Disposal Of Used Insulin Syringes
Used syringes, pen needles, cannulas and lancets must be disposed of in an Australian Standards-approved sharps container, which is puncture-proof and has a secure lid. These containers are usually yellow and are available through pharmacies, local municipal councils and state or territory diabetes organisations such as Diabetes Victoria.;Procedures to dispose of sharps containers vary from state to state.For sharps disposal information and help, you can contact:
- state or territory diabetes organisations, such as Diabetes Victoria
- state department of health
Insulin needs to be stored correctly. This includes:
- storing unopened insulin on its side in a fridge
- keeping the fridge temperature between 2 and 8°C
- making sure that insulin does not freeze
- once opened, keeping it at room temperature for not more than one month and then disposing of it safely
- avoiding keeping insulin in direct sunlight.
Extreme temperatures can damage insulin so it doesn’t work properly. It must not be left where temperatures are over 30 °C. In summer your car can get this hot so don’t leave your insulin there.
There are various insulated insulin carry bags available for transporting insulin.
Other Considerations When Choosing Csii Or Mdi In Type 1 Diabetes
The relative disadvantages of CSII compared with injection treatment include the extra cost of pump and supplies and trained personnel needed to supervise the therapy, although recent cost-benefit analyses have concluded that CSII is fully cost-effective when the improved quality of control and its likely effect on reducing the risk of tissue complications are taken into account . Although the frequency of diabetic ketoacidosis is no higher during CSII than injection therapy , patients treated by insulin pumps are at potential risk of more rapid development of ketoacidosis than with injection therapy where there is a subcutaneous reservoir of insulin from the long-acting formulation. It should be noted that many patients may not meet the requirements for compliance and ability to manage the procedures of CSII or may just prefer to use MDI as their form of optimized therapy.
It must be underlined again that CSII is not needed in those type 1 diabetic patients who are well controlled and do not have problems of hypoglycemia on MDI, whether using long-acting analogs or not. There may be several other reasons for preferring MDI over CSII, including local resources, expertise, and patient preference .
Yes Insulin Does Expire Here’s How Long It Takes And When You Should No Longer Use It
- Insulin expires over time because its proteins break down and it becomes less effective at regulating blood sugars.;
- Unopened insulin generally expires after one year, but once you open your insulin, it takes about 28 days to expire.;
- It’s also important to store insulin properly, as it can expire early, so make sure to keep it refrigerated and away from light or heat.;
- This article was reviewed by;Jason R. McKnight, MD, MS, a family medicine physician and clinical assistant professor at;Texas A&M College of Medicine.;
- This story is part of Insider’s guide to;Diabetes.;
Insulin is a hormone that is produced in the pancreas, and helps signal the body to break down blood sugar for energy. In healthy individuals, the body produces all the insulin that it needs. However, people with diabetes either don’t produce insulin or are unable to use insulin effectively .;
As a result, about 24% of people with diabetes need to take insulin. However, this important medication can degrade over time, so it’s important to know when it expires and how to store it properly.;
Don’t Miss: What Is A Normal A1c For A Non Diabetic
Factors That Speed Insulin Absorption
Variation in insulin absorption can cause changes in blood glucose levels. Insulin absorption is increased by:
- injecting into an exercised area such as the thighs or arms
- high temperatures due to a hot shower, bath, hot water bottle, spa or sauna
- massaging the area around the injection site
- injecting into muscle this causes the insulin to be absorbed more quickly and could cause blood glucose levels to drop too low.
How Does It Work
Type 1 Diabetes, formerly known as Juvenile Onset Diabetes, is an autoimmune disorder that often develops at younger ages, however can occur at adulthood as well. ;It is believed that the immune system of the Type 1 Diabetic attacks the cells in the Pancreas called Beta Cells, which are responsible for producing insulin. Insulin is a hormone that helps regulate levels of blood sugar in the bloodstream. Symptoms of Type 1 Diabetes can include excessive hunger, thirst and urination, weight loss, blurred vision and tingling in the hands and feet. For people who do not have Diabetes, insulin is produced at a normal, constant levels on a consistent basis, with surges of extra insulin released after meals are ingested. Without the Beta Cells in the Pancreas producing insulin, there is no way for the blood glucose to be controlled in a Type 1 Diabetic without proper medical intervention. Uncontrolled Blood Glucose levels can be life-threatening and need to be managed as quickly as possible by a physician.
