Intravenous Insulin Protocol Selection
Multiple intensive insulin protocols have been developed to manage hyperglycemia however, no singular protocol has been universally accepted. Significant similarities in strategy exist among the various protocols, and the differences relate to bolus amounts, infusion rates, and target glucose goals. The complexity of these differences can be better appreciated in the summary of variations of protocols outlined below.
Areas of variation in insulin protocols are as follows:
-
Presence or absence of preexisting diabetes
-
Initial hyperglycemic threshold
-
Initial bolus insulin dose
-
Subsequent bolus insulin
-
Change in insulin dose
-
Based on direction of change in glucose
-
Velocity of change
-
Dose adjustment for insulin resistance
-
Basis of change in insulin dose
-
Unit of change in insulin dose
-
Number of steps required some requiring calculations to change the dose
Target glucose level
Logistics of implementation are as follows:
-
Paper vs computerized vs web-based protocols
-
Nurse-driven, with varying physician input
-
Adherence to protocol or allowance for changes in protocol
-
Differences in frequency of glucose monitoring
-
Differences in requirement of a constant glucose source
-
Adjustments for hypoglycemia
-
Average time to goal
Two archetypal approaches are presented in more detail: the Georgia Hospital Association Protocol , also referred to as the Davidson or Glucommander Protocol, and the Portland Protocol.
Examples Of Recent Errors
Several recent insulin errors during hyperkalemia treatment have been reported to ISMP or have appeared in the literature. For example, just this month, we learned about an error in which a nurse correctly calculated the volume needed for a 10 unit dose of insulin lispro, but accidentally measured out 20 units of insulin using a 10 mL non-insulin syringe. A physician prescribed treatment that included calcium gluconate 1 g IV, insulin lispro 10 units IV, and dextrose 50% IV. The nurse calculated that she would need 0.1 mL of the insulin for the 10 unit dose, and a nurse manager verified the calculation. Using a 10 mL syringe, she drew the insulin lispro into the syringe up to the first gradation mark, believing this represented 0.1 mL. But the first syringe marking was actually 0.2 mL. The nurse manager did not verify the dose in the syringe prior to administration. The error was quickly discovered when a clinical nurse specialist asked the nurse, who had just completed orientation, to demonstrate how she had measured the insulin dose in a 10 mL syringe. The patients blood glucose was monitored, and she experienced no adverse effects.
Cii Versus Sliding Scale
In critically ill patients, insulin is necessary to achieve a reduction inblood glucose levels. Using intravenous insulin in the absence of glucoselowering will have no effect on outcomes. The Diabetes and Insulin-GlucoseInfusion in Acute Myocardial Infarction studydemonstrated that, in patients suffering an acute myocardial infarctionregardless of a history of diabetes, IV insulin therapy for 24 hours followedby intensive subcutaneous therapy for 3 months improved long-termsurvival. The follow-up DIGAMI 2study wasdesigned to evaluate the relative benefit of long-term tight glycemicmanagement. Although the investigators failed to demonstrate significantdifferences in glucose control and mortality among the three treatment arms,they did illustrate the association between higher glucose levels andincreased risk of death. Thus, merely administering insulin without loweringglucose levels will not improve outcomes.
CII is the only delivery method specifically developed for inpatient useand is preferred over the subcutaneous route for several clinical indications. The only type ofinsulin that should be given intravenously is human regular insulin. There isno advantage to using rapid-acting analogs in preparing insulin infusionsbecause the rate of absorption is no longer a factor when administeringinsulin intravenously and can only result in added costs to theinstitution.
Table 2.
Common Indications for IV InsulinTherapy,
Don’t Miss: Complications Of Metformin
Insulin Regular May Interact With Other Medications
Insulin regular injectable solution can interact with several other medications. Different interactions can cause different effects. For instance, some can interfere with how well a drug works, while others can cause increased side effects.
Below is a list of medications that can interact with insulin regular . This list does not contain all drugs that may interact with insulin regular .
Before taking insulin regular , be sure to tell your doctor and pharmacist about all prescription, over-the-counter, and other drugs you take. Also tell them about any vitamins, herbs, and supplements you use. Sharing this information can help you avoid potential interactions.
If you have questions about drug interactions that may affect you, ask your doctor or pharmacist.
Humalog For Type 1 Diabetes
Humalog is FDA-approved to help control blood sugar levels in people with type 1 diabetes. This includes adults as well as children ages 3 years and older.
