I Survived An Insulin Overdose
Trigger Warning: Contains content related to self-harm and diabetes burnout.
Im now 33, having been diagnosed right before I turned 4. I dont understand a normal life. Each time Im asked what would I do if diabetes was cured, Im at a loss for words.
Growing up, I did normal things. I played sports, even went on to be a starting soccer player in college. I drove fast cars, got invited to parties, had great friends. What was missing was all mental. That lead to a very dark path.
This path consumed me and took me into a depression. In my early 20s, all I could imagine was how much money I would save without diabetes, how I could keep a girlfriend without her being afraid of my illness. How I could travel and not worry. These thoughts made the depression worse.
Into my mid-twenties, I found out I was going to be a father. The joy and excitement that should come along with this was soon overshadowed by the what-ifs: What if I never get to see him graduate school? What if I cant be there for him because diabetes took me to soon? What if when he needs me most Im having a low and am incoherent?
With these questions looming, I reached a point of no hope, no light at the end of the tunnel. It was better to leave the earth then before he truly needed me later. Trust me, I know it sounds selfish. It is. When you are clouded by thoughts of a lifelong illness, the depression that comes along with it takes hold of everything.
Usual Adult Dose For Diabetes Type 1
Note: Regular human insulin is available in 2 concentrations: 100 units of insulin per mL and 500 units of insulin per mL Doses should be individualized based on patient’s metabolic needs, blood glucose monitoring results, and glycemic goals-Total daily insulin requirements are generally between 0.5 to 1 unit/kg/dayInsulin U-100 :SUBCUTANEOUS Administration: Inject subcutaneously approximately 30 minutes prior to a meal-Insulin U-100 should generally be used in a regimen with an intermediate or long-acting insulinINTRAVENOUS Administration: Administer only under medical supervision with close monitoring of blood glucose and serum potassium-Humulin R: Dilute to a concentration of 0.1 to 1 unit/mL in an infusion system using polyvinyl chloride infusion bags; this insulin is stable in normal saline-Novolin R: Dilute to a concentration of 0.05 to 1 unit/mL in an infusion system using polypropylene infusion bags; this insulin is stable in normal saline, 5% dextrose, or 10% dextrose with 40 mmol/L potassium chlorideInsulin U-500 : For subcutaneous administration only-Administer U-500 insulin subcutaneously 2 to 3 times a day approximately 30 minutes prior to start of a meal–The safety and efficacy in combination with other insulins has not been determined.
Analysis Of Tk/td Relationships
We conducted a TK/TD analysis between the glucose infusion rate in order to normalize the capillary glucose concentration and the corresponding serum insulin concentrations . This study was approved by our institutional ethics committee, and verbal informed consent was obtained from the patient when conscious or from the next of kin when not.
What Can Cause An Insulin Overdose
Insulin overdoses can occur for a number of reasons. Some common reasons are listed below:
- Miscalculating the carb content of a meal
- Missing out or delaying a scheduled meal or snack after having injected
- Accidentally injecting twice for the same meal or snack
- Accidentally injecting the dosage number of a different meal
- Accidentally injecting the wrong insulin for example injecting your rapid acting insulin instead of your long acting insulin
- Having difficulty seeing the numbers or gradation on an insulin pen or syringe
Type 1 Diabetes Mellitus
Rapid-acting human insulin analogue indicated to improve glycemic control in patients with diabetes mellitus
<3 years: Safety and efficacy not established
3 years: 0.4-1 units/kg/day SC of total insulin with higher amounts required during puberty; otherwise, use adult dosing
See also Administration
Safety and efficacy not established
Overdose During A Suicide Attempt
Hypoglycemic Encephalopathy Caused by Insulin Aspart , he was awake and blood glucose was 40 mg/dl. He received a total glucose load of 230 g in the first 15 hours. Head CT was not remarkable. He was discharged on day 14. Three weeks later, he was found in a deep coma. He had injected 900 units of insulin aspart in a suicide attempt 8 hours prior to be found. On arrival, he was comatose and his blood glucose was 19 mg/dl. Head CT revealed low density areas throughout the cerebral cortex and partial cerebral edema. He received a total glucose load of 270 g in the first 22 hours. A repeat head CT examination on day 9, revealed worsening of the findings throughout the cerebral cortex. He fell into an apallic syndrome and was transferred to a local hospital.In the second overdose, the patient rapidly developed a sustained hypoglycemia, and fell into hypoglycemic encephalopathy because of the delay in receiving appropriate treatment. We consider that insulin aspart overdose may, in fact, predispose to hypoglycemic encephalopathy compared with long-acting insulin. Keywords: Rapid-acting insulin; Acute poisoning; Diabetes Mellitus Introduction Reports of intentional massive overdoses of rapid-acting insulin are infrequent . No case reports are found in the literature documenting hypoglycemicContinue reading >>
Prosecutor: Woman Gave Autistic Daughter Lethal Insulin Dose
