If You Take Too Little Insulin
Taking too little insulin can cause your blood glucose level to rise too high. This is called hyperglycaemia.
If you have forgotten or missed a dose of insulin, or not taken enough insulin:
- Do not take the missed dose or extra insulin unless your diabetes nurse or educator or doctor advises you to do so.
- Drink plenty of sugar-free, non-alcoholic fluids such as water to stay well hydrated. Avoid alcohol and drinks containing caffeine, such as cola, tea and coffee because these can dehydrate you.
- Continue to monitor your blood glucose level regularly.
- If you find your blood glucose level remains high, you will need to address this see hyperglycaemia.
Physiology Of Insulin Secretion
Glucose is the principal stimulus for insulin secretion, though other macronutrients, hormones, humoral factors and neural input may modify this response. Insulin, together with its principal counter-regulatory hormone glucagon, regulates blood glucose concentrations. Pancreatic cells secrete 0.251.5 units of insulin per hour during the fasting state, sufficient to enable glucose insulin-dependent entry into cells. This level prevents uncontrolled hydrolysis of triglycerides and limits gluconeogenesis, thereby maintaining normal fasting blood glucose levels. Basal insulin secretion accounts for over 50% of total 24 hour insulin secretion. Following secretion of insulin into the portal venous system, 60% is subsequently removed by the liver so portal vein insulin concentrations reaching the liver approach triple that of the peripheral circulation. In healthy lean individuals circulating venous fasting insulin concentrations are about 315 mIU/L or 1890 pmol/L. Meal-related insulin secretion accounts for the remaining fraction of the total daily output.
How Insulin Functions On A Cellular Level
The primary functions of insulin in the body’s cells have to do with the metabolism of carbohydrates, fats, and amino acids from protein as well as the transcription and translation of mRNA.
- Carbohydrates: Insulin contributes to carbohydrate metabolism at many points during the process. It facilitates the diffusion of glucose from carbohydrates into fat and muscle cells, signals the presence of an abundance of intracellular energy, and more.
- Fats: Insulin instigates the synthesis of fatty acids in adipose tissue as well as in the liver and in the mammary glands during lactation. It also affects the metabolism of phospholipids.
- Protein: Insulin stimulates protein synthesis throughout the body. It also contributes to the transcription of mRNA as well as aiding translation of mRNA into ribosomal proteins.
In a big-picture sense, insulin’s role has to do with the regulation of the body’s cellular energy supply and the balance of micronutrients. When the body is in a fed, as opposed to fasting, state, insulin orchestrates the anabolic processes that lead to muscle growth , tissue healing, and more. Insulin signals an abundance of energy, indicating to the body that it can halt the breakdown of fat stores and instead carry out fat synthesis.
Also Check: Does Low Blood Sugar Cause High Blood Pressure
How Is Insulin Controlled
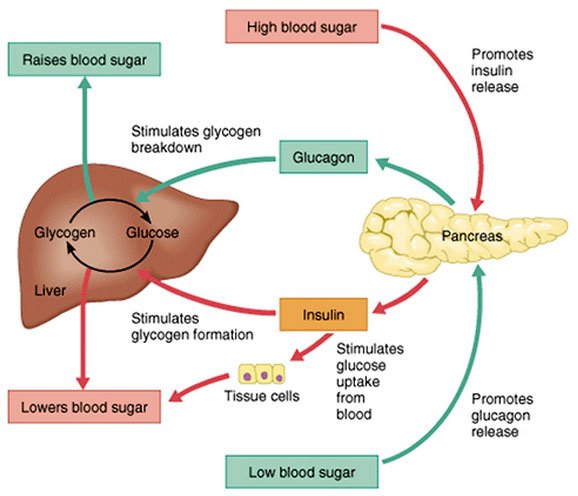
The main actions that insulin has are to allow glucose to enter cells to be used as energy and to maintain the amount of glucose found in the bloodstream within normal levels. The release of insulin is tightly regulated in healthy people in order to balance food intake and the metabolic needs of the body. This is a complex process and other hormones found in the gut and pancreas also contribute to this blood glucose regulation. When we eat food, glucose is absorbed from our gut into the bloodstream, raising blood glucose levels. This rise in blood glucose causes insulin to be released from the pancreas so glucose can move inside the cells and be used. As glucose moves inside the cells, the amount of glucose in the bloodstream returns to normal and insulin release slows down. Proteins in food and other hormones produced by the gut in response to food also stimulate insulin release. Hormones released in times of acute stress, such as adrenaline, stop the release of insulin, leading to higher blood glucose levels to help cope with the stressful event.