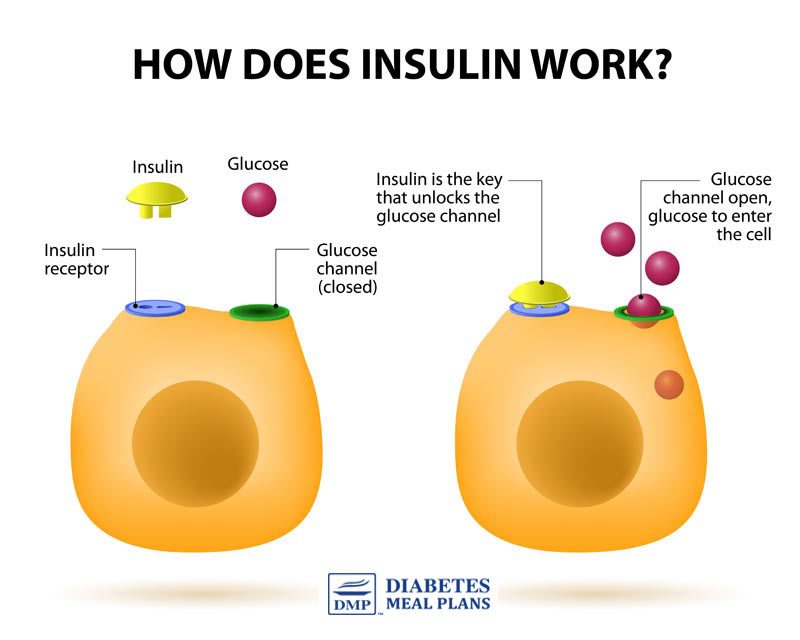
Type 1 diabetes explained
Type 1 diabetes is a life-long condition in which your pancreas doesnt make a hormone called insulin. Insulin helps your body process glucose . Without insulin, your blood sugar levels can rise too high, and this can damage cells in your body.
High blood sugar levels can lead to problems in various parts of your body, especially your eyes, kidneys, and nerves. The problems can include damage to those areas.
If you have type 1 diabetes, you need to take insulin to manage your blood sugar and prevent it from getting too high.
Humalog explained
Humalog is an insulin medication. There are two different types: Humalog and Humalog Mix.
Humalog contains insulin lispro, which is a rapid-acting insulin analog. This form of insulin works very quickly. You take it at mealtimes to help manage the surge in blood sugar that can occur after eating.
Humalog Mix contains a premixed combination of insulin lispro and a longer-acting insulin called insulin lispro protamine. Humalog Mix works very quickly, but it lasts longer than Humalog. Humalog Mix helps control mealtime surges in blood sugar and then helps manage blood sugar between meals or at night. Each dose of Humalog Mix is intended to cover two meals or one meal and a snack.
Effectiveness for type 1 diabetes
Mealtime injections
Insulin pump use
Read Also: Do Bananas Affect Blood Sugar
Rx Severe Hyperkalemia: Potassium Elimination
dialysis vs. kaliuresis
- Ultimately, most patients will require elimination of excess potassium from the body. This may be achieved either via the kidneys or via dialysis.
- Patients with end-stage renal disease on chronic dialysis will require emergent dialysis . For most other patients, kaliuresis should be attempted prior to emergent dialysis.
kaliuresis step #1 = volume resuscitation if hypovolemic
- Many patients present with renal failure and hyperkalemia due to volume depletion. The first step in managing these patients is volume repletion.
- Isotonic bicarbonate is the preferred resuscitative fluid in metabolic acidosis .
- The isotonic bicarbonate should be dosed with the goal of bringing the patients serum bicarbonate level back to a high-normal level . The dose can be estimated by calculating the patients bicarbonate deficit . Divide the bicarbonate deficit by 150 to estimate the number of liters of isotonic bicarbonate needed. The dose is usually 1-2 liters.
- Bicarbonate should be infused rapidly for patients with hypovolemia and severe hyperkalemia .
- If the patient remains hypovolemic after receiving enough sodium bicarbonate to normalize the serum bicarbonate level, then residual hypovolemia can be treated with lactated ringers.
kaliuresis step #2 = consider fludrocortisone
kaliuresis step #3 = diuretic cocktail
Indications For Intravenous Insulin
Because of their susceptibility to deep wound infections, patients who undergo open cardiac surgery may benefit from the routine use of intravenous insulin. Patients with diabetes who have suboptimal glucose control with conventional subcutaneous insulin treatment may also benefit from intravenous therapy.
Don’t Miss: Somatostatin D Cells
Target Blood Glucose Levels
The optimal range of glucose control in critically ill patients remains to be determined. A blood glucose level between 140 and 180 mg/dL is recommended for most of these patients. Certain subgroups, such as those undergoing cardiothoracic surgery, may benefit from a lower target range . Reduction of glucose levels to below 110 mg/dL is no longer recommended because of the risk of hypoglycemic complications.
