Produced In The Pancreas
When you eat, food travels to your stomach and small intestines, where its broken down into nutrients that include glucose. The nutrients are absorbed and distributed via your bloodstream.
The pancreas is a gland located behind your stomach that performs an essential role in the digestion process. It creates enzymes that break down the fat, starches, and sugar in the food. It also secretes insulin and other hormones into your bloodstream.
Insulin is created in the beta cells of the pancreas. Beta cells comprise about 75% of pancreatic hormone cells.
Other hormones produced by the pancreas are:
- glucagon, which alerts your liver to raise your blood sugar if it gets too low
- gastrin, which stimulates the production of gastric acid in your stomach
- amylin, which helps control your appetite
I The Dual Nature Of The Pancreas
The pancreas is a complex gland active in digestion and metabolism through secretion of digestive enzymes from the exocrine portion and hormones from the endocrine portion. The exocrine pancreas, which accounts for more than 95-98% of the pancreas mass , is structurally comprised of lobules, with acinar cells surrounding a duct system. The endocrine pancreas makes up only 2% of the pancreatic mass and is organized into the islets of Langerhans small semi-spherical clusters of about 1500 cells dispersed throughout the pancreatic parenchyme which produce and secrete hormones critical for glucose homeostasis. The existence of islets was described by Paul Langerhans in 1869, and the functional role of islets in glucose homeostasis was first demonstrated in 1890 when Joseph von Mering and colleagues showed that dogs developed diabetes mellitus following pancreatectomy . Though islet mass may vary between individualsan example is the increase in the setting of adult obesity the average adult human pancreas is estimated to contain one to two million islets . In humans, the concentration of islets is up to two times higher in the tail compared to the head and neck. However, the cellular composition and architectural organization of cell types within the islets is preserved throughout the pancreas .
What Are The Sex Hormones
The sex hormones comprise of estrogen and testosterone. Estrogen is known as the female hormone and testosterone as the male hormone this is due to the fact that women normally produce more estrogen and men more testosterone. Nevertheless, both hormones play an important role in our bodies, regardless of our gender.As the name sex hormone suggests, these hormones are primarily responsible for sex drive and reproduction. If the hormone levels in our bodies decrease, then our libido also suffers at the same time.
Also Check: When Do Diabetics Need Insulin
Types Of Insulin Administration With Needles Pumps Pens And Why Insulin Is So Expensive
What does insulin do? Help your body turn food into energy, for starters. When youre diabetic, and youre either not producing insulin, or your insulin function is off, all sorts of things can go wrong. From needles, to pens, to pumps, to types of insulin, were here to empower you with clear answers to all your pressing Qs.
In This Article:
Alvin Powers MD, Mihail Zilbermint MD, and Irl Hirsch MD
Iii Insulin Gene Transcription
The insulin gene on chromosome 11 is primarily expressed in pancreatic b cells, but is expressed in low levels in the brain, thymus, and in the yolk sak during fetal development . It has three exons and two introns, and its transcription results in the 446 base pair preproinsulin mRNA .
Figure 1. Various levels of glucose regulation of insulin gene expression. Glucose stimulates nuclear translocation of Pdx-1 promotes Pdx-1 and MafA phosphorylation and binding to the insulin promoter and stimulates transcription of the insulin gene, pre-mRNA splicing, translation, and mRNA stability. ).
Transcription of the insulin gene to preproinsulin mRNA is sophisticated and reflects the tight regulation by transcription factors and recruited coactivators. Pdx-1, NeuroD1 and MafA are important transcription factors in b cell function, respond to elevated glucose levels. Individual b cells respond to ambient glucose with differential insulin secretion, and these changes are apparent at the level of gene transcription . At the level of the islet, rapid increase in blood glucose results in rapid elevation in preproinsulin mRNA in the endocrine pancreas. A rapid decrease in blood glucose results in a slow decline in preproinsulin mRNA.
This is due to the unusual stability of preproinsulin mRNA, further stabilized by increased glucose concentrations . The specific regulation of this molecules translation is the primary mechanism of insulin production control .
