Selecting An Insulin Infusion Protocol
Numerous insulin infusion protocols have been published. However, head-to-head comparisons are rare, and efficacy and safety are difficult to determine because of differing patient populations, glycemic targets, metrics for evaluation, and definitions of hypoglycemia used in the various protocols., Selecting a validated protocol allows for more rapid implementation but does not eliminate the need for ongoing safety and effectiveness monitoring and continuous quality improvement.
Some paper protocols are table-based, whereas others require mathematical calculations. The level of clinical judgment and physician oversight also varies among the available protocols. Computerized protocols allow for more complex mathematical calculations and can provide alerts or alarms to remind staff members to check patients blood glucose level and adjust infusion rates.
Several studies comparing computerized and paper-based protocols have found improved protocol adherence, improved glycemic control, and less hypoglycemia with computerized protocols. It is worth noting that evaluations of computerized glucose control programs have used glycemic targets that are tighter than currently recommended, and although the percentages of blood glucose readings within the target range were higher than with paper protocols, they still were not optimal in most studies. It is not clear how computerized glucose control programs compare to paper-based protocols when currently recommended targets are used.
Ask The Diabetes Team
Question: From a nurse in Michigan, USA: Can insulin be given IV push ? I am a new nurse and this was a sliding scale order for one of my patients. The patient’s blood sugar level was 234 and the sliding scale order was to give 2 units of R insulin IV push and 8 units R subcutaneously. The patient was 54 years old. My nursing drug book stated not to give concentrated insulin IV. Is this something new that physicians are beginning to prescribe? Answer: Regular insulin can be given as an IV push undiluted. The only reason to dilute it is to facilitate low dose continuous infusion if this is what is needed. DTQ-19991105013815 Original posting 11 Jan 2000 Posted to Insulin This Internet site provides information of a general nature and is designed for educational purposes only. If you have any concerns about your own health or the health of your child, you should always consult with a physician or other health care professional. This site is published by T-1 Today, Inc. , a 501c3 not-for-profit organization, which is responsible for its contents. Our mission is to provide education and support to families living with type 1 diabetes. By using this site, you agree to our Terms of Use, Legal Notice, and Privacy Policy. © Children with Diabetes, Inc. 1995-2017. Comments and Feedback.Continue reading > >
Is It Possible To Eat While On An Insulin Drip
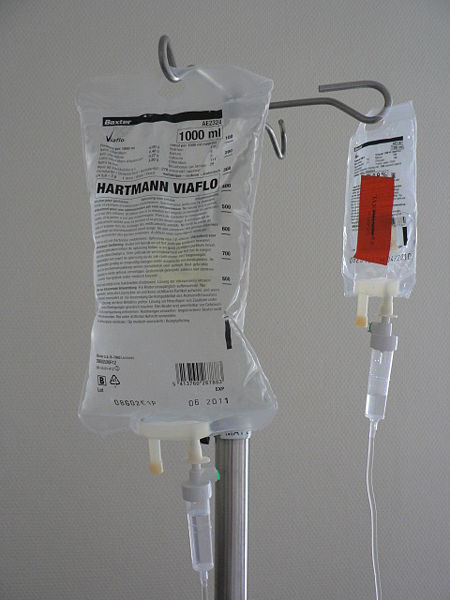
Insulin drips are usually prescribed for DKA patients until the anion gap closes and the blood glucose levels normalize. Many patients are kept NPO until this happens, however if the gap closure procedure takes a long time, some patients may be permitted to consume tiny meals. Patients have a high level of insulin resistance.
Also Check: Can I Get A Tattoo If I Have Diabetes
The 3 Routes Of Administration For Insulin
Insulin is only available as a liquid preparation.
Depending on different circumstances it can:
- be injected subcutaneously via an insulin syringe, pre-filled pen device or insulin pen
- for certain patients with type 1 diabetes, be delivered as an insulin infusion via a wearable personal insulin pump
- be administered through an intravenous insulin infusion
Is It Necessary To Shake Nph Insulin

A: In the vial, some forms of insulin, such as NPH, Lente, and Ultralente insulin, appear murky. Rolling the insulin between your palms is a smart approach to combine insulin in a vial without creating a lot of little bubbles. They will not harm you if you shake the insulin and mix in a lot of bubbles.