Association Between Hyperkalemia And Outcomes
The potassium ion is the most abundant cation in the body. There is an estimated total reserve of 30004000 mmol in adults, of which only 60 mmol are extracellular . Hyperkalemia is associated with poor outcomes in many different settings: in the general population , in patients with cardiac and renal disease and in critically ill patients . In a retrospective study of hospitalized patients, Khanagavi et al. found that acute kidney injury and prolonged hyperkalemia are independent predictors of in-hospital mortality. In acute myocardial infarction, a serum potassium above 4.5 mmol/L is associated with a higher mortality . More recently, Legrand et al. identified that a serum potassium> 4.5 mmol/L in heart failure patients admitted to the emergency department is associated with an increased risk of death.
The net effect is a U-shaped mortality curve associated with potassium abnormalities . Several observational studies have identified hypokalemia as an independent risk factor for poor outcome . This association raises concern regarding the potential for overcorrection, as may occur with some fast-acting potassium-lowering agents. However, these associations do not mean causality and thresholds for treating hyperkalemia remain debated.
Recommended Reading: Pancreas Alpha Cell
Dosage For Type 1 Diabetes
The product information for Humalog and Humalog Mix doesnt give exact dosage recommendations for treating type 1 diabetes. Thats because the recommended dosage depends on many individual factors, including those listed above.
Your doctor will calculate your total daily insulin dosage, based on how much you weigh. According to the American Diabetes Association, a typical daily insulin dosage for type 1 diabetes is about 0.4 to 1.0 unit of insulin for each kilogram of your body weight.
Most people take about half their daily insulin dose as a fast-acting insulin, such as Humalog, at mealtimes. They take the rest as an intermediate- or long-acting insulin once or twice a day.
Youll typically take Humalog up to 15 minutes before each meal or right after each meal. How much Humalog you should take with each meal may vary. Your healthcare provider will teach you how to adjust your dose. The dosage is typically based on your premeal blood sugar level, the amount of carbohydrates in your meal, and how physically active you are.
Depending on the dosage you need, you may require more than one injection.
Insulin pump
In addition to being given as injections, Humalog U-100 can also be used in an insulin pump. If youre using Humalog in an insulin pump, your doctor will explain how and when to take the medication.
Intravenous injection
Humalog Mix
Humalog Mix contains a combination of fast- and intermediate-acting insulins.
Can Insulin Be Administered Im
IntramuscularIMinsulin
. Likewise, what happens if you give insulin IM?
Insulin should be injected into the fatty tissue just below your skin. If you inject the insulin deeper into your muscle, your body will absorb it too quickly, it might not last as long, and the injection is usually more painful. This can lead to low blood glucose levels.
Secondly, can insulin be administered intravenously? The only type of insulin that should be given intravenously is human regular insulin. There is no advantage to using rapid-acting analogs in preparing insulin infusions because the rate of absorption is no longer a factor when administering insulin intravenously and can only result in added costs to the institution.
Regarding this, what ways can insulin be administered?
There are different ways to inject insulin into your body this is called insulin delivery. Syringes, pens, pumps, and jet injectors give many persons with diabetes options for their insulin delivery. A syringe is a device with a hollow center, plunger, needle, and removable needle guard.
Why is insulin given as an injection?
To enter most cells, insulin is needed. Without insulin, glucose builds up in the bloodstream. When the body cannot make insulin or make enough insulin, it must be taken through injection. Therefore, when the body can’t make insulin, it can’t be taken in pill form and at this time must be injected.
Read Also: When Do Diabetics Need Insulin
Optimal Range Of Glucose Control
The results of the experience with intravenous insulin and tight glucose control led to a re-examination of the optimal range of glucose control. Although control of hyperglycemia did reduce infection rates, especially after cardiothoracic surgery, a net benefit was tempered by higher rates of hypoglycemia and mortality. The ideal target blood glucose level in the intensive care setting has yet to be established but seems to be less than 180 mg/dL .
The lowest acceptable threshold for serum glucose has not been established. However, given the increased risk of hypoglycemia associated with insulin protocols that sought to control blood glucose levels between 80 and 110 mg/dL, a goal of less than 110 mg/dL cannot be endorsed. This was also the sentiment of a consensus statement that suggested a glucose target of 140-180 mg/dL in critically ill patients however, certain subgroups, such as patients undergoing cardiothoracic surgery, may benefit from a lower target range. Therefore, a glucose target of 110-140 mg/dL may eventually be a more appropriate range for this subgroup and other critically ill patients however, this level of control has not been subjected to rigorous investigation and determined with evidence-based support.
