Regulation Of Insulin Action At The Cellular Level
Abstract Insulin regulates cellular metabolic reactions by its action on the plasma membrane, intracellular enzymes and the nucleus. The first stage in the propagation of the insulin signal is the coupling of insulin to specific receptors at the cell surface. The exact mechanism whereby the transmembrane signalling mechanism results in different insulin-mediated cellular effects is not known. However, the insulin receptor tyrosine kinase, the expression of second messengers, and the action of protein kinase C may, either individually or in combination, mediate some of the insulin effects, such as translocation and activation of glucose transporter proteins. Insulin resistance in clinical conditions such as insulin-dependent diabetes mellitus , non-insulin-dependent diabetes mellitus , hypertension and obesity may be acquired to a large extent, and is thus partially reversible. Regulatory factors in insulin sensitivity, such as free fatty acids, counterregulatory hormones and blood glucose level, play an important role in the metabolic control and pathogenesis of insulin resistance in man.Continue reading >>
Mechanisms Of Insulin Resistance
Physiologically, at the whole body level, the actions of insulin are influenced by the interplay of other hormones. Insulin, though the dominant hormone driving metabolic processes in the fed state, acts in concert with growth hormone and IGF-1; growth hormone is secreted in response to insulin, among other stimuli, preventing insulin-induced hypoglycaemia. Other counter-regulatory hormones include glucagon, glucocorticoids and catecholamines. These hormones drive metabolic processes in the fasting state. Glucagon promotes glycogenolysis, gluconeogenesis and ketogenesis. The ratio of insulin to glucagons determines the degree of phosphorylation or dephosphorylation of the relevant enzymes. Catecholamines promote lipolysis and glycogenolysis; glucocorticoids promote muscle catabolism, gluconeogenesis and lipolysis. Excess secretion of these hormones may contribute to insulin resistance in particular settings, but does not account for the vast majority of insulin resistant states.
Other Ligands For The Insulin Receptor
Insulin-like growth factors are so-called because they have significant structural homology with proinsulin but mainly mitogenic effects, significantly regulated by growth hormone. IGF-1 and 2 are coded for on the long arm of chromosome 12 and short arm of chromosome 11 respectively. They have specific receptors and bind with different affinities to the various IGF binding proteins. Insulin can bind to the receptors for IGF-1 and 2 but with much lower affinity respectively. IGF-1 binds weakly to the insulin receptor, with only 1.25×103 the affinity for the IGF-1 receptor; it binds the IGF-2 receptor with 1/4 the affinity for the IGF-2 receptor. IGF-2 does not bind to the insulin receptor; it does bind the IGF-1 receptor but with 1/3 the affinity for the IGF-2 receptor. Therefore overlap in physiological functions is more limited in vivo.
Read Also: Can Type 2 Diabetics Eat Bananas
Structural Analysis And Synthesis
Purified animal-sourced insulin was initially the only type of insulin available for experiments and diabetics. John Jacob Abel was the first to produce the crystallised form in 1926. Evidence of the protein nature was first given by Michael Somogyi, Edward A. Doisy, and Philip A. Shaffer in 1924. It was fully proven when Hans Jensen and Earl A. Evans Jr. isolated the amino acids phenylalanine and proline in 1935.
The amino acid structure of insulin was first characterized in 1951 by Frederick Sanger, and the first synthetic insulin was produced simultaneously in the labs of Panayotis Katsoyannis at the University of Pittsburgh and Helmut Zahn at RWTH Aachen University in the mid-1960s.Synthetic crystalline bovine insulin was achieved by Chinese researchers in 1965. The complete 3-dimensional structure of insulin was determined by X-ray crystallography in Dorothy Hodgkin‘s laboratory in 1969.
Two other Nobel Prizes have been awarded for work on insulin. British molecular biologist Frederick Sanger, who determined the primary structure of insulin in 1955, was awarded the 1958 Nobel Prize in Chemistry.Rosalyn Sussman Yalow received the 1977 Nobel Prize in Medicine for the development of the radioimmunoassay for insulin.