Also Check: How Many Points Does Metformin Lower Blood Sugar
Production Of Hormones To Control Blood Sugar Levels
A small proportion of the pancreas is made up of other types of cells called islets of Langerhans. These cells sit in tiny groups, like small islands, scattered throughout the tissue of the pancreas. The islets of Langerhans contain alpha cells which secrete glucagon and beta cells which secrete insulin.
Insulin and glucagon are hormones that work to regulate the level of sugar in the body to keep it within a healthy range. Unlike the acinar cells, the islets of Langerhans do not have ducts and secrete insulin and glucagon directly into the bloodstream.
Depending on what youve eaten, how much exercise your muscles are doing, and how active your body cells are, the amount of glucose in your bloodstream and cells varies. These 2 hormones have the job of keeping tight control of the amount of glucose in your blood so that it doesnt rise or fall outside of healthy limits.
Mechanisms Of Insulin Resistance
Physiologically, at the whole body level, the actions of insulin are influenced by the interplay of other hormones. Insulin, though the dominant hormone driving metabolic processes in the fed state, acts in concert with growth hormone and IGF-1 growth hormone is secreted in response to insulin, among other stimuli, preventing insulin-induced hypoglycaemia. Other counter-regulatory hormones include glucagon, glucocorticoids and catecholamines. These hormones drive metabolic processes in the fasting state. Glucagon promotes glycogenolysis, gluconeogenesis and ketogenesis. The ratio of insulin to glucagons determines the degree of phosphorylation or dephosphorylation of the relevant enzymes. Catecholamines promote lipolysis and glycogenolysis glucocorticoids promote muscle catabolism, gluconeogenesis and lipolysis. Excess secretion of these hormones may contribute to insulin resistance in particular settings, but does not account for the vast majority of insulin resistant states.
Recommended Reading: How Many Carbs Should A Diabetic Eat In One Day
The Insulin Resistance Syndrome
The insulin resistance syndrome describes the cluster of abnormalities which occur more frequently in insulin resistant individuals. These include glucose intolerance, dyslipidaemia, endothelial dysfunction and elevated procoagulant factors, haemodynamic changes, elevated inflammatory markers, abnormal uric acid metabolism, increased ovarian testosterone secretion and sleep-disordered breathing. Clinical syndromes associated with insulin resistance include type 2 diabetes, cardiovascular disease, essential hypertension, polycystic ovary syndrome, non-alcoholic fatty liver disease, certain forms of cancer and sleep apnoea.
What Are The Different Types Of Insulin
The American Diabetes Association characterizes insulin by how fast it works. But everyones body is different. If you have diabetes, you should expect deviations in the amount of time any medication takes to reach your bloodstream.
Here are 8 different types of Insulin and how they work.
- Onset is defined as the length of time before insulin hits your bloodstream and begins to lower blood glucose.
- Peak is the time during which insulin is at its maximum effectiveness at lowering your blood glucose levels.
- Duration is the length of time insulin continues to lower your blood glucose levels.
- Rapid-acting insulin begins to affect blood glucose approximately 15 minutes after injection. It peaks in about an hour, and then continues to work for a few more.
- Short-acting insulin reaches your bloodstream within 30 minutes of injection. It peaks in the 2-3-hour range and stays effective for 3-6 hours.
- Intermediate-acting insulin includes NPH insulin which helps control glucose for 10-12 hours. A protamine is a type of protein that slows the action of this insulin.
- Long-acting insulin enters the bloodstream 1-2 hours after injection and may be effective for as long as 24 hours. An advantage to long-acting insulin is there is no pronounced peak, and it works more like typical pancreatic insulin.
- Premixed/combination insulin contains a mix of rapid- or short-acting insulin combined with an intermediate-acting insulin. This eliminates the need to draw insulin from more than one bottle.
You May Like: Metformin Side Effects Blurred Vision
Avoiding Injection Bruises And Lumps
Bruising can happen when you catch a tiny capillary under the skin where you have injected. It is quite normal for this to happen occasionally when you are injecting regularly and youre not doing anything wrong.
