Does Lantus Insulin Raise Or Lower Blood Sugar Levels
Lantus lowers high blood sugar levels.
Lantus is the man made form of a long acting insulin that is given by injection to diabetic patients, to lower their high blood sugar levels.
- Normally our bodies naturally produce the hormone insulin which works to keep the levels of sugar in our blood to the ideal range.
- People who have diabetes have high blood sugar levels regularly due to their body not producing enough insulin or their body has become resistant to the effect of insulin.
- Lantus insulin carries the excess blood sugar from your bloodstream and stores it in your bodys tissues to use for energy later on.
- Lantus lowers the high blood sugar levels that diabetic patients have so that the blood glucose levels are a more normal range.
How Does Intermittent Fasting Affect Glucose Levels
Intermittent fasting is the intentional restricting of our mealtimes to maximize health. Media coverage tends to paint IF as the latest fad diet ⦠except itâs neither a fad nor a diet. IF existed long before it blipped on Google Trends . IF lacks other dietsâ bizarre rules: âeat only grapefruitâ or âdrink cabbage juice.â
IF really isnât a âdiet.â Think of intermittent fasting like the dietary cousin to restricting kidsâ screen time. Limiting computer time keeps our kids from gorging on YouTube and helps their developing brains. IF does the same for our bodies.
Response To An Increase In Blood Glucose
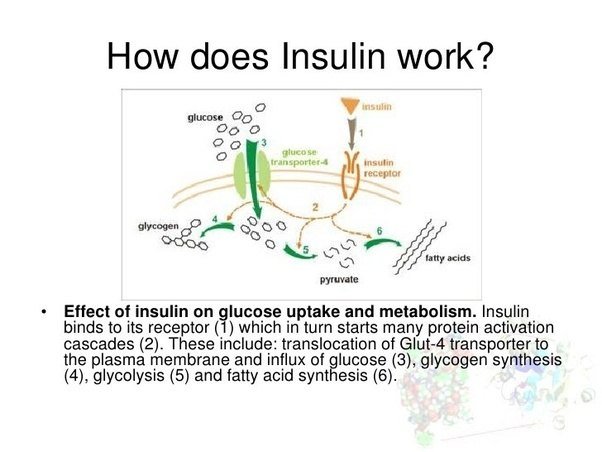
In the absorptive state, an increase in blood glucose is detected by the beta cells of the pancreatic islets, causing them to increase the release of insulin into the blood. Insulin stimulates cells, especially adipose and muscle cells, to take up glucose from the blood.
Insulin and the transport of glucose into cells – To enter cells, glucose requires trans-membrane transporters and there is a family of these called GLUT . The most numerous is GLUT4, which is found on muscle and fat cells.
When insulin binds to insulin receptors on the cell membrane, cells are stimulated to increase the number of glucose transporters. The more transporters are produced, the more glucose is transported into cells – with a corresponding drop in blood glucose.
The precise mechanism whereby insulin binds to receptors causing translocation is still to be determined .
Not all tissues require insulin to take up glucose, for example brain and liver cells use GLUT transporters that are not dependent on insulin.
Further effects of insulin – The hormone also has other effects on the bodys cells, all of which contribute to an increase in glucose usage and storage – and therefore a reduction in blood glucose. These include:
– The promotion of glycolysis, a process that breaks down glucose for cellular energy
– The promotion of glycogenesis, a process that converts glucose into glycogen for storage
– The inhibition of lipolysis, a process that breaks down lipids to release energy.
Also Check: How Much Does Metformin Lower Fasting Blood Sugar
Early Time Restricted Eating
One of the hidden superpowers of IF is how it boosts our natural circadian rhythms. Deep within everyoneâs brain is a master clock that, taking into account external data such as sunlight, nudges our bodies toward certain activities. This circadian rhythm, as it’s called, is like having a smartphone pre-set with a whole dayâs worth of alarmsâwake up, eat lunch, etc.âbut much less annoying.
Our circadian rhythm includes a glucose/insulin timer. Sensitivity to insulin actually decreases as the day wears on. It takes our bodies longer to process a piece of toast at 9 PM than it does at noon. Those who practice early time-restricted feeding IF, , boost insulinâs circadian effectiveness. Overall insulin sensitivity rises. Mean glucose levels fall. By shifting our eating window earlier in the day, we are aligning our food intake with when our body is naturally most insulin sensitive, reducing spikes in insulin and blood sugar.