Where Does Insulin Come From When Used As Medication
When the pancreas cannot produce enough of its own insulin, it becomes necessary to get insulin from an external source. If you have diabetes, your doctor may decide to prescribe insulin injections for you.
Before the 1980s, the only way to source insulin was to take insulin from pigs or cows . Insulin extracted from these animals was purified before use in humans. However, with the advent of DNA technology in the 1980s, it is more common for patients to receive biosynthetic human insulin. The use of porcine or bovine insulin has become a lot less common .
We produce biosynthetic human insulin by utilising bacteria or yeast cells. Firstly, the human gene responsible for producing insulin is extracted. This is then inserted into the genetic material of bacteria or yeast cells. As these cells replicate and multiply, they produce insulin. In the end, the insulin they produce gets purified and is ready for medical use. Drug companies usually package insulin into cartridges, pens or vials for human use.
Recommended Reading: Can You Get Diabetes If You Re Skinny
How Should I Store My Insulin
- Keep current insulin at room temperature to help alleviate injection discomfort.
- Insulin can usually be stored at room temperature for about a month. Once in use, insulin pens should be stored at room temperature. Expiration dates of insulin pens can vary depending upon the type of insulin. For disposable pens, you should discard the entire device when empty or when you reach the expiration date.
- Store extra insulin in the refrigerator.
- Dont expose insulin to excessive cold or heat.
Sleep And Sleep Deprivation
Acute sleep deprivation in healthy young adults has been reported to raise fasting blood glucose concentrations in association with altered diurnal cortisol secretion and reduced heart rate variability. These effects suggest increased counter-regulatory hormone secretion via hyper-arousal with activation of the hypothalamo-pituitary adrenal axis. There is also accumulating evidence that chronic sleep deprivation may impact on insulin and insulin resistance. Recent epidemiological studies report that reduced sleep duration is associated with increased BMI. Sleep deprivation is associated with decreased plasma concentrations of leptin, the adipocyte peptide hormone regulating fat mass and appetite, and increased concentrations of ghrelin, which increases appetite. Growth hormone is secreted during slow wave sleep, sleep declines with age and growth hormone deficiency in adults has been associated with central adiposity and insulin resistance, but whether sleep deprivation acts through these mechanisms is not clearly established. Obstructive sleep apnoea , where sleep disturbance results from obstruction to breathing during sleep, is associated with impaired glucose tolerance independent of adiposity, and improves with continuous positive airway pressure treatment but whether this is due to resolution of hypoxia and hypercapnia, or to effects on sleep quality, is unclear.
Don’t Miss: Which Of The Following Is Most Closely Related To Diabetes
Who Needs To Take Insulin
Diabetes impairs insulin production by the pancreas and use of this essential hormone by the body. The condition causes high blood sugar levels.
However, not every person with type 2 diabetes will need to take insulin. People with type 1, on the other hand, will have to supplement their insulin supply for the rest of their lives.
There are three main types of diabetes:
- Type 1 diabetes: Typically starts in childhood when a person does not produce enough insulin. Usually results from the bodys immune system attacking an otherwise healthy pancreas.
- Type 2 diabetes: Can develop at any age but 45 years is the average age of onset. Either the pancreas does not produce enough insulin, or the bodys cells become resistant to its actions.
- Gestational diabetes: Occurs during pregnancy and makes it harder for a womans body to respond to insulin. Typically stops after childbirth but increases a womans risk of developing type 2 diabetes.
Type 1 and type 2 diabetes are usually lifelong conditions. According to the Centers for Disease Control and Prevention , more than 30 million people in the United States have diabetes. Type 2 diabetes is the most common, accounting for
The Basics Of High Blood Sugar
Diabetes is a problem with your body that causes;blood;sugar ;levels to rise higher than normal. This is also called;hyperglycemia.
