What Happens If I Have Too Little Insulin
People with diabetes have problems either making insulin, how that insulin works or both. The main two types of diabetes are type 1 and type 2 diabetes, although there are other more uncommon types.
People with type 1 diabetes produce very little or no insulin at all. This condition is caused when the beta cells that make insulin have been destroyed by antibodies , hence they are unable to produce insulin. With too little insulin, the body can no longer move glucose from the blood into the cells, causing high blood glucose levels. If the glucose level is high enough, excess glucose spills into the urine. This drags extra water into the urine causing more frequent urination and thirst. This leads to dehydration, which can cause confusion. In addition, with too little insulin, the cells cannot take in glucose for energy and other sources of energy are needed to provide this energy. This makes the body tired and can cause weight loss. If this continues, patients can become very ill. This is because the body attempts to make new energy from fat and causes acids to be produced as waste products. Ultimately, this can lead to coma and death if medical attention is not sought. People with type 1 diabetes will need to inject insulin in order to survive.
Muscle And Fat Storage
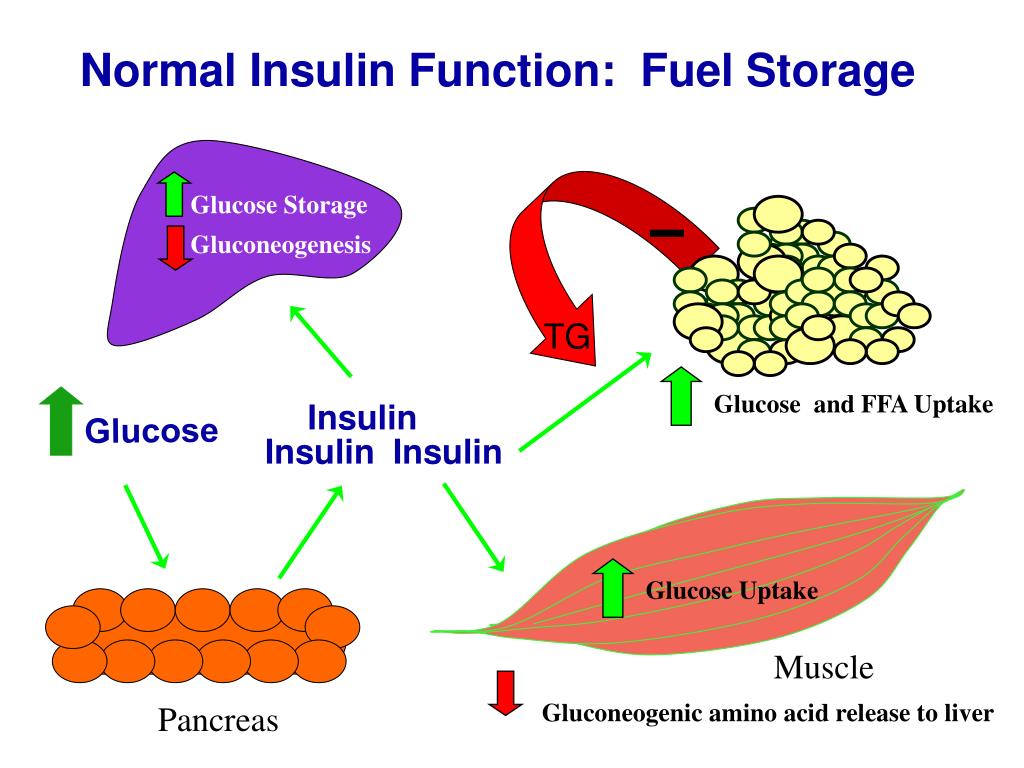
Insulin helps your muscles and fat cells store extra glucose so it doesnt overwhelm your bloodstream.
It signals your muscle and fat tissue cells to stop breaking down glucose to help stabilize your blood sugar level.
The cells then begin creating glycogen, the stored form of glucose. Glycogen provides your body with energy when your blood sugar level drops.
When your liver can hold no more glycogen, insulin triggers your fat cells to take in glucose. Its stored as triglycerides, a type of fat in your blood, that can be used for energy later.
Role Of Leukocytes In Systemic Insulin Resistance
In recent years, foundations have been established due to the discovery of immunometabolism as a field of science that has 2 aspects: the first is to understand how changes in cellular metabolism contribute to regulation of the functions of immune cells, such as their activation, polarization, differentiation, and proliferation, whereas the second focuses on understanding how leukocytes modulate cellular processes in tissues to drive the necessary changes in the body in response to environmental stimuli.