Insulin works in tandem with glucagon, another hormone produced by the pancreas. While insulin’s role is to lower blood sugar levels if needed, glucagon’s role is to raise blood sugar levels if they fall too low. Using this system, the body ensures that the blood glucose levels remain within set limits, which allows the body to function properly.
How Is Type 2 Diabetes Diagnosed
Doctors can say for sure if a person has diabetes by testing blood samples for glucose. Even if someone doesn’t have any symptoms of type 2 diabetes, doctors may order blood tests to check for it if the person has certain risk factors .
Some kids and teens with diabetes may go to a pediatric endocrinologist â a doctor who specializes in diagnosing and treating children and teens living with diseases of the endocrine system, such as diabetes and growth problems.
p
Don’t Miss: Blood Sugar Too High Symptoms
Is Insulin Required To Digest Proteins & Fats
Insulin is a peptide harmone, which does not directly involve in digestion of any macromolecules. insteed it act indirectly as peptide signalling harmone, what it does is it goes and binds the receptors on the cell surface and stimulates them to uptake glucose from the bloodstream into the inside of cell to undergo oxidative brakdown of glucose in to carbon dioxide and water and energy. apart from this it doesn’t stimulate uptake of any other biomolecules from blood stream except glucose. in diabetic absence of insulin, results in not activation of cells to uptake glucose from blood, hence glucose remains more and undigested in blood itself, hence this condition is called glucosemia above the normal, which is detrimental. Insulin is an anabolic hormone mainly affecting the carbohydrate metabolism. As such insulin is not involved in digestion process but yes it is involved in the metabolism of fat and proteins also. Insulin has several actions: 1. It causes the cells in the liver, muscle, and fat tissue to take up glucose from blood and convert it to glycogen that can be stored in the liver and muscles 2. Insulin also prevents the utilization of fat as an energy source. In absence of insulin or in conditions where insulin is low glucose is not taken up by body cells, and the body begins to use fat as an energy source 3. Insulin regulates the amino acid uptake by body cells.Continue reading > >
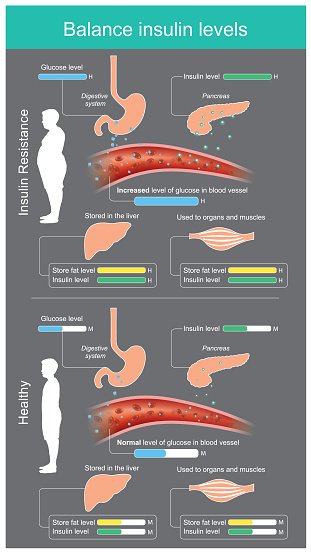
Controlling Insulin Levels And Fat Storage
So what can you do to prevent high insulin levels? Simple. If high levels of carbohydrates increase insulin levels, then it makes sense that a low carb diet would drop insulin levels. This is precisely the case. When individuals switch to a low carb diet they claim to feel more energetic and that their weight sheds off. To a certain extent both claims hold some truth.
Lower carbohydrate intake reduces insulin levels and fat storage. A low carb diet puts less stress on fat cells to buildup excess glucose from the blood. When this stress is alleviated fat cells can open their gates and release the stored up energy to be used. This is why individuals feel more energetic when they begin a low carb diet. It is the second claim that people must look at with an eye of skepticism.
Yes, the fat cells are able to release energy for the body to use. However, if that energy has no way of being used it will go back to being dormant. Use the analogy of a lazy river ride at the amusement park. The water will continue to slowly go full circle around and around and the water level will remain constant.
It is not until a path is opened for the water to drop. The gates are open, but there needs to be a void for the freely floating energy to go. So it is necessary to incorporate some exercise and is important to know that the fat will not just melt away magically. So, even though lower insulin levels release fat storage, you still need to get active for maximum fat burn.
Read Also: How Long Do Type 1 Diabetics Live
Insulin Receptors And Insulin Binding
Insulin mediates its actions through binding to insulin receptors. The insulin receptor was first characterised in 1971. It consists of a heterotetramer consisting of 2 and 2 glycoprotein subunits linked by disulphide bonds and is located on the cell membrane. The gene coding for the insulin receptor is located on the short arm of chromosome 19. Insulin binds to the extracellular subunit, resulting in conformational change enabling ATP to bind to the intracellular component of the subunit. ATP binding in turn triggers phosphorylation of the subunit conferring tyrosine kinase activity. This enables tyrosine phosphorylation of intracellular substrate proteins known as insulin responsive substrates . The IRS can then bind other signalling molecules which mediate further cellular actions of insulin.