When you eat, your body breaks food down into sugar;and sends it into the blood. Insulin then helps move the sugar from the blood into your cells. When;sugar enters your cells, it is either used as fuel for energy right away or stored for later use. In a person with diabetes, there is a problem with;insulin. But, not everyone with diabetes has the same problem.;
There are different types of diabetestype 1, type 2;and gestational diabetes. If you have diabetestype 1, type 2;or gestationalyour body either doesn’t make enough insulin, can’t use the insulin well, or both.
Learn more about blood sugar; ; ;Learn more about insulin
Recommended Reading: How To Lose Weight On Insulin
Do You Have Insulin Resistance
How do you find out if youre insulin resistant? No one test will tell you, but if you have high blood sugar levels, high triglycerides , high LDL cholesterol, and low HDL cholesterol, your health care provider may determine you have insulin resistance.
Important note: Type 1 diabetes is different; its thought to be caused by an autoimmune reaction . People with type 1 diabetes dont make enough insulin and need to take it to survive.
Synthesis And Release Of Insulin
Insulin is coded on the short arm of chromosome 11 and synthesised in the cells of the pancreatic islets of Langherhans as its precursor, proinsulin. Proinsulin is synthesised in the ribosomes of the rough endoplasmic reticulum from mRNA as pre-proinsulin. Pre-proinsulin is formed by sequential synthesis of a signal peptide, the B chain, the connecting peptide and then the A chain comprising a single chain of 100 amino acids. Removal of the signal peptide forms proinsulin, which acquires its characteristic 3 dimensional structure in the endoplasmic reticulum. Secretory vesicles transfer proinsulin from the RER to the Golgi apparatus, whose aqueous zinc and calcium rich environment favours formation of soluble zinc-containing proinsulin hexamers. As immature storage vesicles form from the Golgi, enzymes acting outside the Golgi convert proinsulin to insulin and C-peptide. Insulin forms zinc-containing hexamers which are insoluble, precipitating as chemically stable crystals at pH 5.5. When mature granules are secreted into the circulation by exocytosis, insulin, and an equimolar ratio of C-peptide are released. Proinsulin and zinc typically comprise no more than 6% of the islet cell secretion.
Read Also: Is Ginger Ale Good For Diabetics
Factors Influencing Insulin Biosynthesis And Release
Insulin secretion may be influenced by alterations in synthesis at the level of gene transcription, translation, and post-translational modification in the Golgi as well as by factors influencing insulin release from secretory granules. Longer-term modification may occur via influences on cell mass and differentiation. Given insulins pivotal role in glucose utilisation and metabolism, it is not surprising that glucose has multiple influences on insulin biosynthesis and secretion. However, other factors such as amino acids, fatty acids, acetylcholine, pituitary adenylate cyclase-activating polypeptide , glucose-dependent insulinotropic polypeptide , glucagon-like peptide-1 , and several other agonists, together in combination, also influence these processes.
How Is Type 2 Diabetes Diagnosed
Doctors can say for sure if a person has diabetes by testing blood samples for glucose. Even if someone doesn’t have any symptoms of type 2 diabetes, doctors may order blood tests to check for it if the person has certain risk factors .
Some kids and teens with diabetes may go to a pediatric endocrinologist â a doctor who specializes in diagnosing and treating children and teens living with diseases of the endocrine system, such as diabetes and growth problems.