Initially, it was considered that in adipose tissue, proinflammatory molecules had a central role in the development of insulin resistance however, it was determined that the cells of the immune system infiltrated in these tissues were the ones that significantly modulated the generation. In fact, many of the immune cells, including macrophages, B and T cells, neutrophils and eosinophils, are involved in the production of cytokines during chronic inflammation.
You May Like: What Are Normal A1c Levels For Non Diabetic
Energy Metabolism Of Leukocytes
Glucose is the primary energy-producing molecule. Once it enters cells, 3 main interconnected metabolic pathways are responsible for the generation of ATP from glucose: glycolysis, the tricarboxylic acid cycle and oxidative phosphorylation . Glycolysis occurs in the cytoplasm and begins with the generation of glucose-6-phosphate, a reaction mediated by hexokinase , which prevents glucose from leaving the cell. Subsequent enzymatic reactions generate 2 molecules of NADH, 2 ATP, and 2 pyruvates as final products. The availability of oxygen determines the next step in the metabolic pathways, under hypoxic conditions, hypoxia-inducible factor 1 is the main driver of glycolysis where pyruvate is converted into lactate by the enzyme lactate dehydrogenase , which produces oxidized NAD+ molecules from NADH that favor the continuity of glycolysis. Under normoxic conditions, pyruvate is converted to acetyl coA, which enters the TCA in the mitochondria, which, through NADH and reduced flavin adenine dinucleotide, maintains the electron transport chain and, finally, OP, which ultimately produces ATP. A pathway derived from glycolysis and glucose-6-phosphate is the pentose phosphate pathway, which is necessary for the production of ribose or NADPH, whereas fatty acid oxidation and glutaminolysis replace the acetyl coA and -ketoglutarate metabolites, respectively, which can be used during the anabolism of proliferating cells.,
FIGURE 1
How Insulin Functions On A Cellular Level
The primary functions of insulin in the body’s cells have to do with the metabolism of carbohydrates, fats, and amino acids from protein as well as the transcription and translation of mRNA.
- Carbohydrates: Insulin contributes to carbohydrate metabolism at many points during the process. It facilitates the diffusion of glucose from carbohydrates into fat and muscle cells, signals the presence of an abundance of intracellular energy, and more.
- Fats: Insulin instigates the synthesis of fatty acids in adipose tissue as well as in the liver and in the mammary glands during lactation. It also affects the metabolism of phospholipids.
- Protein: Insulin stimulates protein synthesis throughout the body. It also contributes to the transcription of mRNA as well as aiding translation of mRNA into ribosomal proteins.
In a big-picture sense, insulin’s role has to do with the regulation of the body’s cellular energy supply and the balance of micronutrients. When the body is in a fed, as opposed to fasting, state, insulin orchestrates the anabolic processes that lead to muscle growth , tissue healing, and more. Insulin signals an abundance of energy, indicating to the body that it can halt the breakdown of fat stores and instead carry out fat synthesis.
Don’t Miss: Can Metformin Cause Heart Problems
Energy Creation And Distribution
The function of insulin is to help transform glucose into energy and distribute it throughout your body, including the central nervous system and cardiovascular system.
Without insulin, cells are starved for energy and must seek an alternative source. This can lead to life threatening complications.
Insulin And Blood Glucose Levels
Insulin helps control blood glucose levels by signaling the liver and muscle and fat cells to take in glucose from the blood. Insulin therefore helps cells to take in glucose to be used for energy.
If the body has sufficient energy, insulin signals the liver to take up glucose and store it as glycogen.
The liver can store up to around 5% of its mass as glycogen.
Some cells in the body can take glucose from the blood without insulin, but most cells do require insulin to be present.
Don’t Miss: What Color Is Diabetes Awareness Ribbon
Insulin Resistance And Cardiovascular Disease
Approximately 5070% of required ATP as fuel for the myocardium is produced by fatty acids oxidation. Glycolysis contributes less than 10% of the overall ATP production in the healthy heart . Although there seems to be a preferential use of fatty acids for the production of energy, the heart has the ability to change to another substrate for the generation of ATP, depending on availability, to ensure its energy demand. But also the substrate transporters, GLUT4 and CD36 , play a role in this dynamic balance of substrate utilization . During injury, the heart shifts from using fatty acids as energetic substrates toward glucose, but this metabolic flexibility is impaired under insulin resistance, leaving to fatty acid as the sole fuel source. This shift induces an increase in the uptake and accumulation of lipid in the heart, producing lipotoxicity . In this sense, the balance between lipid degradation and glucose oxidation could decrease diabetic cardiomyopathy . Likewise, the overexpression of glucose transporter-4 and/or the elimination of CD36 could represent an objective for the development of a new generation drugs for the treatment of diabetic cardiomyopathy.
