Diabetes Can Cause Neuropathy
Diabetes can cause nerve damage called neuropathy, a common diabetes complication. Sometimes the damage causes a loss of sensation in the feet. If you step on something and injure your foot or develop a blister, you may not be able to feel it. An open skin sore called a foot ulcer can develop and could get infected. Take a look at your feet every day to make sure they are not injured in any way.
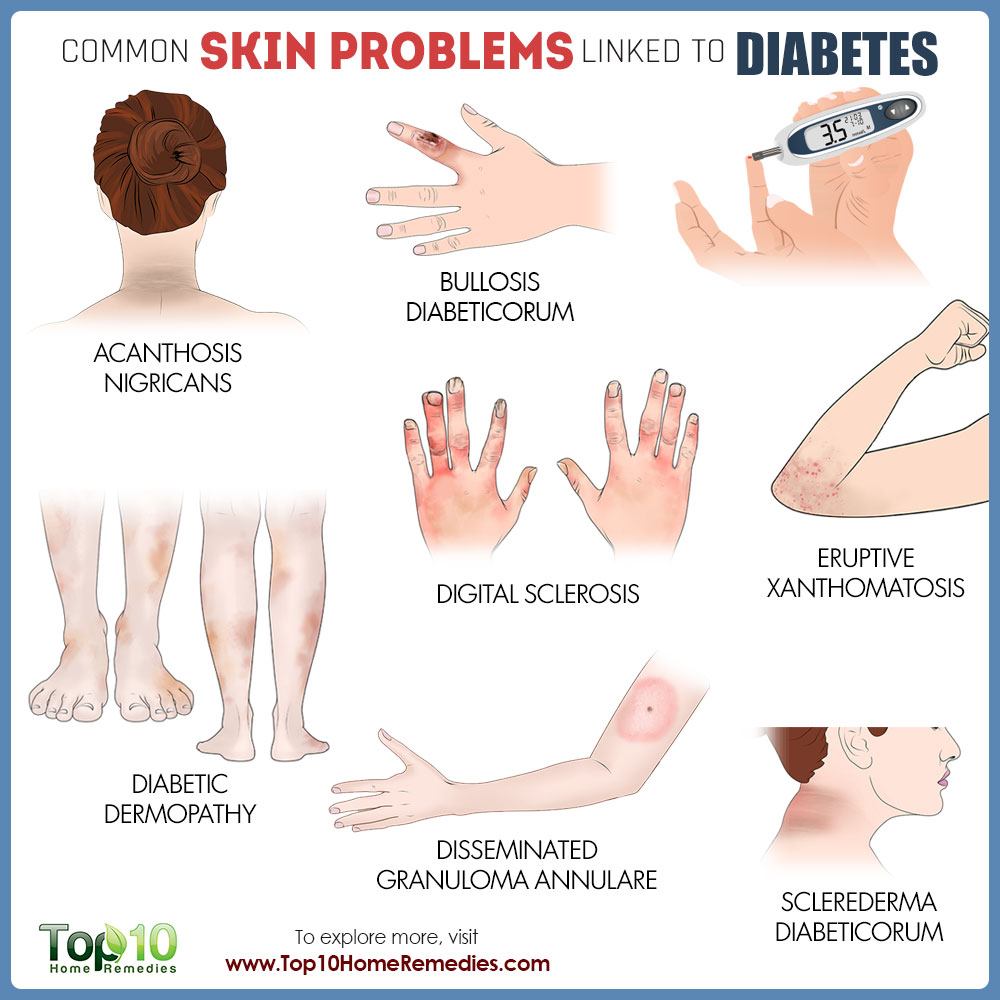
Good Blood Sugar Control Treats Digital Sclerosis
About a third of people with type 1 diabetes have digital sclerosis thick, tight, waxy skin that develops on the backs of the hands. The finger joints stiffen and become difficult to move. Sometimes this skin problem occurs on the toes and forehead as well. Rarely, knees, ankles, or elbows may stiffen. Again, good blood glucose control is the only treatment. Moisturizer may help soften the skin.