p
Don’t Miss: Qu? Fruta No Puede Comer Un Diabetico
What Is Type 2 Diabetes
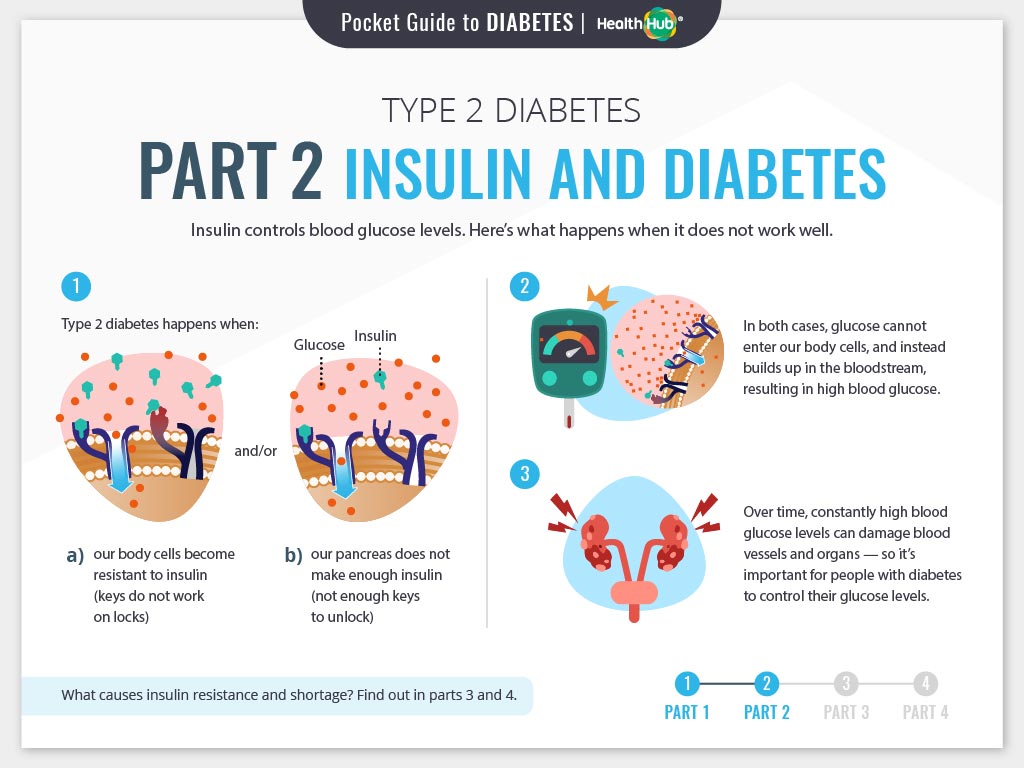
There are two major types of diabetes: type 1 and type 2. Each type causes high blood sugar levels in a different way.
In type 1 diabetes, the pancreas can’t make insulin. The body can still get glucose from food, but the glucose can’t get into the cells, where it’s needed, and glucose stays in the blood. This makes the blood sugar level very high.
With type 2 diabetes, the body still makes insulin. But a person with type 2 diabetes doesn’t respond normally to the insulin the body makes. So glucose is less able to enter the cells and do its job of supplying energy.
When glucose can’t enter the cells in this way, doctors call it insulin resistance. Although there’s plenty of insulin in the person’s body, because it doesn’t work properly, the pancreas still detects high blood sugar levels. This makes the pancreas produce even more insulin.
The pancreas may eventually wear out from working overtime to produce extra insulin. When this happens, it may no longer be able to produce enough insulin to keep blood sugar levels where they should be. In general, when someone’s blood sugar levels are repeatedly high, it’s a sign that he or she has diabetes.
p
Exercise & Physical Activity
Since Chauveu & Kaufmans remarkable observation in 1887 that When a horse chews on hay the concentration of glucose in the blood draining its masseter muscle substantially decreases a large body of evidence supports the role of exercise in improving insulin sensitivity and its beneficial outcomes in insulin resistant states. Epidemiological studies such as the US Physicians Health Study have reported substantial decreases in the relative risk of type 2 diabetes with lifelong regular physical activity. Large scale randomised controlled clinical trials such as the Diabetes Prevention Program and the Finnish Prevention Study demonstrate a 58% reduction in progression of impaired glucose tolerance to type 2 diabetes by intensive lifestyle modification which included a minimum of 2030 minutes of exercise per day. Acute exercise increases GLUT 4 translocation to sarcolemmal membrane, whereas chronic exercise training increases Glut 4 mRNA expression. In addition to this insulin-dependent mechanism, enhanced glucose uptake into exercising muscle occurs by multiple insulinin dependent mechanisms. Exercise training appears to enhance insulin sensitivity by increased post-receptor insulin signalling; increased insulin-mediated glucose transport appears to be related to enhanced signal transduction at the level of IRS proteins and PI 3-kinase.