1515 North Flagler Drive; ; Suite 440; ; West Palm Beach, FL 33401
© Metabolic Research Institute, Inc. 2016-2017; All Rights Reserved.; Website Design & Manager:; VKA
Don’t Miss: How Long Does It Take Metformin To Lower A1c
Yes Insulin Does Expire
Medical insulin breaks down over time, which is why all insulin has an expiration date, says Maria Fernandez de Fiore, RN, a diabetes care and education specialist and Inpatient Diabetes Program Coordinator for Riverside University Health System in Moreno Valley, California.;
“The expiration date means that the insulin will start to degrade after this date,” Fernandez de Fiore says. “It will go bad because it won’t be effective to manage blood glucose levels anymore.”
Specifically, this is because insulin proteins break down over time. Expired insulin won’t make you sick, but it will be less effective, and it can be dangerous to use.;
“When it comes to insulin, we have to make sure it works at its full potency, or the blood glucose levels can go dangerously high,” Fernandez de Fiore says.;
How Is Insulin Injection Given
Insulin injections are usually administered by the patients, themselves, their caregivers or a parent/guardian in the case of a child. Insulin injections are subcutaneous, administered in the fat tissue beneath the skin. The sites for the injection, which should regularly rotate, may be:
- Front or side of the thigh
- Abdomen
- Outer side of the upper arm
- Upper outer quadrant of the buttocks
The important points of care for the patients during self-administration of insulin injections include the following:
- Washing hands before injection
- Correct time, dose and technique to administer the injection
- Dealing with possible steep drop in blood sugar with insulin
Injection technique
- Roll the insulin bottle several times between the palms .
- Remove the lid and wipe the bottleâs rubber top with an alcohol swab.
- Pull air into the syringe by pulling back the plunger up to the line showing the required dose.
- Push the needle through the bottleâs rubber top and push in the air.
- Turn the bottle and syringe upside down and draw in the required dose using the plunger
- Pinch up some skin in the chosen area and insert the needle.
- Push the plunger till the syringe is empty and hold in place for five seconds.
- Let go of the pinched skin and withdraw the needle.
- Press the insertion point for a few seconds if there is blood or insulin oozing out, but do not rub the area.
Prefilled pens
Mixing two insulins
Read Also: How Many Points Does Metformin Lower Blood Sugar
Comparing And Contrasting Long
If your doctor has told you that you needlong-acting insulin, you may be overwhelmed with the number of productsavailable. Although many brand name long-acting insulins are advertised on TVand in print, they represent only three main insulin products. The three mainlong-acting insulins that are available in the United States are insulinglargine , insulin degludec andinsulin detemir .
In this article, we will explore thesimilarities and differences between the long-acting insulins to help give youa better idea of what to expect.
How Soon After Taking Levemir Will My Symptoms Improve
Many different factors affect the levels of glucose in a persons blood. Physical activity, diet, stress, illness, time of dosing, the amount of dosing, and even the temperature can all have an effect on blood sugar. Following your doctor’s instructions regarding diet, dosing, and other lifestyle factors will help Levemir work best. Take this medication each day at the same time of the day as directed by your doctor. Levemir begins to work within a few hours of injection and stays in the system for about 24 hours.Continue reading >>
Also Check: Blood Sugar Rises During Sleep
When To Consider Adjusting Your Background Insulin
When Regular is injected or bolused, it takes 30 minutes to begin working, peaks between 2 and 4 hours and hangs on for 6 to 8 hours. However, most meals raise the blood sugar for only 2 to 3 hours after they are eaten. So when Regular is taken 30 minutes before a meal, it works for several hours after the meal, meaning it actually works as a long-acting insulin.
Humalog, on the other hand, begins working in 10 minutes, peaks at 1 to 2 hours, and is gone in about 3 and 1/2 hours. Because it more closely matches the action time of most meals, Humalog is lowering the blood sugar at the same time the food is raising it.
Because Humalog has a shorter action time, this may allow blood sugars to rise between meals as the insulin level drops before the next Humalog dose is taken. To compensate for this, doses of long-acting insulin may need to be increased when Humalog is started and less Humalog may be needed for meals than Regular.
One current trend is to use smaller, more frequent doses of long-acting insulin to provide a more stable level of background insulin throughout the day. If you are having difficulty maintaining control on Humalog, consider adjusting the long-acting insulin.
Frequent highs or lows can be caused by many things, but this is one of the most common signs that your long-acting insulin is not set up to cover your background need.
Keep in mind, most control problems have nothing to do with gastroparesis. So always consult with your physician about this.
Before Taking This Medicine
You should not use Lantus if you are allergic to insulin, or if you are having an episode of hypoglycemia .
