates BG levels.
Somatostatin is formed in the delta cells of the pancreas and acts as the pancreatic policeman, balancing insulin and glucagon. It helps the pancreas alternate in turning on or turning off each opposing hormone.
Amylin is a hormone, made in a 1:100 ratio with insulin, that helps increase satiety, or satisfaction and state of fullness from a meal, to prevent overeating. It also helps slow the stomach contents from emptying too quickly, to avoid a quick spike in BG levels.
In a healthy liver, up to 10% of its total volume is used for glycogen stores. Skeletal muscle cells store about 1% of glycogen. The liver converts glycogen back to glucose when it is needed for energy and regulates the amount of glucose circulating between meals. Your liver is amazing in that it knows how much to store and keep, or break down and release, to maintain ideal plasma glucose levels. Imitation of this process is the goal of insulin therapy when glucose levels are managed externally. Basalbolus dosing is used as clinicians attempt to replicate this normal cycle.
Test Your Knowledge
Apply Your Knowledge
Online Resource
Mode Of Action And Effect On Metabolism
The effects of insulin are mediated by binding to its specific tyrosine kinase transmembrane receptor. The insulin receptor is a tetrameric protein with two extracellular -subunits and two intracellular -subunits. IR is present in both peripheral and central tissues. In peripheral tissues, insulin mediates metabolism via downstream activation of phosphatodylinostiol 3 kinase and insulin receptor substrate . The IRS-P13K pathway results in activation of different kinases. Recent evidence suggests that insulins action on hepatocytes stimulates glycolysis and lipogenesis via the protein complex mTORC2. Insulin is also considered to reduce gluconeogenesis by downregulating the Forkhead box class O transcription factors. Further effects on metabolism also include glycogen and protein synthesis.
Don’t Miss: What Is A Normal A1c For A Non Diabetic
How Does Insulin And Glucagon Regulate Glycolysis
insulinwillcanGlucagon doeswill
Insulin helps the cells absorb glucose, reducing blood sugar and providing the cells with glucose for energy. When blood sugar levels are too low, the pancreas releases glucagon. Glucagon instructs the liver to release stored glucose, which causes blood sugar to rise.
Additionally, does insulin increase glycolysis? Insulin has the opposite effect on these enzymes. Thus the phosphorylation of phosphofructokinase inhibits glycolysis, whereas its dephosphorylation through the action of insulin stimulates glycolysis.
Similarly, you may ask, how does insulin regulate glycolysis?
Glycolysis is regulated by a key bifunctional enzyme, 6-phosphofructo-2-kinase/fructose-2,6-bisphosphatase 1 . Insulin dephosphorylates phosphorylated-PFKFB1 and activates its kinase activity, thereby promoting glycolysis .
Why does glucagon inhibit glycolysis?
Glucagon generally elevates the concentration of glucose in the blood by promoting gluconeogenesis and glycogenolysis. Glucagon turns off glycolysis in the liver, causing glycolytic intermediates to be shuttled to gluconeogenesis. Glucagon also regulates the rate of glucose production through lipolysis.
Insulin And Tca Cycle
Ketones in insulin resistant state 1. How is glucose normally maintained in the post absorptive state? 2. Why is muscle glycogen not useful for bloodglucose 3. Why may this situation have evolved 4. Under what circumstances do you think substantial gluconeogenesis will occur 5. What is necessary for the production of ketones 6. What will reduce acetyl CoA oxidation 7. When is oxaloacetate availability impaired 8. When is the regulation of gluconeogenesis disrupted…
PremiumCitric acid cycle, Metabolism, Glucose 958 ;Words | 4 ;Pages
Recommended Reading: Does Diet Soda Raise Insulin Levels
Regulation Of Blood Glucose Levels By Insulin And Glucagon
Glucose is required for cellular respiration and is the preferred fuel for all body cells. The body derives glucose from the breakdown of the carbohydrate-containing foods and drinks we consume. Glucose not immediately taken up by cells for fuel can be stored by the liver and muscles as glycogen, or converted to triglycerides and stored in the adipose tissue. Hormones regulate both the storage and the utilization of glucose as required. Receptors located in the pancreas sense blood glucose levels, and subsequently the pancreatic cells secrete glucagon or insulin to maintain normal levels.
How Is Glucagon Controlled
Glucagon works along with the hormone insulin to control blood sugar levels and keep them within set levels.;Glucagon is released to stop blood sugar levels dropping too low , while insulin is released to stop blood sugar levels rising too high .;
The release of glucagon is stimulated by low blood glucose, protein-rich meals and adrenaline . The release of glucagon is prevented by raised blood glucose and carbohydrate in meals, detected by cells in the pancreas.
In the longer-term, glucagon is crucial to the bodys response to lack of food.;For example, it encourages the use of stored fat for energy in order to preserve the limited supply of glucose.
Recommended Reading: Skinny Diabetics
Ideal Blood Sugar Levels
A range of factors, including insulin resistance, diabetes, and an unbalanced diet, can cause blood sugar levels to spike or plummet.