You May Like: When Viagra Doesn T Work Diabetes
When The Blood Glucose Level Goes Up
- Blood sugar rises;
- The pancreas detects the rise;
- The pancreas pumps out insulin into the blood;
- Insulin helps the uptake of glucose into muscles and other cells;
- This causes the blood glucose level to fall to its normal set point; and
- The pancreas detects the fall and switches off insulin production.
Myths About Insulin Therapy
According to the American Diabetes Association , several common myths surround the use of insulin therapy for people with type 2 diabetes.
People who take insulin may sometimes hear others make the following statements, but they have no basis in research or fact:
- Insulin can cure diabetes. There is, at present, no cure for diabetes. However, insulin can help a person control its effects.
- It will cause disruption in your life. While a course of insulin takes some getting used to, a person can enjoy a full and active life, as long as they stick to their insulin schedule.
- Insulin injections cause pain. Many people have a phobia of needles. However, modern insulin pens cause almost no pain. People using pumps can avoid injections altogether.
- Insulin will increase the frequency of severe hypoglycemia. While insulin can increase the risk of hypoglycemia, certain insulins can limit a sudden drop in blood sugar.
- Insulin causes weight gain for as long as a person uses it. Insulin might increase weight at first, but this is not an ongoing effect. The body first needs to adapt to insulin supplementation.
- The injection site is not important. Where on the body a person inserts a needle or pen determines the speed at which insulin has an effect. This can be vital after meals when quick drops in blood glucose levels reduce the impact of the food.
- Insulin is addictive. Insulin is not an addictive drug and is vital for any person whose pancreas does not produce insulin.
Also Check: Do You Need Insulin For Type 2 Diabetes
Produced In The Pancreas
When you eat, food travels to your stomach and small intestines, where its broken down into nutrients that include glucose. The nutrients are absorbed and distributed via your bloodstream.
The pancreas is a gland located behind your stomach that performs an essential role in the digestion process. It creates enzymes that break down the fat, starches, and sugar in the food. It also secretes insulin and other hormones into your bloodstream.
Insulin is created in the beta cells of the pancreas. Beta cells comprise about 75% of pancreatic hormone cells.
Other hormones produced by the pancreas are:
- glucagon, which alerts your liver to raise your blood sugar if it gets too low
- gastrin, which stimulates the production of gastric acid in your stomach
- amylin, which helps control your appetite
Common Conditions Associated With Insulin Resistance
Type 2 Diabetes
Following pioneering work by Bornstein and the Nobel Prize-winning work of Yalow and Berson, the first insulin assays became widely available in the late 1960s; it was subsequently confirmed that diabetic patients with so-called or maturity onset or type 2 diabetes had normal or increased plasma insulin levels. Insulin resistance was reported to be a characteristic feature of T2DM in the early 1970s. A progressive inability of the cells to compensate for the prevailing insulin resistance by sufficient hyperinsulinaemia, heralds the clinical onset of this disorder. While twin studies and linkage analyses are consistent with a strong genetic component in the development of type 2 diabetes, several decades of research have failed to identify a predominant genetic abnormality in the majority of cases. The aetiology of T2DM is thought to be polygenic, with environmental factors being superimposed upon this basic predisposition.
Insulin resistance typically predates the development of diabetes and is commonly found in unaffected first-degree relatives. The morbidity of the disorder relates both to the severity of hyperglycaemia and the metabolic consequences of insulin resistance itself. The primary defects in insulin action appear to be in muscle cells and adipocytes, with impaired GLUT 4 translocation resulting in impaired insulin-mediated glucose transport.
Metabolic Syndrome
-
Abdominal obesity
Men <40 mg/dL
Women <50 mg/dL
Dyslipidaemia
Hypertension
PCOS
OSA
You May Like: Can Diabetics Eat Domino’s Pizza