PI 3-kinase promotes the translocation of glucose transporter proteins, glycogen, lipid and protein synthesis, anti-lipolysis and the control of hepatic gluconeogenesis. PI 3-kinase acts via serine and threonine kinases such as Akt/protein kinase B , protein kinase C and PI dependent protein kinases1& 2 . The RAS pathway activates transcription factors and stimulates the growth promoting actions of insulin. Thus broadly, PI 3-kinase mediates insulins metabolic effects, e.g. cellular glucose uptake, while RAS significantly mediates insulins mitogenic effects, together with other less well described actions. These pathways are presented schematically in .
Common Conditions Associated With Insulin Resistance
Type 2 Diabetes
Following pioneering work by Bornstein and the Nobel Prize-winning work of Yalow and Berson, the first insulin assays became widely available in the late 1960s it was subsequently confirmed that diabetic patients with so-called or maturity onset or type 2 diabetes had normal or increased plasma insulin levels. Insulin resistance was reported to be a characteristic feature of T2DM in the early 1970s. A progressive inability of the cells to compensate for the prevailing insulin resistance by sufficient hyperinsulinaemia, heralds the clinical onset of this disorder. While twin studies and linkage analyses are consistent with a strong genetic component in the development of type 2 diabetes, several decades of research have failed to identify a predominant genetic abnormality in the majority of cases. The aetiology of T2DM is thought to be polygenic, with environmental factors being superimposed upon this basic predisposition.
Insulin resistance typically predates the development of diabetes and is commonly found in unaffected first-degree relatives. The morbidity of the disorder relates both to the severity of hyperglycaemia and the metabolic consequences of insulin resistance itself. The primary defects in insulin action appear to be in muscle cells and adipocytes, with impaired GLUT 4 translocation resulting in impaired insulin-mediated glucose transport.
Metabolic Syndrome
-
Abdominal obesity
Men < 40 mg/dL
Women < 50 mg/dL
Dyslipidaemia
Hypertension
PCOS
OSA
Read Also: Max Dosage Metformin
Insulin And Blood Glucose Levels
Insulin helps control blood glucose levels by signaling the liver and muscle and fat cells to take in glucose from the blood. Insulin therefore helps cells to take in glucose to be used for energy.
If the body has sufficient energy, insulin signals the liver to take up glucose and store it as glycogen.
The liver can store up to around 5% of its mass as glycogen.
Some cells in the body can take glucose from the blood without insulin, but most cells do require insulin to be present.
How Insulin Is Made
Insulin is produced by the pancreas, a glandlike organ nestled in the curve of the duodenum , just behind the stomach. The pancreas functions both as an exocrine gland and an endocrine gland.
The exocrine function of the pancreas basically is to help with digestion. It’s in the role as an endocrine gland that the pancreas produces insulin, as well as another hormone called glucagon. The pancreatic cells that produce glucagon are called alpha cells.
Insulin is produced by specialized beta cells in the pancreas, which are clustered into groups called islets of Langerhans. A healthy adult pancreas has approximately one million islets, taking up about 5% of the entire organ.
Don’t Miss: Hypoglycemia Turning Into Diabetes
Factors Influencing Insulin Biosynthesis And Release
Insulin secretion may be influenced by alterations in synthesis at the level of gene transcription, translation, and post-translational modification in the Golgi as well as by factors influencing insulin release from secretory granules. Longer-term modification may occur via influences on cell mass and differentiation. Given insulins pivotal role in glucose utilisation and metabolism, it is not surprising that glucose has multiple influences on insulin biosynthesis and secretion. However, other factors such as amino acids, fatty acids, acetylcholine, pituitary adenylate cyclase-activating polypeptide , glucose-dependent insulinotropic polypeptide , glucagon-like peptide-1 , and several other agonists, together in combination, also influence these processes.
Production Of Digestive Enzymes
The pancreas produces secretions necessary for you to digest food. The enzymes in these secretions allow your body to digest protein, fat and starch from your food. The enzymes are produced in the acinar cells which make up most of the pancreas. From the acinar cells the enzymes flow down various channels into the pancreatic duct and then out into the duodenum. The secretions are alkaline to balance the acidic juices and partially digested food coming into the duodenum from the stomach.