Lantus is not approved for use by anyone younger than 6 years old, and should not be used to treat type 2 diabetes in a child of any age.
To make sure Lantus is safe for you, tell your doctor if you have:
-
liver or kidney disease; or
-
low levels of potassium in your blood ;
Tell your doctor if you also take pioglitazone or rosiglitazone . Taking certain oral diabetes medicines while you are using insulin may increase your risk of serious heart problems.
Tell your doctor if you are pregnant or breastfeeding.
Follow your doctor’s instructions about using Lantus if you are pregnant or you become pregnant. Controlling diabetes is very important during pregnancy, and having high blood sugar may cause complications in both the mother and the baby.
Recommended Reading: What Happens If You Stop Taking Diabetes Medication
Elevated A1c And Glycemic Variability
There has been some uncertainty about the relative effect of CSII and MDI at improving glycemic control as measured by A1C, but it is now clear from several studies that the change in A1C when switching from MDI to CSII depends on the initial A1C values on injections: the most poorly controlled patients on MDI improve the most on CSII . Interestingly, one factor that is a major determinant of A1C on MDI is the glycemic variability, the swings both within and between days . This is important because the target group of hypoglycemia-prone type 1 diabetic subjects often maintain a high A1C because they may have learned that their large fluctuations in blood glucose will precipitate hypoglycemia when attempts are made to tighten control with MDI . Such patients do well on insulin pumps, with the lower glycemic variability on CSII being one of the factors allowing a reduced frequency of hypoglycemia and lower A1C.
Figure 2
Correlation in type 1 diabetes between the A1C on MDI and the subsequent change in A1C when patients were switched to CSII. From Pickup et al. , with permission.
Figure 3
A1C in hypoglycemia-prone type 1 diabetic subjects when treated by MDI based on glargine and after switching to CSII.
Table 2
Some randomized controlled trials showing a comparable mean A1C percentage during isophane -based MDI and long-acting analogbased MDI in type 1 diabetes
Figure 4
The Problem Of Poor Control In Type 2 Diabetes
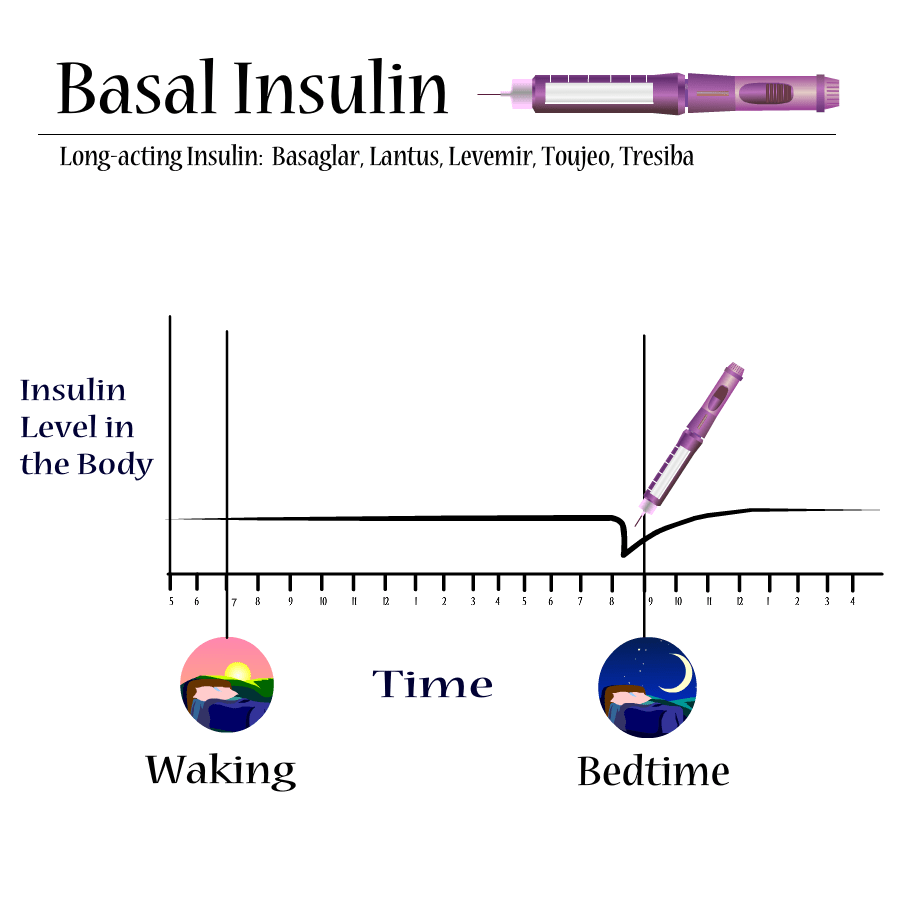
Gradual loss of -cell insulin secretion and persistent insulin resistance result, sooner or later, in the requirement for insulin therapy in most type 2 diabetic patients. To prevent complications in type 2 diabetes, strictly reinforced targets of blood glucose control provide further support for the need of optimized therapy. Initial bedtime basal insulin injection, sometimes combined with oral antidiabetic drugs, is among the most widely used regimens, but maintaining blood glucose control will then often need adaptations of insulin regimens toward MDI .