The standard measurement units for blood sugar levels are milligrams per deciliter . Ideal blood sugar ranges are as follows:
| Timing |
Insulin and glucagon do not take immediate effect, particularly in people whose blood sugar levels are extremely high or low.
What Happens If I Have Too Little Glucagon
Unusual cases of deficiency of glucagon secretion have been reported in babies.;This results in severely low blood glucose which cannot be controlled without administering glucagon.;
Glucagon can be given by injection to restore blood glucose lowered by insulin .;It can increase glucose release from glycogen stores more than insulin can suppress it. The effect of glucagon is limited, so it is very important to eat a carbohydrate meal once the person has recovered enough to eat safely.
You May Like: How Does High Blood Sugar Feel
Blood Sugar And Post Meal
Dependent Variable: plasma levels of glucose, ketones, insulin, and glucagon2.Independent Variable: food and beverage intake 3.Controlled Variables: physical activity, caffeine and alcohol intake, gender, age, BMI 4.Why were physical activity and caffeine and alcohol intake the controlled variables? You can control the amount of physical activity, caffeine and alcohol the patient intakes.5.What type of assay was used to measure plasma glucose and ketone levels? Glucose, Oxidase, Peroxide,…
PremiumCortisol, Diabetes mellitus, Blood sugar 775 ;Words | 6 ;Pages
Effects Of Autonomic Nerves
The islets of Langerhans receive both parasympathetic and sympathetic innervation. The activation of the parasympathetic system during meals stimulates insulin secretion at the same time that gastrointestinal function is stimulated. The activation of the sympathetic system, by contrast, stimulates glucagon secretion and inhibits insulin secretion. The effects of glucagon, together with those of epinephrine, produce a “stress hyperglycemia” when the sympathoadrenal system is activated.
Read Also: What Happens If A Diabetic Eats Too Much Sugar
Understanding The Processes Behind The Regulation Of Blood Glucose
20 April, 2004
VOL: 100, ISSUE: 16, PAGE NO: 56
Pat James, PhD, is senior lecturer in applied physiology
Roger McFadden, MSc, is senior lecturer in applied physiology; both at the School of Health and Policy Studies, The University of Central England in Birmingham
Pat James, PhD, is senior lecturer in applied physiology
Glucose is one of the bodys principal fuels. It is an energy-rich monosaccharide sugar that is broken down in our cells to produce adenosine triphosphate. ATP is a small packet of chemical energy that powers the millions of biochemical reactions that take place in the body every second.
We obtain glucose from the food that we eat, predominantly starch-rich foods such as potatoes, rice, bread, and pasta. Starch is a polysaccharide that is broken down by digestive enzymes into individual glucose molecules.
In the small intestine, glucose is absorbed into the blood and travels to the liver via the hepatic portal vein. The hepatocytes absorb much of the glucose and convert it into glycogen, an insoluble polymer of glucose.
This is stored in the liver and can be reconverted into glucose when blood-glucose levels fall. Other types of simple sugars in our diet such as fructose, sucrose and lactose are also fuels that contribute to the production of ATP.
If glucose levels fall to too low a concentration or rise too high then this situation can lead to the neurological processes in the brain being compromised.
Antagonistic Glucagon Peptide Analogs
Extensive efforts have been made to generate linear and cyclic peptide glucagon analogs. Compared with the wild-type glucagon, some of these peptide analogs have been shown to have distinct properties in terms of their ability to bind to the glucagon receptor and affect glucagon-stimulated cAMP production. They act as pure agonists, partial agonists/antagonists, or pure antagonists of the glucagon receptor . It was first reported that -glucagon, a potent antagonistic glucagon analog, significantly decreased hyperglycemia in streptozotocin-induced diabetic rats in vivo . -glucagon amide, another potent antagonistic glucagon analog, was also found to completely block exogenous glucagon-induced hyperglycemia in normal rabbits and to block hyperglycemia due to endogenous glucagon in streptozotocin-induced diabetic rats . Finally, similar glucose-lowering effects have been reported for another antagonistic glucagon analog, -glucagon-NH2 . It is therefore possible that such antagonistic peptide glucagon analogs may also have therapeutic potentials.
You May Like: Non Diabetic A1c Levels
Blood Glucose Concentration Lab Report
From the experiment, the bloodglucose concentration for Patient A is 5.6 mmol/L. The bloodglucoselevel for Patient A is normal as 5.6mmol/L is in the normal range. Urine sample from Patient A was tested and it is shown that there was no glucose and sodium present. The results showed that Patient A is healthy and could act as a control in this investigation. Secondly, patient B is suspected to suffer from diabetes mellitus. The bloodglucose concentration for Patient B is 111mmol/L…
PremiumEnzyme, Blood, Glucose 801 ;Words | 4 ;Pages
How Do Insulin And Glucagon Regulate Blood Glucose Levels
Insulin and glucagon work to help keep your blood glucose level under control. Both of these hormones are produced in the pancreas.;Insulin, which helps to normalize a high level of blood sugar, is produced by the beta cells. On the other hand, glucagon, which helps to control a low level of blood sugar, is produced by the alpha cells.