How To Manage Diabetes Skin Problems
For patients suffering from diabetic skin conditions, keeping their diabetes under control is the most important factor in preventing the development and worsening of skin-related diabetes complications. Maintaining control over blood glucose levels, using proper diabetic skin care, and staying hydrated by drinking plenty of water can help reduce the risk of skin-related problems. The following comprises additional ways to help prevent the occurrence and worsening of diabetes-related skin issues.
Discover How Advanced Dermatology & Skin Cancer Center Can Help Give You The Healthy Skin You Deserve
Read Also: Side Effects Of Metformin 500
Allergic Reactions To Medications
Nearly any diabetes medicationincluding insulincan trigger an allergic reaction that brings on symptoms that affect the skin, such as itching, swelling, rash, or redness.
Why it happens: Allergic reactions to medications occur because a person has a pre-existing sensitivity to either the drug itself or to an inactive ingredient in the drug, such as a preservative. Some people who use injectable medications experience skin reactions that are limited to the area where the needle was inserted.
What to do: Call your healthcare provider if you have an allergic reaction to a diabetes medication. He or she may instruct you to take an over-the-counter medication to relieve itching in the short term, and then will discuss trying a different drug to treat your diabetes.
If skin changes brought on by medication are accompanied by difficulty breathing or other alarming symptoms, get emergency help immediately.
Are You Suffering From A Diabetes
Do you have diabetes? Diabetes is the fastest growing long-term disease, affecting millions of people across the globe. In the United States, more than 25 million people suffer with diabetes. About 75 percent of them have type 2 diabetes, linked to obesity or being overweight. Researchers believe that the diabetes epidemic will escalate, and predict that in 2050, one in three Americans will have diabetes.
About a third of people with diabetes will develop skin problems such as skin sores or a leg rash. In fact, according to the American Diabetes Association , some skin problems can be warning signs of diabetes in those who are undiagnosed. The good news is that most skin problems with diabetes can be prevented or treated easily if theyre caught early.
Keeping proper control of your blood sugar can prevent diabetes skin problems and many other diabetes symptoms from happening in the first place.
Many diabetes skin problems can happen to healthy people, but people with diabetes have a much higher risk. Diabetes skin problems include:
- Bacterial infections
- Necrobiosis lipoidica diabeticorum
- Skin itching
Controlling your blood glucose is the first step in preventing and treating diabetes skin problems. When diabetes affects your skin, causing skin sores or diabetes rash, it is a sign your blood sugar levels are too high.
Also Check: Maximum Metformin Dose
Skin Discoloration And Changes In Texture
Diabetic dermopathy: Also known as shin spots, these diabetes skin symptoms involve light brown, oval or circular patches of scaly skin on the lower legs due to damage to the small blood vessels that supply the tissues with nutrition and oxygen. Although this form of diabetes-related skin discoloration typically does not require treatment, it may persist even when your blood glucose is well-controlled.1
Necrobiosis lipoidica diabeticorum : Though rarer than diabetic dermopathy, NLD also causes patches of dark skin on the legs, which are sometimes associated with extreme itching and pain. Though treatment is generally unnecessary, it is important to talk to your doctor about ways to prevent this condition from progressing.1
Acanthosis nigricans: This type of diabetes-related skin discoloration can present as raised patches of brown, tan or gray skin on the neck can, and can also appear in the groin and armpits as well as on the elbows and knees. The patches often have a velvety feel and appearance. This type of skin discoloration is more prevalent in diabetic patients who are obese.1
Ichthyosiform Changes Of The Shins
Ichthyosiform changes of the shins presents with large bilateral areas of dryness and scaling . Although cutaneous changes may occur on the hands or feet, the anterior shin is most classically involved. These cutaneous changes are related to rapid skin aging and adhesion defects in the stratum corneum . The prevalence of ichthyosiform changes of the shins in those with type 1 diabetes has been reported to be between 22% to 48% . These changes present relatively early in the disease course of diabetes. There is no known difference in prevalence between males and females . The development of ichthyosiform changes of the shins is related to production of advanced glycosylation end products and microangiopathic changes. Treatment is limited but topical emollients or keratolytic agents may be beneficial .
Also Check: Diabetic Slim Fast
Tight Blood Sugar Control Crucial
Both Garoufalis and Meffert agree the best way to avoid skin problems of all kinds is to maintain tight control of your blood sugar. This lessens the dryness and the chances of an opening for bacteria to enter your body. Good control helps preserve immune function, so you can better fight off an infection before it spreads. Lower average blood sugars also lessen the nerve and vessel damage that leads to ulcers and skin breakdown.