Evolution And Species Distribution
Insulin may have originated more than a billion years ago. The molecular origins of insulin go at least as far back as the simplest unicellular eukaryotes. Apart from animals, insulin-like proteins are also known to exist in the Fungi and Protista kingdoms.
Insulin is produced by beta cells of the pancreatic islets in most vertebrates and by the Brockmann body in some teleost fish.Cone snailsConus geographus and Conus tulipa, venomous sea snails that hunt small fish, use modified forms of insulin in their venom cocktails. The insulin toxin, closer in structure to fishes’ than to snails’ native insulin, slows down the prey fishes by lowering their blood glucose levels.
Don’t Miss: What Is Max Dose Of Metformin
Vphysiology Of Insulin Secretion In Vivo
Insulin secretionin vivo has also been extensively studied. As predictable from the studies of single beta cells described above, the most important regulators of insulin secretion are circulating nutrients, in particular, glucose. In the fasting state, insulin secretion is maintained at levels that provide sufficient insulin to constrain hepatic glucose release at rates that match glucose utilization and so the plasma glucose concentration is maintained at normal levels of 90 mg/dl . After meal ingestion, glucose concentrations in the circulation rise and stimulate insulin secretion . Increased delivery of insulin into the circulation causes further suppression of hepatic glucose release and increased stimulation of glucose uptake by insulin-sensitive tissues such as muscle to restore normoglycemia. Therefore, the simplest model to describe insulin secretion in vivo would have two components: a constant basal rate of insulin secretion superimposed on which are meal-related increments. Although this model is commonly employed by physicians attempting to replace insulin in patients who secrete insufficient insulin, it is an oversimplification of a very complex dynamic neuroendocrine secretory system.
Juris J. Meier, in, 2016
In The Second Part Of The Series On Drug Interactions That Persons With Diabetes Should Watch Out For We Talk Of Which Medicines Increase Or Decrease Your Blood Glucose Level And What You Should Watch Out For
Often persons with diabetes are on medications other than the diabetes drugs . They may be on some medications for life for chronic conditions or acute conditions . Drug interactions are known to occur between 2 sets of drugs. For such patients, such interacts can be crucial as they can tamper the blood glucose levels. The specific pathway behind such mechanisms may not be fully known, but it is hypothesized that certain drugs cause a decrease in peripheral insulin sensitivity, increase the gluconeogenesis or decrease insulin secretion from the cells of the pancreas. Concurrently, if the glucose levels seem uncontrollable, it would be wise to investigate whether a simultaneous or new medicine is responsible for it.
Lets look at medications that are known to affect blood sugar levels.
Don’t Miss: Diabetes And Dizziness
Structural Analysis And Synthesis
Purified animal-sourced insulin was initially the only type of insulin available for experiments and diabetics. John Jacob Abel was the first to produce the crystallised form in 1926. Evidence of the protein nature was first given by Michael Somogyi, Edward A. Doisy, and Philip A. Shaffer in 1924. It was fully proven when Hans Jensen and Earl A. Evans Jr. isolated the amino acids phenylalanine and proline in 1935.
The amino acid structure of insulin was first characterized in 1951 by Frederick Sanger, and the first synthetic insulin was produced simultaneously in the labs of Panayotis Katsoyannis at the University of Pittsburgh and Helmut Zahn at RWTH Aachen University in the mid-1960s.Synthetic crystalline bovine insulin was achieved by Chinese researchers in 1965. The complete 3-dimensional structure of insulin was determined by X-ray crystallography in Dorothy Hodgkin‘s laboratory in 1969.
Two other Nobel Prizes have been awarded for work on insulin. British molecular biologist Frederick Sanger, who determined the primary structure of insulin in 1955, was awarded the 1958 Nobel Prize in Chemistry.Rosalyn Sussman Yalow received the 1977 Nobel Prize in Medicine for the development of the radioimmunoassay for insulin.
How Can Diet Affect Insulin Resistance
Your diet has a big impact on your blood sugar and insulin levels. Highly processed, high-carbohydrate and high-fat foods require more insulin.
In general, eating foods that have a low to medium glycemic index and limiting foods that have a high glycemic index can help you reverse and/or manage insulin resistance. Eating foods with fiber also helps regulate blood sugar levels because it takes your body longer to digest fiber, meaning your blood sugar levels dont spike as much.
The glycemic index is a measurement that ranks foods containing carbohydrates according to how much they affect your blood sugar levels. The Glycemic Index Foundation classifies the GI of foods as either low, medium or high, with pure glucose generally as a reference at 100:
- Low GI: 55 or less.