Read Also: Low Hba1c Symptoms
The Pancreas Is An Exocrine And Endocrine Organ
Anatomical organization of the pancreas. The exocrine function of the pancreas is mediated by acinar cells that secrete digestive enzymes into the upper small intestine via the pancreatic duct. Its endocrine function involves the secretion of various hormones from different cell types within the pancreatic islets of Langerhans. The micrograph shows the pancreatic islets. LM × 760 . Adapted from Human Anatomy and Physiology, an OpenStax College resource.
Maintenance of blood glucose levels by glucagon and insulin. When blood glucose levels are low, the pancreas secretes glucagon, which increases endogenous blood glucose levels through glycogenolysis. After a meal, when exogenous blood glucose levels are high, insulin is released to trigger glucose uptake into insulin-dependent muscle and adipose tissues as well as to promote glycogenesis.
Cells And Secretions Of The Pancreatic Islets
The pancreatic islets each contain four varieties of cells:
- The alpha cell produces the hormone glucagon and makes up approximately 20 percent of each islet. Glucagon plays an important role in blood glucose regulation; low blood glucose levels stimulate its release.
- The beta cell produces the hormone insulin and makes up approximately 75 percent of each islet. Elevated blood glucose levels stimulate the release of insulin.
- The delta cell accounts for four percent of the islet cells and secretes the peptide hormone somatostatin. Recall that somatostatin is also released by the hypothalamus , and the stomach and intestines also secrete it. An inhibiting hormone, pancreatic somatostatin inhibits the release of both glucagon and insulin.
- The PP cell accounts for about one percent of islet cells and secretes the pancreatic polypeptide hormone. It is thought to play a role in appetite, as well as in the regulation of pancreatic exocrine and endocrine secretions. Pancreatic polypeptide released following a meal may reduce further food consumption; however, it is also released in response to fasting.
Recommended Reading: Diabetes And The Digestive System
Got It Whats Glucagon
Glucagon is similar to insulin: Its another hormone your pancreas releases that controls the levels of glucose in your blood.
Glucagon works with your liver to prevent your blood sugar level from dropping too low. It also helps convert glycogen into glucose and releases it into your blood so your body can use it for energy.
Ever the multitasker, glucagon also works to keep your liver from consuming too much glucose in order to keep your blood sugar stable throughout your body.
Glucagon And Glucagon Receptor In Diabetes
There is ample evidence suggesting that glucagon plays an important role in initiating and maintaining hyperglycemic conditions in diabetic animals and humans. Insulin and glucagon are the key regulatory hormones for glucose homeostasis. The absolute levels and, even more so, the ratios of the two hormones are tightly regulated in vivo, depending on nutritional status. It has been reported that the absolute levels of glucagon or the ratios of glucagon to insulin are often elevated in various forms of diabetes in both animal and human subjects . Diabetes is also one of the diseases associated with glucagonoma, a glucagon-secreting tumor derived from pancreatic islet -cells . Chronic hyperglucagonemia is correlated with and is at least partially responsible for increased hepatic glucose output and hyperglycemia in type 2 diabetes .
It is controversial whether the number of glucagon receptors is altered in diabetic states. Most studies, however, appear to suggest that the number of glucagon receptors is reduced in diabetic subjects. Interestingly, even in the presence of fewer glucagon receptors, the ability of glucagon to stimulate cAMP production may remain unchanged or even be elevated . This may be at least partially explained by the observation that the activation of adenylate cyclase by glucagon involves only 20% of glucagon receptors .
Don’t Miss: How Long Do Type 1 Diabetics Live
Regulation Of Blood Glucose Levels By Thyroid Hormones
The basal metabolic rate, which is the amount of calories required by the body at rest, is determined by two hormones produced by the thyroid gland: thyroxine, also known as tetraiodothyronine or T4, and triiodothyronine, also known as T3. These hormones affect nearly every cell in the body except for the adult brain, uterus, testes, blood cells, and spleen. They are transported across the plasma membrane of target cells and bind to receptors on the mitochondria resulting in increased ATP production. In the nucleus, T3 and T4activate genes involved in energy production and glucose oxidation. This results in increased rates of metabolism and body heat production, which is known as the hormones calorigenic effect.
Disorders can arise from both the underproduction and overproduction of thyroid hormones. Hypothyroidism, underproduction of the thyroid hormones, can cause a low metabolic rate leading to weight gain, sensitivity to cold, and reduced mental activity, among other symptoms. In children, hypothyroidism can cause cretinism, which can lead to mental retardation and growth defects. Hyperthyroidism, the overproduction of thyroid hormones, can lead to an increased metabolic rate and its effects: weight loss, excess heat production, sweating, and an increased heart rate. Graves disease is one example of a hyperthyroid condition.