Who Does Insulin Resistance Affect
Insulin resistance can affect anyone you dont have to have diabetes and it can be temporary or chronic. The two main factors that seem to contribute to insulin resistance are excess body fat, especially around your belly, and a lack of physical activity.
People who have prediabetes and Type 2 diabetes usually have some level of insulin resistance. People with Type 1 diabetes can also experience insulin resistance.
Also Check: What Happens With Diabetes
Insulin Clearance By The Liver: Its Receptor
Pulsatile delivery of insulin through the portal vein to the liver
The liver is the first organ that insulin encounters along its journey. Accordingly, the liver is uniquely exposed to higher concentrations of insulin than other insulin-responsive tissues such as muscle and fat. The portal vein delivers insulin from the pancreas to the liver in discrete pulses that occur every 5 min , where the amplitude of these insulin pulses is 0.51 nmol/liter in the fasted state and rises to 5 nmol/liter after a meal . Pulsatile insulin delivery to the liver is an important physiological signal that regulates both hepatic insulin action and insulin clearance , although the cellular underpinnings of how hepatocytes sense pulsatility are unknown.
The portal circulation delivers insulin into the capillaries of the sinusoids, which are not supported by a basement membrane and their endothelial cells contain fenestrations , together permitting the exchange of contents between the blood and the surrounding liver cells. The unique structure of the hepatic sinusoids allows insulin to easily diffuse out of the circulation and into the perisinusoidal space, where it comes into contact with hepatocytes .
CEACAM1 and insulin-degrading enzyme : Hepatic molecules driving insulin clearance
What Is The Difference Between Insulin Resistance And Diabetes
Anyone can develop insulin resistance temporarily or chronically. Over time, chronic insulin resistance can lead to prediabetes and then Type 2 diabetes if its not treated or able to be treated.
Prediabetes happens when your blood glucose levels are higher than normal, but not high enough to be diagnosed as diabetes. Prediabetes usually occurs in people who already have some insulin resistance.
Prediabetes can lead to Type 2 diabetes , the most common type of diabetes. T2D happens when your pancreas doesnt make enough insulin or your body doesnt use insulin well , resulting in high blood glucose levels.
Type 1 diabetes happens when your bodys immune system attacks and destroys the insulin-producing cells in your pancreas for an unknown reason. T1D is an autoimmune and chronic disease, and people with T1D have to inject synthetic insulin to live and be healthy. While T1D is not caused by insulin resistance, people with T1D can experience levels of insulin resistance in which their cells dont respond well to the insulin they inject.
Gestational diabetes is a temporary form of diabetes that can happen during pregnancy. Its caused by insulin resistance thats due to the hormones the placenta makes. Gestational diabetes goes away once you deliver your baby. Approximately 3% to 8% of all people who are pregnant people in the United States are diagnosed with gestational diabetes.
Don’t Miss: Is Hyperglycemia The Same As Diabetes
What Is Insulins Role In Type 2 Diabetes
Type 2 diabetes, similar to type 1, is a chronic illness that occurs when it is too much glucose in your blood. However, type2 diabetes, unlike type 1 diabetes, takes place not because your body does not make insulin but rather because your muscle cells, liver cells, and fat cells do not respond to too much insulin correctly. Due to your body cells insulin resistance, the sugar can not be delivered to them and is thus stored in your blood.
People with diabetes of this type are not dependent on insulin therapy, because their body is still capable of producing insulin. Thus, maintaining a healthy diet with a special diabetes menu, leading an active lifestyle, controlling your blood pressure, and keeping your optimal weight can help you regulate your blood sugar levels.
Functions Of Insulin In The Body: Good Guy Or Bad Guy

Insulin is perhaps the most important compound circulating in our bodies. It is involved in more than 60 key biological processes. Impairments in insulin function affect many facets of health and well-being and, if left uncorrected, are ultimately fatal. Despite its paramount importance, the functions of insulin in the body are widely misunderstood.
Insulin is an anabolic hormone, meaning it acts to promote synthesis and building, as opposed to catabolic hormones that break down and deconstruct bodily tissues and compounds. Given its vital importance, it is curious that insulin is sometimes portrayed as the bad guy. Consider, for instance, how we cast insulin as the villain responsible for the development of adverse health conditions: type 1 and type 2 diabetes, metabolic syndrome, polycystic ovary syndrome, and even certain types of cancer.
In this article, we will explore the basic functions of insulin in the body to gain a better appreciation for all it does as well as a clearer understanding of how to keep this hormone functioning in balance and at its optimal capacity.