- Medium GI: 5669.
- High GI: 70 or greater
High-GI foods generally have a lot of carbohydrates and/or sugar and low to no fiber content. Low-GI foods generally have low amounts of carbohydrates and higher amounts of fiber.
Examples of foods with a high GI include:
- White bread.
- Indigenous people from the continental United States.
- Indigenous people from the Pacific Islands.
Although you cant change certain risk factors for insulin resistance, such as family history or age, you can try lowering your chances of developing it by maintaining a healthy weight, eating a healthy diet and exercising regularly.
Also Check: Can Metformin Cause Blurry Vision
How Does Insulin Lower Blood Glucose Levels Quizlet
blood glucose levelsinsulinblood glucoseglucose
. Correspondingly, how does insulin regulate blood sugar levels?
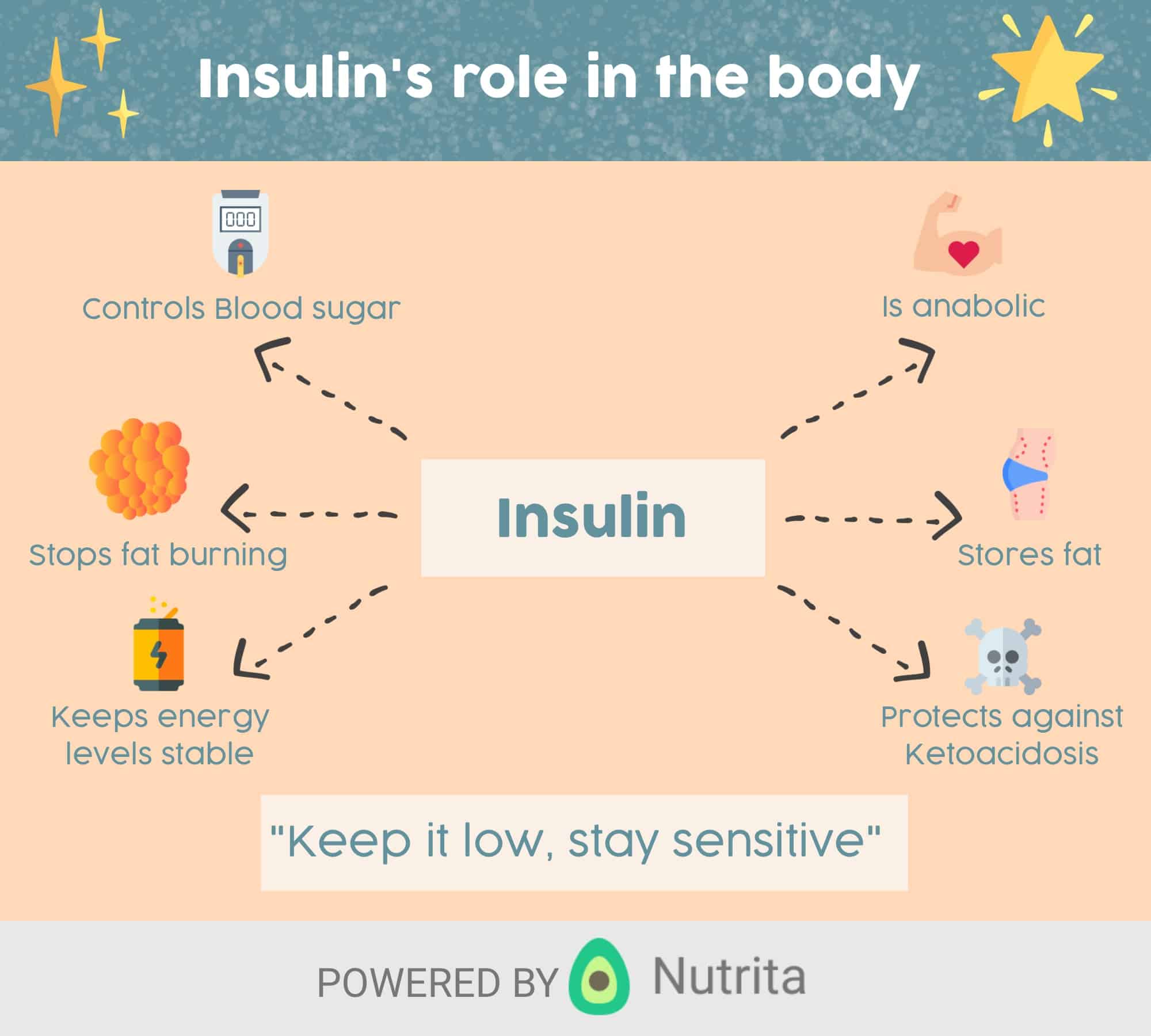
Insulin helps control blood glucose levels by signaling the liver and muscle and fat cells to take in glucose from the blood. Insulin therefore helps cells to take in glucose to be used for energy. If the body has sufficient energy, insulin signals the liver to take up glucose and store it as glycogen.