EASTLAKE, OHIO: An Ohio woman has pleaded guilty to involuntary manslaughter after prosecutors say she gave her autistic 21-year-old daughter a fatal dose of insulin and did not call for help. The News-Herald reports Sandra Speck, of Eastlake, pleaded guilty Monday and will be sentenced June 19. Prosecutor Rocco DiPierro says hell recommend that she serve no more than four years. DiPierro says Specks daughter, Mindy, was prone to violent outbursts and was particularly aggressive the day she died. He says Speck gave her insulin because her blood sugar was too high, but then gave her additional doses when she would not calm down. Speck says she fell asleep beside her unconscious daughter before she could give her a soft drink to counteract the insulin. She called police the next day.Continue reading >>
The Carbohydrate Cure: Approach To Insulin Overdose
Ashley Gray, MDBrown University, Emergency Medicine ResidencyA 60 year-old diabetic female is brought in by ambulance after injecting herself with 600 units subcutaneous Humalog just prior to calling 911. On arrival, she has a blood sugar of 31 and has tachycardia and tremor. What is the next step in care?
How To Prevent Insulin Overdoses
- Take care when calculating meal time insulin. Taking an extra couple of minutes to be sure of your dose will save the time and hassle of an overdose.
- Never be tempted to delay your meal or snack if you have injected.
- Dont inject whilst doing other tasks, such as watching the TV, holding a conversation or performing another task as this raises the chance that you may forget your injection has been done. Concentrate solely on giving the injection
- Be careful of injecting insulin when you are hypo as mistakes are more likely to be made. Ideally, ensure your blood glucose has risen to safe levels and then put in your scheduled insulin dose.
- Ask for help if you have difficulty seeing the numbers or gradations on your insulin pen or syringe. See also our page on diabetes and visual impairment which lists a number of injection aids for people that have visual impairments
Causes Of An Accidental Insulin Overdose
In life with diabetes, trying to balance your insulin needs with the variables of food, activity, stress, weight management, etc. is a constant challenge. Just one or two units of insulin more than your body needs can easily lead to even the earliest symptoms of an overdose.
Here are the general causes of an accidental insulin overdose:
- Taking a dose of insulin for your meal twice
- Taking your long-acting insulin twice in one day when you normally take it once
- Taking insulin for a planned meal but forgetting to eat
- Overestimating the amount of insulin needed for a meal
- Overestimating the amount of insulin needed to correct a high blood sugar
- Exercising with too much insulin in your bloodstream / not enough glucose
- Taking your rapid-acting insulin instead of your long-acting, or vice versa
- Prescribed an insulin dose that doesnt fit your bodys needs
- Changes in your insulin sensitivity like losing weight, improved diet, decreased stress, exercising more, etc.
- Taking insulin for a high-carb/high-fat meal that digests too slowly to match the peak of your insulin
Insulin Overdose Among Patients With Diabetes: A Readily Available Means Of Suicide
Go to: CASE VIGNETTE Ms A, an 18-year-old woman with insulin-dependent diabetes, was found by her brother while having a generalized tonic-clonic seizure . He called emergency rescue services, who determined that her fingerstick glucose level was 25 mg/dL and brought her to the emergency department. Her glucose level was stabilized in the emergency department, and she was transferred to the medical service for further observation before transfer to an inpatient psychiatric unit. Although Ms A had not received any psychiatric treatment before this event, she reported infrequent panic attacks and moderate social anxiety, and she used cannabis and clonazepam daily. Ms A had attempted suicide twice in the past several months; both of these attempts involved overdoses of insulin, and neither resulted in her receiving medical attention. For several years, she had been poorly adherent with her insulin regimen . Ms A, who lived at home with her mother, father, and brother, was failing several classes in her senior year of high school, and she had recently quit the soccer team.Continue reading >>
Insulin Toxicokinetic/toxicodynamic Relationships In Acute Intoxications
TK/TD relationships allow descriptive and quantitative characterization of the time course of in vivo drug effect in relation to its corresponding drug concentration within an individual . To our knowledge, there is no case of human insulin poisoning with a TK/TD analysis addressing the effects of insulin on glycaemia. We used the glucose infusion rate as a surrogate marker of the severity of hypoglycaemia. In the six patients the maximal glucose infusion rate was associated with a wide range of insulin concentrations, suggesting a saturable toxic mechanism at these high concentrations. Consistent with this, insulin-stimulated glucose flux is a saturable, receptor-mediated process with a nonlinear dose-effect curve . The range of insulin concentrations accompanied by a decrease in glucose infusion rate was highly variable, enhancing the weak prognostic value of circulating insulin concentration. In contrast, the rate of glucose infusion decreased only when plasma insulin concentrations dropped dramatically. Our findings clearly demonstrate that prompt recognition and adequate treatment of the hypoglycaemic events is the key to achieving a successful outcome.