Usual Adult Dose For Diabetes Type 1
Note: Regular human insulin is available in 2 concentrations: 100 units of insulin per mL and 500 units of insulin per mL Doses should be individualized based on patient’s metabolic needs, blood glucose monitoring results, and glycemic goals-Total daily insulin requirements are generally between 0.5 to 1 unit/kg/dayInsulin U-100 :SUBCUTANEOUS Administration: Inject subcutaneously approximately 30 minutes prior to a meal-Insulin U-100 should generally be used in a regimen with an intermediate or long-acting insulinINTRAVENOUS Administration: Administer only under medical supervision with close monitoring of blood glucose and serum potassium-Humulin R: Dilute to a concentration of 0.1 to 1 unit/mL in an infusion system using polyvinyl chloride infusion bags this insulin is stable in normal saline-Novolin R: Dilute to a concentration of 0.05 to 1 unit/mL in an infusion system using polypropylene infusion bags this insulin is stable in normal saline, 5% dextrose, or 10% dextrose with 40 mmol/L potassium chlorideInsulin U-500 : For subcutaneous administration only-Administer U-500 insulin subcutaneously 2 to 3 times a day approximately 30 minutes prior to start of a meal–The safety and efficacy in combination with other insulins has not been determined.
Don’t Miss: Diabetes Type 2 Hereditary
Hyperkalemia In Cardiac Arrest
Based on the principles of treatment and indications discussed above, our experts recommend the following approach to suspected hyperkalemia or confirmed hyperkalemia in cardiac arrest in addition to usual ACLS measures:
Push 1 amp calcium chloride in well running peripheral IV or central line and repeat until the QRS is < 100ms
Epinephrine 5-20 mcg q2-5 minutes
Sodium Bicarbonate 1 amp IV
Shift potassium with Insulin and Glucose followed by B-agonist
Dialysis
Rebound Hyperkalemia
In cases of cardiac arrest due to hyperkalemia, perform CPR until the hyperkalemia is corrected. This may be a much longer time than usual. When ROSC is achieved, it will be primarily due to the effects of calcium rather than decreased potassium levels. The effect of calcium can last 20-30min. Since the stabilizing effects of calcium will wear off, you must promptly work on shifting the potassium and enhancing its elimination as described above. Consider repeating the calcium bolus if there are any worsening ECG changes. Repeat serial potassium measurements to monitor for rebound hyperkalemia, which occurs more often than wed like.
PEARL: the patient in cardiac arrest with hyperkalemia should not be pronounced dead until their potassium level is normalized
Is Iv Insulin Therapy Different From Daily Insulin Injections
Intravenous insulin therapy is a treatment procedure to manage high blood sugar with intravenous infusion of insulin. Intravenous insulin is administered only in a hospital ICU setting in selected critically ill patients with a diabetes emergency or other conditions affecting blood sugar who require rapid and efficient control of hyperglycemia.
Self-administration of insulin by people with diabetes is always with an injection in the fatty tissue under the skin . Intravenous insulin therapy is performed only under medical supervision along with continuous monitoring of blood sugar levels and various other vital parameters.
Recommended Reading: What Is A Normal A1c For A Non Diabetic
Diabetes Responsive To Intravenous But Not Subcutaneous Insulin: Effectiveness Of Aprotinin
Abstract Patients with diabetes that is insensitive to subcutaneous insulin but sensitive to intravenous insulin have recently been described. We have studied this phenomenon in five female diabetics who required excessive amounts of insulin to avoid recurrent ketoacidosis. Known causes of insulin resistance were excluded. All patients had normal responses to conventional doses of intravenous insulin . Four patients required continuous intravenous infusion of insulin for one to six months. When a mixture of aprotinin and regular porcine insulin was given subcutaneously, conventional doses produced euglycemia plasma levels of free insulin rose, and ketonuria disappeared. Four patients had episodes of spontaneous, severe hypoglycemia before and during aprotinin therapy, necessitating continuous infusion of glucose for two to 14 days. Although no insulin was administered, hyperinsulinemia was present. These findings suggest excessive degradation or sequestration of insulin at the site of injection. Supported by the John W. Champion Center, Children’s Hospital, Columbus, Ohio by Clinical Research Center grants to University Hospital, Ohio State University and by a Clinical Research Center grant and a grant from the National Institutes of Health to Washington University and the Diabetic Children’s Welfare Association, St. Louis. From the divisions of Endocrinology and Metabolism, departments of Pediatrics and Medicine, Ohio State UniversiContinue reading > >
What Should I Do If My Humalog Insulin Isnt Working
If you think that Humalog isnt working well enough to manage your blood sugar, talk with your doctor. They may need to adjust your dosage. Or you may have to change the spot where you inject Humalog. For example, if youve been giving yourself injections into damaged areas of skin, Humalog may not work as well.
If your Humalog KwikPen isnt working, check the brochure that comes with the pen for instructions. Or ask your doctor or pharmacist for help. If the dose knob is hard to push, the needle may be blocked. So you can try using a new needle. Or there may be something inside the pen, such as dust or food. In this case, youd need to get a new pen.
You May Like: High Blood Sugar And Chills