Likewise, which hormones are responsible for maintaining blood glucose levels quizlet?
Then, when blood sugar levels decrease what happens to insulin and glucagon?
When blood sugar drops too low, the level of insulin declines and other cells in the pancreas release glucagon, which causes the liver to turn stored glycogen back into glucose and release it into the blood. This brings blood sugar levels back up to normal.
Which event would increase blood glucose levels quizlet?
When blood glucose levels are low, glucagon stimulates in the liver to break down stored glycogen and increase the levels of blood glucose. Epinephrine acts on the liver to stimulate from noncarbohydrate sources. Growth hormone stimulates to provide fuel for energy from fatty acids stored in adipose tissue.
How Does Insulin And Glucagon Regulate Glycolysis
insulinwillcanGlucagon doeswill
. Likewise, people ask, how does insulin and glucagon regulate blood sugar?
Insulin helps the cells absorb glucose, reducing blood sugar and providing the cells with glucose for energy. When blood sugar levels are too low, the pancreas releases glucagon. Glucagon instructs the liver to release stored glucose, which causes blood sugar to rise.
Beside above, does insulin increase glycolysis? Insulin has the opposite effect on these enzymes. Thus the phosphorylation of phosphofructokinase inhibits glycolysis, whereas its dephosphorylation through the action of insulin stimulates glycolysis.
In this manner, how does insulin regulate glycolysis?
Glycolysis is regulated by a key bifunctional enzyme, 6-phosphofructo-2-kinase/fructose-2,6-bisphosphatase 1 . Insulin dephosphorylates phosphorylated-PFKFB1 and activates its kinase activity, thereby promoting glycolysis .
Why does glucagon inhibit glycolysis?
Glucagon generally elevates the concentration of glucose in the blood by promoting gluconeogenesis and glycogenolysis. Glucagon turns off glycolysis in the liver, causing glycolytic intermediates to be shuttled to gluconeogenesis. Glucagon also regulates the rate of glucose production through lipolysis.
You May Like: Diabetes Causing Hypertension
General Treatment Of Diabetes
People with diabetes benefit greatly from learning about the disorder, understanding how diet and exercise affect their blood glucose levels, and knowing how to avoid complications. A nurse trained in diabetes education can provide information about managing diet, exercising, monitoring blood glucose levels, and taking drugs.
|
|
Managing Your Diabetes Devices
If you are using an insulin pump, talk to your diabetes team about how to best manage hyperglycemia. In general, be sure to check your pump first. Make sure all parts are connected and working correctly. Check your bolus history and temporary basal rate. Also check your insulin to make sure it has not expired or gotten too warm.
If you use a CGM, try not to react to it too often. You might be tempted to give another dose of insulin too soon, before the first one finishes working, which is known as stacking insulin this can cause low blood sugar .
You May Like: Overdose Of Diabetic Tablets
The Basics Of High Blood Sugar
Diabetes is a problem with your body that causes blood sugar levels to rise higher than normal. This is also called hyperglycemia.
When you eat, your body breaks food down into sugar and sends it into the blood. Insulin then helps move the sugar from the blood into your cells. When sugar enters your cells, it is either used as fuel for energy right away or stored for later use. In a person with diabetes, there is a problem with insulin. But, not everyone with diabetes has the same problem.
There are different types of diabetestype 1, type 2 and gestational diabetes. If you have diabetestype 1, type 2 or gestationalyour body either doesnt make enough insulin, cant use the insulin well, or both.
Dont Miss: What Is The Best Fruit For Diabetics To Eat
References And Recommended Reading
Ahrén, B. Islet G protein-coupled receptors as potential targets for treatment of type 2 diabetes. Nature Reviews Drug Discovery8, 369385 . doi:10.1038/nrd2782.
Kebede, M. A., Alquier, T., et al. Lipid receptors and islet function: therapeutic implications? Diabetes, Obesity and Metabolism11, 1020 . doi: 10.1111/j.1463-1326.2009.01114.x.
Kim, H., Toyofuku, Y., et al. Serotonin regulates pancreatic beta cell mass during pregnancy. Nature Medicine16, 804808 . doi:10.1038/nm.2173.