Treating An Insulin Overdose

How you treat an insulin overdose depends on how much excess insulin was dosed. If it was just a few units and youre mentally clear and capable of feeding yourself, the low blood sugar should be easily corrected with a small snack.
The greater the overdose of insulin is, the more likely youll need more serious medical intervention.
Lets take a closer look.
Prognosis Of Severe Acute Insulin Poisoning
Prognostic factors in insulin poisoning are subject to debate. It is generally accepted that the severity of intoxication should be assessed based on clinical findings rather than on any speculated amount of self-injected insulin . The interval between insulin self-injection and initiation of therapy and the duration of the hypoglycaemic coma were proposed to be relevant prognostic factors . Our findings were consistent with the reported literature in that we identified two independent outcome predictors: delayed initiation of dextrose infusion and duration of mechanical ventilation . Interestingly, as in our study, the dose and type of insulin were found to be closely related to the duration but not to the severity of hypoglycaemia . It should be noted that patients may become hypoglycaemic much later than predicted based on the conventional duration of action of insulin preparations .
Is There A Maximum Insulin Glargine Dose
Is there a maximum insulin glargine single-injection dose? Anecdotally, I have heard that patients receiving more than 50 units should split the dose from daily dosing to twice-daily. Whats the evidence?
The question of a maximum insulin glargine dose is not straightforward because it encompasses several issues:
Pharmacodynamics and Duration of Insulin GlargineEfficacy of Daily versus Twice-Daily Lantus Administration
- The primary endpoint, mean evening blood glucose , was not different between daily and twice-daily dosing
- The mean 24-hour blood glucose was lower with twice-daily dosing
- There was no difference in hypoglycemic events between the two dosing regimens
Maximum Single-Injection Subcutaneous DoseVolume LimitationsTypes of SyringesLantus SoloStar PenLantus SoloStar disposable penOne source Maximum Doses are Expert Opinion At Best
- Volumes greater than 0.5 mL should be split and injected in separate areas to facilitate absorption
- Because insulin glargine is typically dosed once daily, however, the potential for injecting large doses of insulin at one site is high, and doing so can lead to poor absorption and decreased efficacy, or lipodystrophy
References
Symptoms Of An Insulin Overdose
Early symptoms of an insulin overdose are the same as symptoms of low blood sugar.
The American Diabetes Association lists the following as symptoms of low blood sugar:
- Feeling shaky
- Color draining from the skin
- Feeling Sleepy
- Feeling weak or having no energy
- Blurred/impaired vision
- Tingling or numbness in the lips, tongue, or cheeks
- Headaches
- Nightmares or crying out during sleep
Severe hypoglycemia from an insulin overdose can lead to:
- Being unable to talk, chew, or swallow
- Losing consciousness because your brain isnt getting the glucose it needs to function
- Seizures because your brain isnt getting the glucose it needs to function
- Death because every part of your part requires glucose in order to function
Forensic Histopathology And Immunohistochemistry
A detailed histological examination of all internal organs, especially of the pancreas and liver, aiming at detection of insulinoma and morphological symptoms of hypoglycemia, respectively, should be always performed by experienced pathologist. The content of glycogen in the liver may be evaluated by the Periodic Acid-Schiff or Bests Carmine staining. Its low amounts can indirectly confirm insulin overdose, as it was presented in the first case . Another useful option is to perform IHC staining for the presence of insulin at the injection site. It is not necessary to buy special antibodies. These routinely used in clinical histopathology can be successfully used for this purpose, as we demonstrated in the second case .