If you are concerned, you could make an appointment with your diabetes specialist nurse who will be able to do a review of your injection technique. In some cases, bleeding and bruising can be reduced by something as simple as using a different sized needle or changing your needle after each injection.
Some people notice hard lumps that can form if you inject in the same place too often. This might be lipohypertrophy , or could be something called cutaneous amyloidosis. These lumps can stop the insulin from working properly, so make sure you rotate where you inject and choose a different spot each time. If you notice any lumps, especially if they’re not going away, speak to your healthcare professional for more advice.
Other side effects from injecting a lot can be itching, rashes and other skin irritations. Changing where you inject helps with this too. You can also get treatments from your local pharmacy that can will help with the irritation.
Insulin And Body Set Weight
Hormones are chemical messengers regulating almost everything. For example, they regulate hunger, satiety, thirst, body temperature, and body weight.
The region of the brain responsible for the regulation of those essential processes is called the hypothalamus.
With this in mind, a defining ability of the human body is the adaption to change called homeostasis.
Therefore the hypothalamus is tightly regulating body temperature around a stable level. Thats usually about 36°C or 98°F.
Similarly, the same principle of homeostasis applies to body weight. Hence, it isnt high caloric intake or lack of exercise that causes weight gain.
However, the food industry is trying to tell us so because the calorie approach justifies low-quality food.
Instead, a hormonal imbalance is setting body weight to an unhealthy level. Given that, the hypothalamus commands the body to increase fat mass using available calories.
As a result, the body is short of energy and craves for increased caloric intake.
Consequently, the hypothalamus increases the hunger hormone ghrelin and decreases the satiety hormones peptide YY, cholecystokinin, and leptin.
Restrictingcalories to counteract the bodys effort to increase fat mass doesnt work outlong-term. In that case, the basal metabolism is down-regulated to satisfy thehigher priority goal of gaining body fat.
For thisreason, overeating and lack of physical activity are symptoms of obesity ratherthan its causes.
Recommended Reading: How Many Points Does Metformin Lower Blood Sugar
Why Are Hormones Called Chemical Messengers
The prominent role of hormones is that of a messenger. Hypothalamus is a part of forebrain where a numerous amount of neurosecretory cells are present. These neurosecretory cells are specialized in the secretion of a hormone called neurohormones. They stimulate the anterior lobe of the pituitary to produce various other hormones.
Sometimes, hormones act more than a regulator than a messenger. The changes in the level of hormone production lead to certain changes in the body. Thus, hormone as a regulator maintains the homeostasis of the body. Once the hormones meet their target, their production needs to be controlled and this is attained by a mechanism called feedback control mechanism. The feedback mechanism could either be positive or negative.
The Battle Of The Hormones: Estrogen Vs Insulin
One of the most frequently asked questions by women as they get older is: Why is it so hard to lose weight if Im eating right and exercising? You may be doing the same exact things youve always done, but suddenly find its just not enough. What you might not realize is that hormonal fluctuations could be playing a part in your weight gain. Many womens first thought is: can estrogen cause weight gain? Well, estrogen dominance canits when you have a disproportionate amount of estrogen in relation to your progesterone.
There are also other hormones that need to be balanced at any age in order to maintain a healthy weight. You already read about cortisol and leptin in our two previous articles and how they affect weight gain after 40. Read on to discover how estrogen and insulin affect your weight and how to balance them naturally to lose weight and feel great.