Langenberg, C., Pascoe, L., et al. Common genetic variation in the melatonin receptor 1B gene is associated with decreased early-phase insulin response. Diabetologia52, 15371542 . doi: 10.1007/s00125-009-1392-x.
Regard, J. B., Kataoka, H., et al. Probing cell type-specific functions of G in vivo identifies GPCR regulators of insulin secretion. Journal of Clinical Investigation117, 40344043 . doi:10.1172/JCI32994.
Rosengren, A. H., Jokubka, R., et al. Overexpression of alpha2A-adrenergic receptors contributes to type 2 diabetes. Science327, 217220 . doi: 10.1126/science.1176827.
Winzell, M. S. & Ahren, B. G-protein-coupled receptors and islet function-implications for treatment of type 2 diabetes. Pharmacology and Theraputics116, 437448 . doi:10.1016/j.pharmthera.2007.08.002.
Don’t Miss: What Is The Max Dose Of Metformin
Glucagon And Alpha Cells
To date, the characterization of GPCRs in islets has focused largely on beta cells, so less is known about the role of GPCRs in alpha cells. Interestingly, alpha cells not only secrete glucagon, but they also express the glucagon receptor, which is itself a GPCR. Thus, glucagon is both secreted by and acts on alpha cells to regulate their own secretion. Along with the glucagon receptor, it is likely that alpha cells express additional GPCRs that play roles in glucagon secretion. Researchers are actively seeking to characterize these receptors, because GPCRs that regulate glucagon secretion may be excellent targets for diabetes therapies due to their overall importance in the regulation of islet function.
Other Hormones That Are Involved In The Regulation Of Blood Glucose
Like most of the physiological processes, the regulation of blood glucose is complex and there are many other hormones beside insulin and glucagon that play an important function, such as somatostatin.
The role of somatostatin – This is released by the delta cells located in the pancreatic islets in response to a post-prandial increase in blood glucose and amino acids. It reduces gut motility and the further absorption of nutrients as well as inhibiting pancreatic exocrine secretions.
The function of gastrin and cholecystokinin – The gastrointestinal tract also releases hormones such as gastrin and cholecystokinin that stimulate the pancreas to secrete insulin in anticipation of the absorption of nutrients.
The role of stress hormones – When a person is experiencing stress, neuro-endocrine mechanisms cause the release of stress hormones such as adrenaline . These increase blood-glucose levels by mobilising glycogen and suppressing the release of insulin.
Other hormones such as amylin and pancreatic polypeptide are involved in glucose regulation but their roles are less well understood.
A summary of the principal hormones involved in glucose regulation is presented in Table 1.
Recommended Reading: What Cheese Is Good For Diabetics
Epinephrine Cortisol And Growth Hormone:
Epinephrine, cortisol, and growth hormone are other hormones that help maintain blood sugar levels. They, along with glucagon are called stress or gluco-counter-regulatory hormones which means they make the blood sugar rise.
Epinephrine is released from nerve endings and the adrenals, and acts directly on the liver to promote sugar production . Epinephrine also promotes the breakdown and release of fat nutrients that travel to the liver where they are converted into sugar and ketones.
Cortisol is a steroid hormone also secreted from the adrenal gland. It makes fat and muscle cells resistant to the action of insulin, and enhances the production of glucose by the liver. Under normal circumstances, cortisol counterbalances the action of insulin. Under stress or if a synthetic cortisol is given as a medication , cortisol levels become elevated and you become insulin resistant. When you have Type 1 diabetes, this means your may need to take more insulin to keep your blood sugar under control.
Growth Hormone is released from the pituitary, which is a part of the brain. Like cortisol, growth hormone counterbalances the effect of insulin on muscle and fat cells. High levels of growth hormone cause resistance to the action of insulin.
Measurement Of Insulin And Insulin Resistance
There are a variety of approaches to the laboratory assessment of insulin resistance. Over the years the limited specificity of older radio-immunoassays that cross-react with proinsulin have reduced the credibility of measuring insulin resistance in clinical settings. Current assays have improved specificity and precision. A comprehensive review of insulin assays is beyond the scope of this review and the reader is encouraged to consult Sapin in this regard. Insulin resistance may be measured by looking directly at insulin mediated glucose uptake in the basal or post-stimulated state, by inference from the relative concentrations of glucose and insulin, or by looking at surrogate markers of insulin action.
Don’t Miss: Metformin Oral Side Effects