Recommended Reading: Adipsic Diabetes Insipidus
Questions From The Audience
Have you found that A1C deteriorates in pump-treated patients?
Although many patients can maintain an excellent and constant level of A1C during CSII, the A1C in some patients does worsen after a year or two. In response to this, we have now instituted a refresher course for established CSII patients in the Insulin Pump Clinic, where the pump nurse, dietitian, and doctor reeducate the patient in pump procedures. First indications are that this is helping to keep glycemic control at optimal levels.
Why cant we normalize the A1C on CSII?
It is possible to identify potentially correctable or understandable factors and largely uncorrectable or inexplicable factors that influence poor control on pump therapy. The first category includes cannula problems, pump malfunctions, poor timing or miscalculated or forgotten bolus doses at meals, intercurrent drugs such as alcohol and steroids, illness, and exercise. In the second category are problems in the pharmacology of insulin, such as delayed and unpredictable absorption from the subcutaneous site, variability of insulin sensitivity, and diabetic gastroparesis, with its delayed and erratic absorption of food.
A trial of an insulin pump is clearly suitable for poorly controlled patients on MDI: Are pumps also useful in patients with a normal or near-normal A1C on MDI?
What Is The Strongest Long
Almost every type of insulin can be divided into several sub-types, such as insulin basics, insulin glulisine, insulin lispro, etc. Each of those differs in the required frequency of the injection, the speed insulin reaches your blood, and the duration of its effect. The long-lasting hormone, for example, is subdivided into:
- Insulin glargine;
- Detemir;
- Degludec.
Despite the fact that each of the above-mentioned hormones can help your body keep a normal range of blood sugar for the entire day, the strongest long-lasting one is the degludec. While insulin detemir injection, for example, controls your blood sugar level for up to twenty-four hours, the effect of the insulin degludec injection lasts for about forty-two hours.
Don’t Miss: Can Type 2 Diabetics Eat Bananas
How Long Does Insulin Last In The Body
Natural insulin that is produced by a properly functioning body has a constant impact on it. On contrary, the duration of the injectable insulin depends on its type. When being more precise, there are many types of hormone, like inhaled insulin, animal insulin, etc. applied in insulin therapy:
- Rapid-acting insulin;
- Regular one ;
- Intermediate-acting insulin;
- Long-acting insulin;
- Pre-mixed insulin .
Each type of insulin has a different duration. For example, the effect of rapid-acting hormone lasts two to four hours, while regular insulin shots last for about five hours. The intermediate-acting hormone affects your body for up to eighteen hours, and the long-lasting one usually lasts for up to forty-two hours.
When To Bring Your Background To The Foreground
Topics covered in this article:
| Emotional Stress |
Diabetes control is the place where two worlds collidethe world of the known and the world of the unknown. You know certain things affect your blood sugarswhat you eat, how much insulin you take, when you take it, and the exercise you do. When you take charge of these areas, you often have good blood sugar readings.
But sometimes, out of nowhere, your blood sugars lose their track and start running out of control. As far as you are aware, youre doing the same things as before. You run through your usual troubleshooting questions. But one question many people dont get to is, Is it time to adjust my long-acting insulin?
Long-acting insulins, whether a dose or doses of L, UL, or NPH or the basal rate in the pump, are typically given to control the blood sugar when you are not eating. Fuel as glucose or fat is released into the bloodstream around the clock to keep the body running. So long-acting insulin or basal insulin has to be in the bloodstream around the clock to assist the movement of glucose into cells.
Long-acting insulin is background insulinoften out of sight and out of mind. Usually, thats okay. Its job is usually less than dramatic, not responding to the turmoil, crisis, and carbohydrates of life like Regular or Humalog. Its usually the last thing you adjust to solve a problem. But there are times when adjusting the long-acting or basal insulin has to be considered.
Also Check: Does Diet Soda Raise Insulin Levels