Recommended Reading: Metformin Vision Side Effects
How Should This Medicine Be Used
Human insulin comes as a solution and a suspension . to be injected subcutaneously . Human insulin is usually injected subcutaneously several times a day, and more than one type of insulin may be needed. Your doctor will tell you which type of insulin to use, how much insulin to use, and how often to inject insulin. Follow these directions carefully. Do not use more or less insulin or use it more often than prescribed by your doctor.
Human insulin solution may also be injected intravenously by a doctor or nurse in a healthcare setting. A doctor or nurse will carefully monitor you for side effects.
Human insulin controls high blood sugar but does not cure diabetes. Continue to use human insulin even if you feel well. Do not stop using insulin without talking to your doctor. Do not switch to another brand or type of insulin or change the dose of any type of insulin you use without talking to your doctor.
Human insulin comes in vials, prefilled disposable dosing devices, and cartridges. The cartridges are designed to be placed in dosing pens. Be sure you know what type of container your insulin comes in and what other supplies, such as needles, syringes, or pens, you will need to inject your medication. Make sure that the name and letter on your insulin are exactly what your doctor prescribed.
If your human insulin comes in a disposable dosing device, read the instructions that come with the device carefully. Ask your doctor or pharmacist to show you how to use the device.
What Other Information Should I Know
Keep all appointments with your doctor and the laboratory. Your blood sugar and glycosylated hemoglobin should be checked regularly to determine your response to human insulin. Your doctor will also tell you how to check your response to human insulin by measuring your blood or urine sugar levels at home. Follow these directions carefully.
You should always wear a diabetic identification bracelet to be sure you get proper treatment in an emergency.
Do not let anyone else use your medication. Ask your pharmacist any questions you have about refilling your prescription.
It is important for you to keep a written list of all of the prescription and nonprescription medicines you are taking, as well as any products such as vitamins, minerals, or other dietary supplements. You should bring this list with you each time you visit a doctor or if you are admitted to a hospital. It is also important information to carry with you in case of emergencies.
You May Like: Metformin Dosage For Ketosis
Barriers To Implementing A Continuous Insulin Infusion Protocol
Potential barriers to implementing an insulin infusion protocol include fear of hypoglycemia, confusion regarding appropriate glycemic targets, insufficient nurse-to-patient ratios, insufficient availability or convenience of glucose-monitoring devices, lack of administrative support, various system and procedural issues, and resistance to change. Before implementing an IV insulin infusion protocol, it is imperative to evaluate the current glycemic-related practices within the institution and address the following crucial questions: What is the current level of glycemic control? Who is checking patients blood glucose and how often? How interested is the staff in optimizing glycemic control, and do they have the support they need to achieve this goal?
Key steps to overcoming these barriers include building support with multidisciplinary champions, involving key staff members in the process, educating staff and administrators about the benefits of optimizing glycemic control, and internally marketing the clinical success of the protocol. Descriptions of several models of implementation have been published, including endocrinologist consultation models, glycemic control teams, and system-wide models. It is important to adapt whichever model is selected to meet the needs of the specific institution.
Components Of Artificial Pancreas Systems
CGM, CSII, and control algorithms constitute the backbone technologies of current systems of closed-loop control of glucose concentration in type 1 diabetes or, the so-called artificial pancreas systems, being meticulously combined to emulate the feedback glucose-responsive functionality of beta-cells in normal physiology of glucose metabolism . Fig. 9.1 illustrates the main components of an AP system. Interstitial glucose concentration measurements are the main input of the controller which, depending on the underlying algorithm, determines the insulin delivery rate such that euglycemia is safely achieved and maintained. Additional bio- and physiological signals , predictive or reflective of glycemia as well as patients physiological, emotional, and behavioral status, may be exploited in order to adjust the operating mode of the controller .
Figure 9.1. Components of closed-loop controller of glucose in type 1 diabetes based on the double subcutaneous route .
Also Check: Long Term Side Effects Of Metformin
Should Cii Be Restricted To The Icu
IV insulin infusion protocols have generally been reserved for the intensive-care setting. Studies to support use of CII have primarily been limited to ICUs. However, patients who could benefit from insulin infusion therapy are not restricted to the intensive-care setting. The use of IV insulin protocols has been widely accepted in the treatment of patients presenting with hyperglycemic hyperosmolar state and diabetic ketoacidosis without a requisite admission to the ICU. Events leading to prolonged hyperglycemia or significant fluctuations in blood glucose levels should not require admission to the ICU for appropriate treatment. Conversely, patients in the ICU who are now clinically stable should not have transfer to a step-down unit or regular medical floor delayed secondary to hospital restrictions regarding IV insulin.