Read Also: What Is A High Blood Sugar Reading
How Does Insulin Regulate Blood Glucose Levels
The primary function of the insulin hormone is to manage blood sugar levels by helping the cells of our body absorb it for their energetic needs.
As we do not always consume the exact amount of glucose our organism needs, and sometimes it may exceed the required level, insulin signals the brain about the necessity to store the excess sugar. As a rule, it is accumulated in the tissues of the liver as well as in the adipose tissue. When the level of sugar drops or there is a need for a quick additional source of energy , or when we are stressed, the organism will use this depot.
What Happens If I Have Too Much Insulin
If a person accidentally injects more insulin than required, e.g. because they expend more energy or eat less food than they anticipated, cells will take in too much glucose from the blood. This leads to abnormally low blood glucose levels . The body reacts to hypoglycaemia by releasing stored glucose from the liver in an attempt to bring the levels back to normal. Low glucose levels in the blood can make a person feel ill.
The body mounts an initial ‘fight back’ response to hypoglycaemia through a specialised set of of nerves called the sympathetic nervous system. This causes palpitations, sweating, hunger, anxiety, tremor and pale complexion that usually warn the person about the low blood glucose level so this can be treated. However, if the initial blood glucose level is too low or if it is not treated promptly and continues to drop, the brain will be affected too because it depends almost entirely on glucose as a source of energy to function properly. This can cause dizziness, confusion, fits and even coma in severe cases.
Some drugs used for people with type 2 diabetes, including sulphonylureas and meglitinides , can also stimulate insulin production within the body and can also cause hypoglycaemia. The body responds in the same way as if excess insulin has been given by injection.
Read Also: What Happens If A Diabetic Eats Too Much Sugar
Produced In The Pancreas
When you eat, food travels to your stomach and small intestines, where its broken down into nutrients that include glucose. The nutrients are absorbed and distributed via your bloodstream.
The pancreas is a gland located behind your stomach that performs an essential role in the digestion process. It creates enzymes that break down the fat, starches, and sugar in the food. It also secretes insulin and other hormones into your bloodstream.
Insulin is created in the beta cells of the pancreas. Beta cells comprise about 75% of pancreatic hormone cells.
Other hormones produced by the pancreas are:
- glucagon, which alerts your liver to raise your blood sugar if it gets too low
- gastrin, which stimulates the production of gastric acid in your stomach
- amylin, which helps control your appetite
Regulation Of Insulin Translation
In response to nutrients, -cells enhance their overall speed of protein translation, which is at least partly controlled by dephosphorylation of eukaryotic initiation factor 2a via protein phosphatase 1 . For example, exposure of -cells to high glucose for 2 hours significantly decreases the ratio of phosphorylated eIF2a to eIF2a . However, there are additional mechanisms to regulate glucose-induced insulin translation, since the overall protein translation induced by glucose compared to the fasting state in -cells was only 3-fold compared with an up to 8-fold induction in proinsulin translation .
Also Check: Diabetes And Orthostatic Hypotension
What Are The Different Types Of Insulin
The American Diabetes Association characterizes insulin by how fast it works. But everyones body is different. If you have diabetes, you should expect deviations in the amount of time any medication takes to reach your bloodstream.
Here are 8 different types of Insulin and how they work.
- Onset is defined as the length of time before insulin hits your bloodstream and begins to lower blood glucose.
- Peak is the time during which insulin is at its maximum effectiveness at lowering your blood glucose levels.
- Duration is the length of time insulin continues to lower your blood glucose levels.
- Rapid-acting insulin begins to affect blood glucose approximately 15 minutes after injection. It peaks in about an hour, and then continues to work for a few more.
- Short-acting insulin reaches your bloodstream within 30 minutes of injection. It peaks in the 2-3-hour range and stays effective for 3-6 hours.
- Intermediate-acting insulin includes NPH insulin which helps control glucose for 10-12 hours. A protamine is a type of protein that slows the action of this insulin.
- Long-acting insulin enters the bloodstream 1-2 hours after injection and may be effective for as long as 24 hours. An advantage to long-acting insulin is there is no pronounced peak, and it works more like typical pancreatic insulin.
- Premixed/combination insulin contains a mix of rapid- or short-acting insulin combined with an intermediate-acting insulin. This eliminates the need to draw insulin from more than one bottle.