Control of diabetes has an effect on skin quality, quality of circulation, your perception of pain and other sensations and your ability to fight off infection, said Garoufalis. Having normal blood sugars is a key to long survival.
Skin Hydration: Avoiding The Progression
Dermocosmetic management through skin hydration and control of xerosis and callus symptoms are essential to avoid progression of skin lesions on DM patients . Regarding dermocosmetic approach, the most commonly used active ingredient is urea. In 2003, Schölermann et al. published the results of two studies with 10 % urea cream in dry skin treatment. In the first study, 603 patients with dry or extremely dry skin, of which 179 were DM patients, were treated with 10 % urea cream for 14 days, presenting a decrease on dryness, callosities and scaling compared to baseline. In the second study, 30 patients with diabetes and/or xerosis were treated in one foot with 10 % urea cream for 10 days, resulting in decreased callosities, dryness and scaling .
Federici et al. conducted a randomized controlled clinical trial with 40 type 2 DM patients who were allocated to receive urea 5 %, arginine and carnosine versus a glycerol-based emollient for 28 days. Patients treated with urea 5 %, arginine and carnosine presented an 89 % reduction on dryness according to DASI scale when compared to control emollient . Another study conducted with 54 type 1 and 2 DM patients treated with 10 % glycerin, 5 % urea, 1 % lactic acid and 8 % paraffin in an emulsion base versus placebo for 4 weeks also demonstrated a decrease of dryness and fissures and increased skin hydration on active-treated group .
Read Also: Rye Bread Good For Diabetes
Poor Blood Flow Results In Itchy Skin
Itchy skin can have many causes. In people with diabetes, a yeast infection, dry skin, or poor circulation can be the root cause. When poor blood flow is the culprit, the lower legs may be the itchiest part of the body. What can you do to stop your skin from crawling? Consider bathing less often, and use mild soap when you do. Slather on some lotion to moisturize dry skin, but avoid applying it between your toes.
Is Diabetes Causing Your Skin Problems
Diabetes can affect every part of the human body, including the skin. Experts say that at least one-third of diabetic patients, in their lifetime, will have to deal with some kind of skin infection or the other. Such skin problems are sometimes the first sign that an individual has diabetes. Most of these skin conditions can be prevented or treated if diagnosed early.
Some of these skin problems are conditions anyone can have, but people suffering from diabetes may acquire these more easily. Other skin problems happen to people with diabetes. These include necrobiosis lipoidica diabeticorum, diabetic dermopathy, and diabetic blisters.
Read Also: Is Pita Bread Bad For Diabetics
How Can I Prevent Skin Sores
- Keep your blood sugar within target range. Your diabetes care team provider will tell you what your blood sugar levels should be. High blood sugar levels increase your risk for skin infections and poor wound healing.
- Keep your skin clean. Do not take hot baths or showers. They can cause your skin to get dry. Do not take a bubble bath if you have dry skin. Use moisturizing soaps.
- Keep your skin from becoming too dry. Apply moisturizing lotion after baths or showers, especially in cold, dry weather. When you scratch dry, itchy skin, you can cause your skin to be open to infection. Bathe less during cold weather and use lotion to moisturize. Do not put lotion between your toes. Moisture between your toes could lead to skin breakdown. Use a humidifier to keep air in your home from being dry.
- Keep areas where skin touches skin dry. Use talcum powder in areas such as armpits and groin. You may also need it under your breasts, and between your toes. Moisture in these areas can cause a fungal infection.
- Treat cuts immediately. Clean minor cuts with soap and water. Cover them with sterile gauze.