In 2005, a group from Duke University published results of a project evaluating the safety, effectiveness, and feasibility of using an IV insulin algorithm in the general hospital wards. Audit findings indicated that the nomogram for monitoring IV insulin infusion could be used effectively on intermediate-care general medicine units with a nurse-to-patient ratio as high as 1:6.
Implementation: Piloting The Protocol
Piloting is necessary to ensure that the general concepts and details of the protocol are understood and feasible. After extensive educational programs designed to inform and empower staff, the team must decide on a roadmap for implementation.
A stepped approach is one method often used because it allows staff to better acclimate to changes in practice and familiarize themselves with the fundamentals of the protocol. The protocol is initially tested in only one ICU, and possibly only one patient, at a time. Often, based on the amount of supporting literature, the cardiovascular or surgical ICU becomes the chosen unit for initiation. The team must come to agreement with the staff on an acceptable glucose level for initiation and a target glucose range. It is recommended to start with higher target ranges that can be fine-tuned over time to the ultimate goal blood glucose range as the comfort level of the staff increases. Working with nurse management to assure staffing appropriate to the additional time constraints should also be a consideration. Under the guidance and oversight of the glycemic management team, staff can implement the details of the protocol. Through repetition, support, and ongoing communication, staff will increase their familiarity with execution of tight glycemic control protocols and build efficiency in performance. Over time,these new behaviors will become the default rather than the exception.
You May Like: Glucophage Side Effects
In A Person With Type 1 Diabetes Or Type 2 Diabetes
In a person with type 1 diabetes: the pancreas constantly tries to produce beta cells in order to make insulin, but the immune system continues to attack and destroy most or all of those beta cells.
For those with type 1 diabetes, the evolution of the disease and the attack on the beta cells occurs very quickly, which means people get sick very quickly. Often mistaken at first for the lingering flu, a simple blood test and urine test can determine and diagnose type 1 diabetes.
Immediately upon diagnosis, patients should begin taking pharmaceutical insulin via pump, pen, or syringe.
In a person with type 2 diabetes: the body is either struggling to produce a normal amount of insulin , or the body is struggling with severe insulin resistance which makes it difficult to manage healthy blood sugar levels with the available amount of insulin.
For those with type 2, the struggle to properly produce or make use of their own insulin is usually a slower process, sometimes taking years before you show strong enough symptoms to warrant an HbA1c test,a diagnosis, and eventual treatment.
Why Is This Medication Prescribed
Human insulin is used to control blood sugar in people who have type 1 diabetes or in people who have type 2 diabetes that cannot be controlled with oral medications alone. Human insulin is in a class of medications called hormones. Human insulin is used to take the place of insulin that is normally produced by the body. It works by helping move sugar from the blood into other body tissues where it is used for energy. It also stops the liver from producing more sugar. All of the types of insulin that are available work in this way. The types of insulin differ only in how quickly they begin to work and how long they continue to control blood sugar.
Over time, people who have diabetes and high blood sugar can develop serious or life-threatening complications, including heart disease, stroke, kidney problems, nerve damage, and eye problems. Using medication, making lifestyle changes , and regularly checking your blood sugar may help to manage your diabetes and improve your health. This therapy may also decrease your chances of having a heart attack, stroke, or other diabetes-related complications such as kidney failure, nerve damage , eye problems, including changes or loss of vision, or gum disease. Your doctor and other healthcare providers will talk to you about the best way to manage your diabetes.
You May Like: Regular Insulin Side Effects
Table 78 Preparation Questions For Intravenous Medications
Safety considerations:
- Be diligent and follow all policies related to medication calculations, preparation, and thorough assessment of patient status before and after an injection. Medication errors are the most common preventable errors in health care.
- Use a blunt filter needle or blunt needle when preparing injections. Never use a needle when injecting IV medication. Always use a needleless system.
- After preparing the medication, always label the medication syringe with two patient identifiers, date, time, medication, dose, and your initials. Never leave the syringe unattended.
- Correctly identify the VAD, and use agency flushing and locking protocols for correct administration.
- Always administer the post-saline lock flush at the SAME RATE as the IV medication.