You May Like: Can You Be Skinny And Have Diabetes
Why Does Insulin Cause Weight Gain
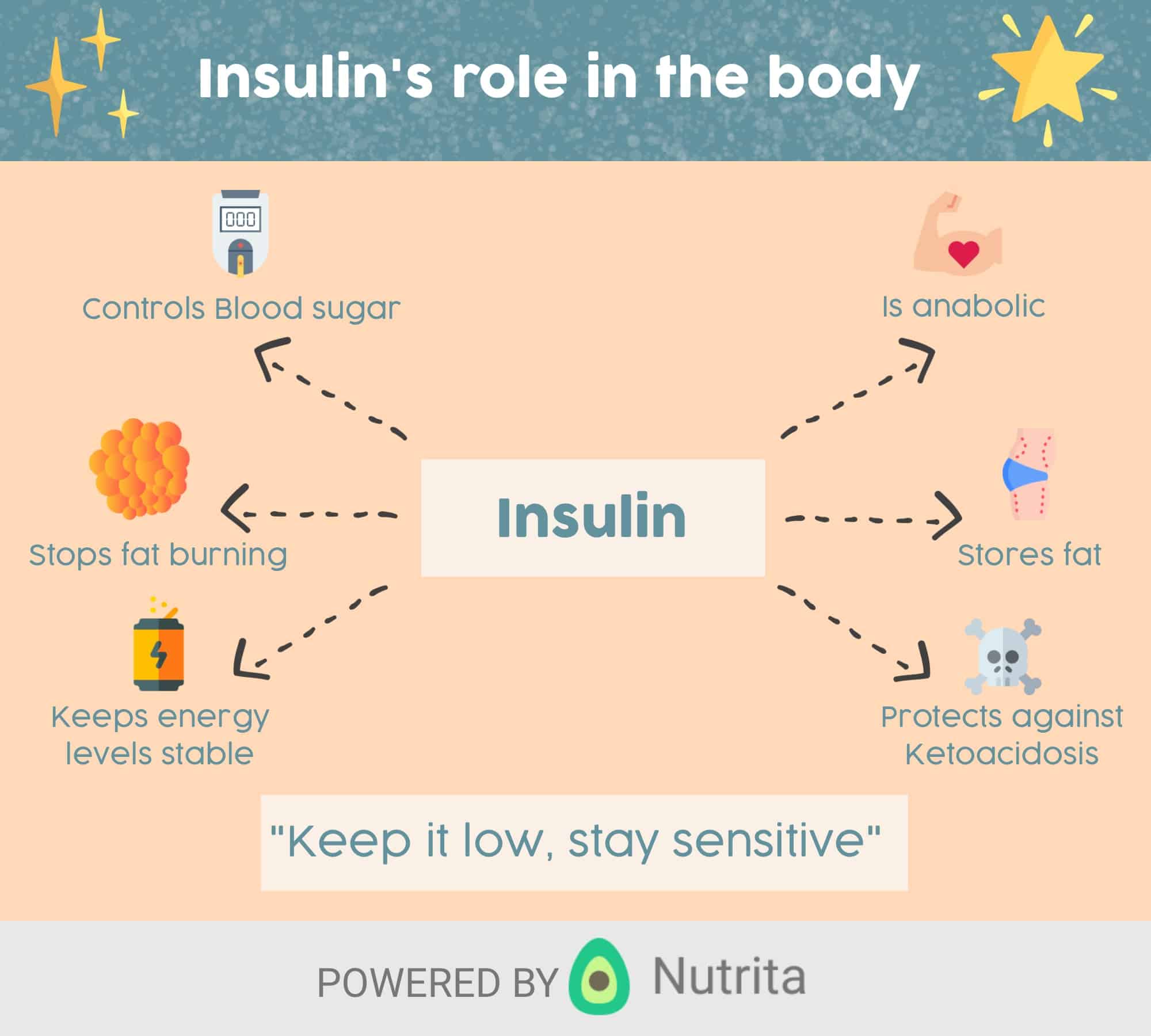
Insulin is the primary storage hormone. Hence, any food consumption leads to insulin release.
It then acts as a messenger for sugar and fat storage. Contrarily, in the absence of food, the high levels of insulin drop to enable the burning of sugar and later fat for energy.
Asexplained above, the average person is seldom tapping into body fat for energy.But that only explains why insulin isnt good for weight loss.
In the case of glycogen stores in the liver are full, it generates new fat.
Therefore your excess carbohydrates will be stored as newly synthesized fat around organs , below your skin , or directly in the liver .