Type 1 Or 2 Diabetes Mellitus
Rapid-acting human insulin analogue indicated to improve glycemic control in patients with type 1 or 2 diabetes mellitus
Type 1 diabetes mellitus
- Usual daily maintenance range is 0.5-1 unit/kg/day in divided doses; nonobese may require 0.4-0.6 unit/kg/day; obese may require 0.8-1.2 units/kg/day
- Intermediate- or long-acting insulin: Approximately one-third of the total daily insulin requirements SC
- Rapid-acting or short-acting, premeal insulin should be used to satisfy the remainder of the daily insulin requirements
Type 2 diabetes mellitus
- Intermediate- or long-acting insulin: 10 units/day SC at bedtime generally recommended
- Short-acting insulin: If necessary, start up to 4 units, 0.1 unit/kg SC within 15 min before each meal, or 10% basal dose; if A1C <8%, consider decreasing basal insulin dose by same amount
- Increase by 1-2 units or 10-15% qWeek or q2Weeks once self-monitoring of blood glucose is achieved
Proper Administration Human Growth Hormone Dosages
Growth Hormone possesses an odd varying half-life of around 30 minutes following injection, as the majority of its effects are resultant from the IGF-1 release signaled to the liver by Human Growth Hormone. Therefore, individuals can choose whether to inject their full dose at once or split it up during the day. Both options are acceptable and neither has been found to hold any advantage over the other except for personal experience, preference, and convenience. Human Growth Hormone is designed for subcutaneous administration primarily , but can also be administered .
An important note to be made is the fact that Human Growth Hormones fat loss effects are not expressed in the subcutaneous area it is injected in fat loss as a result of Human Growth Hormone occurs systemically, and there is no such thing as spot reduction with Growth Hormone despite what rumors may circulate about it. Following injection into subcutaneous tissue, the Human Growth Hormone is carried into the bloodstream where it first travels to the liver before exhibiting its effects on the body.
Bacteriostatic water: When reconstituted with bacteriostatic water , Human Growth Hormone possesses a shelf-life of approximately 2 weeks to 20 days .
Sterile water: When reconstituted with sterile water , Human Growth Hormone possesses a shelf-life of approximately 5 days .
Ohio Mother Gives Autistic Daughter Lethal Insulin Dose
EASTLAKE, Ohio An Ohio woman has pleaded guilty to involuntary manslaughter after prosecutors say she gave her autistic 21-year-old daughter a fatal dose of insulin and did not call for help. The News-Herald reports Sandra Speck, of Eastlake, pleaded guilty Monday and will be sentenced June 19. Prosecutor Rocco DiPierro says he’ll recommend that she serve no more than four years. DiPierro says Speck’s daughter, Mindy, was prone to violent outbursts and was particularly aggressive the day she died. He says Speck gave her insulin because her blood sugar was too high, but then gave her additional doses when she would not calm down. Speck says she fell asleep beside her unconscious daughter before she could give her a soft drink to counteract the insulin. She called police the next day.Continue reading >>
Intentional Overdose As A Method Of Suicide

Overdosing insulin has been used as a method of attempted suicide by both people with diabetes and non-diabetics. Because people with diabetes face an increased risk of depression, its important to note that overdosing insulin is not a smooth or guaranteed death.
Instead, in many cases, your liver saves you by releasing a large dose of glycogen which is converted into glucose .
However, that doesnt mean a full recovery is guaranteed either. Many patients who attempt suicide by insulin overdose suffer longterm neurological damage that can affect your speech and motor skills.
If you are contemplating or planning suicide, call the National Suicide Prevention Hotline immediately: 1-800-273-8255, available 24 hours a day, 7 days a week.
Suggested next post: What Low Blood Sugar Feels Like
If you found this guide to insulin overdoses useful, please sign up for our newsletter using the form below. We send out a weekly newsletter with the latest posts and recipes from Diabetes Strong.