Also Check: Symptoms Of High Glucose Levels
As An Anabolic Hormone
Remember that insulin is an anabolic hormone as well because it promotes the conversion of small molecules in the blood, such as glucose, fats, and amino acids, into large molecules inside cells. Because of this role, insulin also functions by decreasing proteolysis or the breaking down of protein into smaller polypeptides or amino acids, autophagy or the level of degradation of damaged cellular organelles, and lipolysis or breakdown of fats into glycerol and free fatty acids. While insulin promotes the storage of energy as fats into fat tissues, thus leading to fat accumulation in the body, proper weight management through nutrition and physical training can also promote storage of energy as proteins in the muscles, thus leading to muscle growth.
The Involvement Of Insulin In Glucose Metabolism
The insulin receptor is constitutively expressed on the plasma membrane of both monocytes and neutrophils, and its expression does not change as a function of insulin concentration. There is no evidence to date that had directly evaluated expression of the receptor in eosinophils and basophils, although as they are granulocytes, it is very likely that their expression is similar to that of neutrophils. However, in lymphocytes, expression of the insulin receptor is not constitutive but is positively regulated in response to insulin, and the effect is potentiated during its activation.- These findings suggest the probable participation of insulin in the regulation of metabolism in these immune cells.
In monocytes, insulin increases the transport and utilization of glucose,- whereas in neutrophils, insulin does not seem to regulate glucose uptake however, it shows an influence on glucose metabolism once transported to the cytoplasm, regulating molecules that participate in glycolysis., Glucose enters the cell by facilitated diffusion through the glucose transporter protein GLUT. Expression of GLUT in the membrane is crucial for increased glucose uptake in activated leukocytes. Fourteen isoforms expressed in humans have been described, of which GLUT1-4 are the most studied, and leukocytes express the GLUT1 and GLUT3 isoforms independent of insulin stimulation, as well as GLUT4, which has been shown to be dependent of insulin-activated signaling.,
You May Like: Pita Bread And Diabetes
Biosynthesis And Export Of Insulin In Pancreatic
Insulin synthesis, processing, and packaging in pancreatic -cells
Humans have a single insulin gene, INS , located on chromosome 11, the transcription of which is controlled largely by upstream enhancer elements that bind key transcription factors that include IDX1 , MafA, and NeuroD1 along with numerous coregulators . In the insulin-producing pancreatic -cells, these are required for insulin gene expression and contribute to the regulation of INS transcription in response to glucose and autocrine insulin signaling . Given the role of these enhancer elements, transcription factors, and their coregulators in controlling the expression of insulin and many additional components of the -cell secretory pathway, such as glucose transporter 2 and the insulin processing enzyme PC1/3, they are key defining contributors to the establishment and maintenance of -cell identity .
Transit of immature secretory granules through the TGN, and their subsequent budding and maturation, is controlled by a host of regulatory proteins, including newly identified vesicle-sorting by proteins such as SORCS1 and HID-1 . Insulin biosynthesis in this manner is generally rapid and efficient, with only 12% of the protein remaining as proinsulin within mature secretory granules where insulin couples with Zn2+ and exists as a hexameric crystal with the cation. Transport of the insulin hexamer into the secretory granules is thought to be mediated by ZnT8 or related zinc transporters .
Quick Answer: What Role Does Insulin Play In Diabetes
Insulin helps control blood glucose levels by signaling the liver and muscle and fat cells to take in glucose from the blood. Insulin therefore helps cells to take in glucose to be used for energy. If the body has sufficient energy, insulin signals the liver to take up glucose and store it as glycogen.
Recommended Reading: What Cheese Can A Diabetic Eat
What Is Insulins Role In Type 1 Diabetes
Type 1 diabetes is a lifelong illness that is characterized by excess glucose in the blood. It usually occurs when your beta cells do not produce insulin properly because your immune system destroys them mistakenly. As a result, your body cells do not get or store glucose that resulting in them being incapable of using glucose for energy, as it is not delivered to them but is rather stored in your blood. When having this type of disease, a person becomes dependent on insulin to regulate blood sugar and, thus, has to take it regularly. However, thanks to the advancements of contemporary medicine, health care providers give you the possibility to choose the most convenient method of intaking insulin. For example, people with type 1 diabetes might regulate the level of their blood sugar with the help of:
- An insulin pump, which is a device that mimics the way insulin works in a healthy body. Insulin pumps deliver small amounts of inhaled insulin to body cells on a constant basis
- An insulin injection, which allows you to inject insulin in a couple of different methods. Injectable insulin therapy can employ a syringe and a vial, an insulin pen, and other things to deliver insulin to your body
- Etc.
Moreover, there are various types of insulin you can intake to maintain your glucose levels, such as rapid-acting insulin, short-acting insulin intermediate-acting insulin, long-active insulin, mixed types of insulin, etc.