Nature built us for periods of feeding and fasting. The human body is meant to switch between the use of readily available and long-term stored energy.
Likewise, you might have heard that we are only losing weight during a nights sleep.
But over the last decades, we have completely repressed that we can go more than eight hours without eating persistently. Ad campaigns educated us with garbage, like having six meals a day to lose weight.
The results are excessively high levels of insulin, induced by the imbalance between feeding and fasting. As a crucial regulator of body weight, insulin causes weight gain.
In essence, we have a perfect recipe for an obesity epidemic .
Sites Of Insulin Action And Manifestations Of Insulin Resistance
The effects of insulin, insulin deficiency and insulin resistance vary according to the physiological function of the tissues and organs concerned, and their dependence on insulin for metabolic processes. Those tissues defined as insulin dependent, based on intracellular glucose transport, are principally adipose tissue and muscle. However, insulins actions are pleotropic and widespread, as are the manifestations of insulin resistance and the associated compensatory hyperinsulinaemia.
Don’t Miss: Which Pancreatic Cells Release Insulin And Glucagon
Types Of Insulin Treatments
All types of insulin produce the same effect. They mimic the natural increases and decreases of insulin levels in the body during the day. The makeup of different types of insulin affects how fast and for how long they work.
- Rapid-acting insulin: This type of insulin begins working approximately 15 minutes after injection. Its effects can last between three and four hours. Its often used before a meal.
- Short-acting insulin: You inject this insulin before a meal. It starts working 30 to 60 minutes after you inject it and lasts five to eight hours.
- Intermediate-acting insulin: This type of insulin starts working in one to two hours after injection, and its effects may last 14 to 16 hours.
- Long-acting insulin: This insulin may not start working until about two hours after you inject it. Its effects can last up to 24 hours or longer.
Insulin And Circulatory System
Our circulatory system makes sure that everything in the body goes well. When there isnt enough insulin in the blood then glucose gets back into the bloodstream from the storage cells. This increases the glucose level in the body which could cause diabetes and nervous disorders if the level exceeds the normal range.