Long Term Effects Of Diabetes On The Body
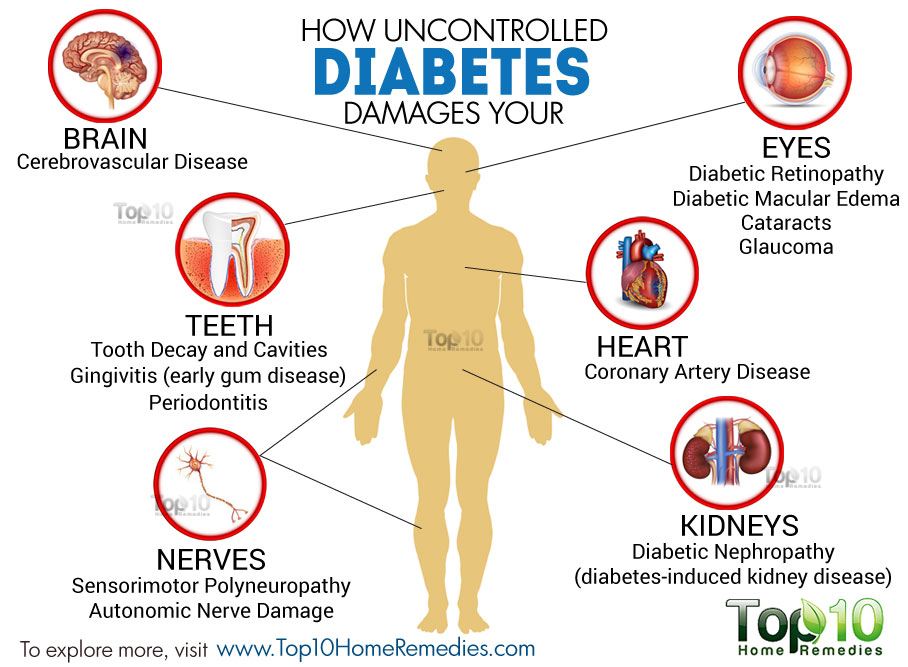
In addition to the symptoms, diabetes can cause long term damage to our body. The long term damage is commonly referred to as diabetic complications
Diabetes affects our blood vessels and nerves and therefore can affect any part of the body.
However, certain parts of our body are affected more than other parts.
Diabetic complications will usually take a number of years of poorly controlled diabetes to develop. Complications are not a certainty and can be kept at bay and prevented by maintaining a strong level of control on your diabetes, your blood pressure and cholesterol
These can all be helped by keeping to a healthy diet, avoiding cigarettes and alcohol, and incorporating regular activity into your daily regime in order to keep blood sugar levels within recommended blood glucose level guidelines
Recommended Reading: Adverse Effects Of Metformin
Shin Spots Or Diabetic Dermopathy
This condition involves circular, reddish, or light-brown patches that usually appear on the shins or other bony parts of the body. Patches are also usually indented and scaly.
Around 33 percent of people with type 1 diabetes and 39 percent of those with type 2 diabetes develop diabetic dermopathy.
The condition is caused by nerve and blood vessel damage, in particular small blood vessel changes.
As the condition impacts areas of the body with less protective muscle and fat, lesions may reflect an increased response to injury.
Lesions are harmless, and the person does not usually need treatment.
Sometimes, insignificant wounds can become open sores called diabetic ulcers. These can occur anywhere on the skin but are most common on the feet.
Diabetes can affect blood circulation and the nervous system. If a person has a wound on their foot due, for example, to ill-fitting shoes, the lack of sensation in the foot can mean that they do not notice the injury. In addition, low blood supply can make it harder for wounds to heal.
Without treatment, an ulcer can develop. If this becomes infected, there is a risk of tissue death, and the person may ultimately need an amputation.
It is essential for people with diabetes to:
- manage their blood sugar levels
- check their feet and other parts of the body regularly for wounds or lesions that may need attention
According to an article in
Why Are Diabetics More Prone To Skin Problems
People with diabetes may experience greater loss of fluid from the body due to high blood glucose levels, which can cause dry skin on the legs, elbows, feet and other areas of the body.
If dry skin becomes cracked, germs can get into these areas and cause infection, meaning that taking care of the skin is essential.
If not checked regularly, even minor skin care problems can evolve into serious diabetes complications, such as diabetic foot ulcers and even amputation
Keeping the skin, particularly of your feet, in good condition should be a priority for people with diabetes.
You May Like: How Does It Feel When Your Blood Sugar Is High
Toenails And Excess Skin
For the most part, it is safe for you to do much of your own general work on your feet and hands. If your nails are normal, cutting them straight across should pose no problem. However, if you have an ingrown toenail, it is best to see a podiatrist. The same suggestions hold if you have a fungal infection of the toenail.