- Always assess the patients symptoms and need for IV medication prior to administration.
- Always assess the patients understanding of the medication.
Principle
How and where do you chart this medication: pain assessment sheet, MAR, etc.? Data source: BCIT, 2015 Berman & Snyder, 2016 Clayton et al., 2010 WHO, 2012
Before giving an intravenous medication, always assess the IV insertion site for patency and for signs of infiltration or phlebitis. Start a new IV site if current site is red, swollen, or painful when flushing. Intravenous medications by direct IV route can be given three ways:
Checklist : Administering Medications Iv Direct Into An Infusing Iv With Compatible Solution
Disclaimer: Always review and follow your agency policy regarding this specific skill.
Safety considerations:
- Review the advantages and disadvantages of IV medications
- Be able to answer the preparation questions for intravenous medication in Table 7.9 before administering the medication.
- If the medication has been diluted and there is wastage, always discard unused diluted portion of the prepared IV medication before going to the bedside.
- Always follow agency policies and guidelines when preparing and administering medications
- Always label the syringe with 2 patient identifiers, date, time, medication, concentration of the dose, dose, and your initials. Once the medication is prepared, never leave it unattended.
- NEVER administer an IV medication through an IV line that is infusing blood, blood products, heparin IV, insulin IV, cytotoxic medications, or parenteral nutrition solutions.
- Never administer an IV medication into an IV line that isnt patent.
- Check compatibilities of the medication to with other medications / solutions in the same line
- Central venous catheters may require special pre- and post-flushing procedures and specialized training.
- CVCs require at minimum a 10 ml syringe to decrease risk of catheter fracture.
- You will need a clock / timer/ watch to time the rate of administration.
- Perform hand hygiene before preparing medications.
Steps
Additional Information
2. Create privacy if possible. This provides comfort to patient.
Don’t Miss: Are Pork Rinds Good For Diabetics
Pitfalls In Bedside Glucose Measurement
Accurate serum glucose levels are crucial to the successful implementation of any intravenous insulin protocol. Timely and accurate glucose measurements guide the dosing of insulin and affect decisions about implementation, adjustment, and discontinuation. Hypoglycemia is the most feared adverse effect of intravenous insulin therapy, not only for its impact on neurologic function but also because of the association of hypoglycemia with increased mortality. Moreover, the warning signs of hypoglycemia are often difficult to appreciate in the critically ill patient.
The need for rapid testing in critically ill patients has spawned multiple bedside, point-of-care devices, and none is more pervasive in the ICU than the bedside glucometer. Accuracy is reduced, with standards requiring only an agreement of ±20% with laboratory analysis. The glucometers are most accurate in hemodynamically stable patients with glucose readings in the normal range, but disagreements with laboratory readings are more pronounced with glucose readings at the high and low ends of the spectrum and in conditions of poor tissue perfusion .
Factors that affect point-of-care blood glucose measurements include the following :
-
Sampling site
-
Amount of blood on glucometer strip
-
Excess blood
-
Insufficient blood
Anemia
Peripheral hypoperfusion
Delay in sample processing
Substances that interfere with glucose measurements:
Levodopa
Maltose
Icodextrin
Cii Versus Sliding Scale
In critically ill patients, insulin is necessary to achieve a reduction in blood glucose levels. Using intravenous insulin in the absence of glucose lowering will have no effect on outcomes. The Diabetes and Insulin-Glucose Infusion in Acute Myocardial Infarction study demonstrated that, in patients suffering an acute myocardial infarction regardless of a history of diabetes, IV insulin therapy for 24 hours followed by intensive subcutaneous therapy for 3 months improved long-term survival. The follow-up DIGAMI 2 study was designed to evaluate the relative benefit of long-term tight glycemic management. Although the investigators failed to demonstrate significant differences in glucose control and mortality among the three treatment arms,they did illustrate the association between higher glucose levels and increased risk of death. Thus, merely administering insulin without lowering glucose levels will not improve outcomes.
CII is the only delivery method specifically developed for inpatient use and is preferred over the subcutaneous route for several clinical indications. The only type of insulin that should be given intravenously is human regular insulin. There is no advantage to using rapid-acting analogs in preparing insulin infusions because the rate of absorption is no longer a factor when administering insulin intravenously and can only result in added costs to the institution.
Table 2.
You May Like: How Many Points Does Metformin Lower Blood Sugar