On the other hand, if there is insulin in the blood then it maintains our glucose level and everything performs well.
In this way, our circulatory system ensures the proper amount of insulin when needed.
Recommended Reading: Can Skinny People Get Diabetes
Insulin As Treatment For Diabetes
Injections of insulin can help treat both types of diabetes. The injected insulin acts as a replacement for or supplement to your bodys insulin. People with type 1 diabetes cant make insulin, so they must inject insulin to control their blood glucose levels.
Many people with type 2 diabetes can manage their blood glucose levels with lifestyle changes and oral medication. However, if these treatments dont help to control glucose levels, people with the condition may also need insulin to help control their blood glucose levels.
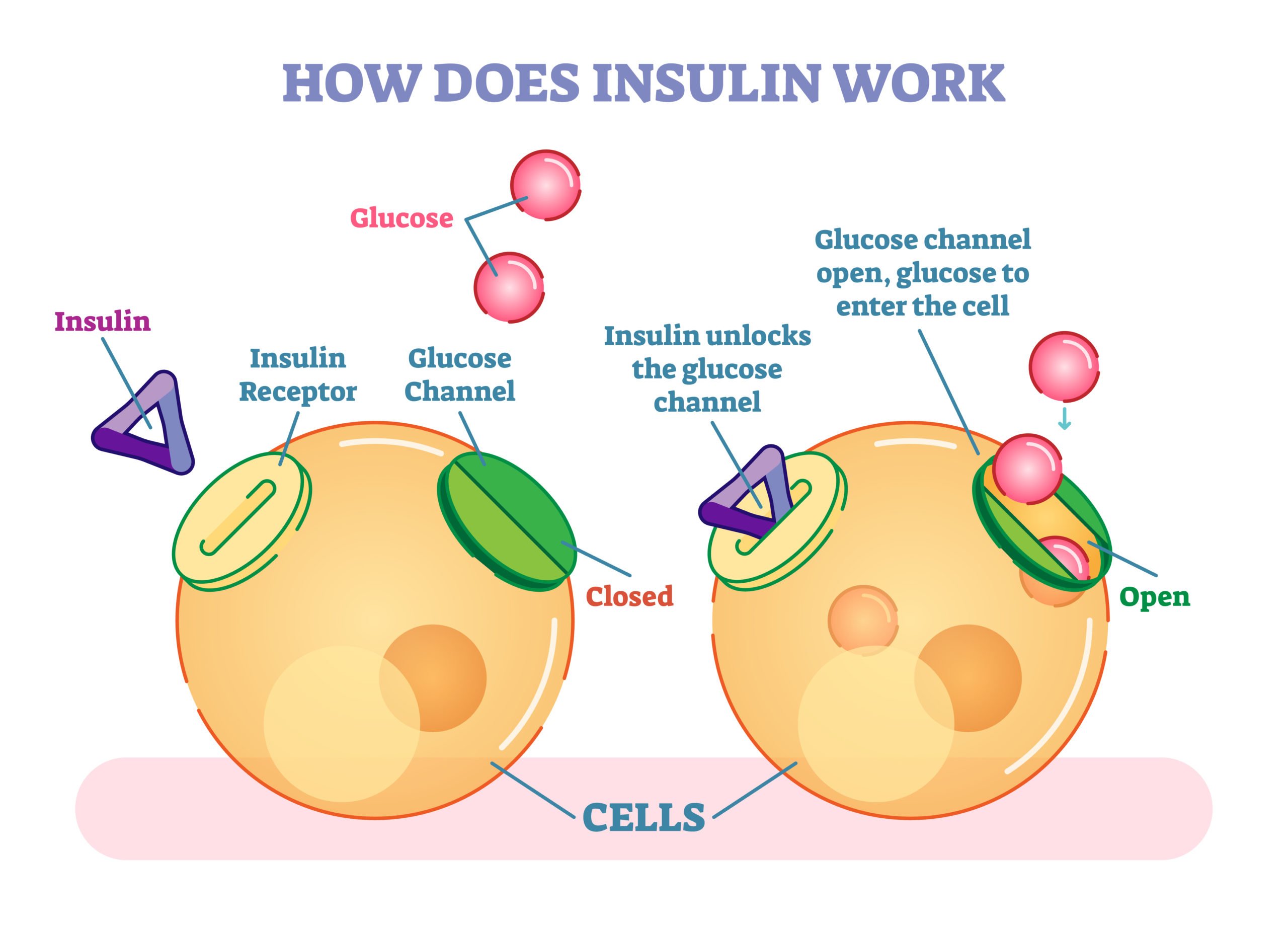
Insulin Receptors And Insulin Binding
Insulin mediates its actions through binding to insulin receptors. The insulin receptor was first characterised in 1971. It consists of a heterotetramer consisting of 2 and 2 glycoprotein subunits linked by disulphide bonds and is located on the cell membrane. The gene coding for the insulin receptor is located on the short arm of chromosome 19. Insulin binds to the extracellular subunit, resulting in conformational change enabling ATP to bind to the intracellular component of the subunit. ATP binding in turn triggers phosphorylation of the subunit conferring tyrosine kinase activity. This enables tyrosine phosphorylation of intracellular substrate proteins known as insulin responsive substrates . The IRS can then bind other signalling molecules which mediate further cellular actions of insulin.
PI 3-kinase promotes the translocation of glucose transporter proteins, glycogen, lipid and protein synthesis, anti-lipolysis and the control of hepatic gluconeogenesis. PI 3-kinase acts via serine and threonine kinases such as Akt/protein kinase B , protein kinase C and PI dependent protein kinases1& 2 . The RAS pathway activates transcription factors and stimulates the growth promoting actions of insulin. Thus broadly, PI 3-kinase mediates insulins metabolic effects, e.g. cellular glucose uptake, while RAS significantly mediates insulins mitogenic effects, together with other less well described actions. These pathways are presented schematically in .
Don’t Miss: What Happens If You Stop Taking Diabetes Medication