The same guidelines are in place for removing excess skin. Careful use of a pumice stone or emery board should pose no problems if your diabetes is in good control and you arent having any nerve concerns.
In most cases, there is no need to use an antibiotic moisturizer. They usually are not only more expensive, but also harsher and destroy the normal flora on your skin that helps protect it.
Skin Conditions That Can Be A Sign Of Diabetes
Medically reviewed by Dr. Kenneth Knowles, MD on September 29th, 2020
If youre among the 30 million Americans with diabetes, youre probably no stranger to the skin conditions which often accompany this disease. If youre among the rest of the U.S. population, keep in mind that certain skin issues can often be a sign of diabetes, so its a good idea to stay on the lookout when it comes to your skin. Read on to learn about the top five skin conditions associated with diabetes, and what to do if you think you might have one.
Don’t Miss: Pita Bread And Diabetes
What Other Skin Conditions Affect People With Diabetes
People with diabetes can have any skin condition. But sometimes, people with diabetes have a rash or other skin irritation due to:
- Allergic reactions: People with diabetes may have an allergic reaction to oral diabetes medications or injectable insulin. You may develop a rash or hives and swelling at the injection site or elsewhere on your body. Contact your healthcare provider if you think youre having an allergic reaction.
- Bacterial infections: Having diabetes increases the risk of bacterial skin infections. You may develop bacterial infections in eyelid glands or deep under the skin . Infected skin may be swollen, hot, red and painful. Youll need antibiotics to get rid of the infection.
- Dry, itchy skin: High blood sugar and certain skin conditions can cause dry, itchy skin. If you have poor blood circulation, your lower legs may itch the most. Moisturizers can help.
- Fungal infections: A yeast called Candida albicans causes most fungal infections in people with diabetes. Youll have moist areas of tiny red blisters or scales that itch. Skin fungus tends to affect skin folds, including under the breast, between fingers and toes, around nailbeds, and in the armpits and groin. Common fungal infections include jock itch, athletes foot and ringworm. Antifungal medications can help.
Dry Skin And Infections
Dry skin can lead to many major concerns in diabetes. Cracking and peeling results in openings in the skin, allowing bacteria or fungi to enter the body. High levels of sugar in the body are great breeding grounds and reduce your bodys ability to heal itself, increasing the chances an infection may spread.Several different kinds of bacterial infections occur more often in people with diabetes. Among these are:
styes in the glands of the eyelids boils folliculitis of the hair follicles carbuncles very deep infections of the skin and underlying tissue and infections around the nails.
With bacterial infections, you most often first see a redness around the area of the cut or crack, said Matthew G. Garoufalis, DPM, a podiatrist in private practice in Chicago. People with diabetes are at a disadvantage because they often will not feel pain, which can be an early warning that an infection is occurring. As it progresses, you may also see drainage from the wound, and it may become warm to the touch.
Fungal infections also are a concern. Most often, the organism in skin folds is Candida albicans. This is a yeast-like fungus that creates a rash of moist, red areas surrounded by tiny blisters. They occur most often in warm and moist areas. Other common fungal diseases include jock itch, athletes foot, ringworm, and vaginal infections.
Read Also: Fasting Blood Sugar For Type 2 Diabetes
Dryness Starts A Harmful Cycle
makes people more prone to dry and itchy skin or infections. decreases the amount of fluid your body holds, leaving your skin parched and prickly. Nerve damage can also stifle your sweat response. As a result, your skin loses natural softness and moisture.
You may notice dry skin first on your legs, feet, and elbows, but it can occur anywhere on your body. Scratching can produce cracks, creating a way for bacteria and other germs to enter. Bacteria and fungi can also invade the glands of your eyelids, your hair follicles, the area around your nails, the spaces between your fingers and toes, and your armpits or groin, among other sites.
Harmful infections receive sustenance from blood sugar. Diabetics have generally weaker immune systems, making them less able to fight infections. Also, nerve damage and poor circulation slow tissue healing. As a result, people with diabetes often have more frequent and serious wounds and skin infections than people without the condition.
Infected tissues often burn, appear red or swollen, itch, or form blisters or scales. Talk with your doctor if you spot any of these signs. You may need prescription medicines such as the antifungal drug Diflucan to control an infection.