Clinical Toxicology Of Insulin Poisoning
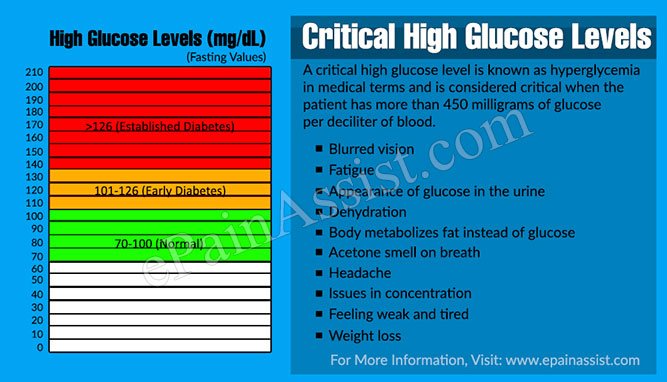
An overdose of insulin is a potential life-threatening condition and requires urgent medical attention . The clinical manifestations of hypoglycemia occur when the blood glucose level is less than 2.22.8 mmol/l . Symptomatology includes two groups of symptoms. The first one is caused by stimulation of the autonomic nervous system and includes profuse sweating, anxiety, tremor, and hunger. The second one is caused by progressive dysfunction of the central nervous system due to neuroglycopenia and includes nausea, headache, dizziness, blurred vision, abnormal intellectual processes, behavioral disturbances, and finally loss of consciousness, convulsions, and death.
The most optimal place of the treatment is clinical toxicology ward, but patients who are overdosed with insulin can be also treated in typical intensive care units or in less serious casesin general internal wards. To differentiate endogenous and exogenous insulin overdose, usually insulin/C-peptide ratio is used, both in clinical and forensic settings . Physiologically for every molecule of insulin formed, a corresponding molecule of C-peptide is formed. If the above-described ratio is >1, it indicates exogenous origin of insulin . However, it should be remembered that C-peptide is very unstable in postmortem blood .
How To Avoid An Insulin Overdose
There are many steps you can take to avoid an accidental insulin overdose. Most of them revolve around avoiding mistakes when you take your insulin and remembering when you took your insulin and how much you took
- Keep an insulin log. If you log every insulin injection, you are much less likely to mistakenly inject the wrong amount of insulin or inject twice. There are many phone apps that will help you calculate your insulin needs and log your injections. Most insulin pumps and smartpens can also do this automatically.
- Always double-check that you are using the right type of insulin. Accidentally using fast-acting insulin when you were supposed to use long-acting insulin can lead to an insulin overdose.
- Dont forget to eat. If you take fast-acting insulin for a meal, you also need to actually eat the meal. Dont take your insulin until you know the meal is on its way and that you have time to eat it.
Descriptive Analysis And Study Of Prognostic Factors
Over a 6-year period, 25 patients were admitted in our ICU because of intentional insulin poisoning. A past psychiatric history was noted in 20 of the 25 patients and diabetes mellitus in 13 of the 25 patients . The five nondiabetic patients were nurses. Rapid-acting insulin was involved in 14 out of 25 patients, while intermediate-acting or slow-acting insulin was used by 13 out of 25 patients. Two patients self-injected both insulin types. Drug ingestion, mainly benzodiazepines, was also identified in 68% of patients. The interval between insulin self-injection and pre-hospital glucose administration was 2.7 hours. At presentation, Glasgow Coma Scale score was 9 , systolic blood pressure was 120 mmHg, pulse rate was 95 beats/minute and respiratory rate was 20 breaths/minute. The temperature was 36.0°C . At the scene, the capillary glucose concentration was 1.4 mmol/l. Six patients were mechanically ventilated for persistent coma despite correction of hypoglycaemia. On ICU admission, the blood glucose was 5.3 mmol/l, plasma potassium was 3.3 mmol/l, plasma lactate 2.0 mmol/l, and the maximal observed plasma insulin concentration was 197 IU/ml.
Table 1 Comparison of patient clinical parameters according to the outcome
Insulin Kinetics In Acute Intoxication
Study of the kinetics of self-injected insulin is difficult, particularly in nondiabetic patients, because of the presence of endogenous insulin. Thus, in order to interpret accurately the insulin levels and to study the disappearance of exogenous insulin from circulation, we used the level of peptide C as a surrogate, the value of which has previously been demonstrated . We considered the existence of suppressed C-peptide immunoreactivity and a molar ratio of insulin to C-peptide of less than 1 to represent assurance of reliable measurement of exogenous insulin .
The kinetics of insulin follow a multi-compartmental course, with a terminal plasma half-life of 10 to 20 minutes . Insulin metabolism is dependent on hepatic and renal functions, with a small contribution made by muscle and adipose tissue . Using a non-compartmental analysis in a case of insulin intoxication in a type 1 diabetic patient, Shibutani and Ogawa found an elimination half-life of 6.2 hours. In another insulin-poisoned type 1 diabetic patient, Fasching and coworkers identified a biphasic slow decline, with apparent half-lives of 4 hours and 10 hours for the two successive phases, respectively. In our patients, we identified late half-lives ranging from 0.8 to 11.7 hours, depending on the insulin type.

