Generics And Biosimilars Are Bringing Down The Overall Price Of Insulins
Since 2019, the overall retail price of insulins has declined by nearly 6%. Most of this decline can be attributed to the recent approval of generics, and the biosimilar counterparts that have been on the market.
In 2019, Eli Lilly released the first generic insulin, insulin lispro, the counterpart to the popular rapid-acting insulin . Since then, the FDA has approved generic versions of , , and .
At present, retail prices for generic insulin lispro and insulin aspart are about half that of their brand-name counterparts, Humalog and Novolog, respectively. The same goes for the generic mixed insulins, insulin lispro 75/25 and insulin aspart 70/30, compared to Humalog 75/25 and Novolog 70/30, respectively.
Generics have been instrumental in bringing down costs for some patients. Instead of paying a retail price of over $140 for a brand-name Humalog KwikPen, patients can now pay about $60 for a generic insulin lispro KwikPen. Similar savings can be found for the other brand and generic alternatives.
, a long-acting insulin approved in 2016, is the follow-on to Lantus, and , a rapid-acting insulin approved in 2017, is the follow-on to Humalog. Now, the average retail price per insulin unit for Basaglar is $0.27, while Lantus is $0.34. Similarly, Admelog has a price per unit of $0.28, while Humalog has a unit price of $0.44.
What Does The Future Of Insulation Costs Look Like
I am being told by the big-wigs that we should expect at least 2 if not 3 more price increases by the end of 2018. And most price increases are about 10%.
Plus, you gotta add in the 1% per month increase in construction labor costs, according to Independence Title. That is 12% per year increase. Hourly labor costs at my company in the last 5 years have increased 73%.
To further increase labor costs, we have the City of Austin new ordinance of mandatory paid sick leave, which increases labor costs about 5%.
Insulin Makers Lit The Fusepbms Fanned The Flames
“Insulin manufacturers lit the fuse on skyrocketing prices by matching each other’s price increases step for step rather than competing to lower them, while PBMs, acting as middlemen for insurers, fanned the flames to take a bigger cut of the secret rebates and hidden fees they negotiate,” added Sen. Ron Wyden, the Committee’s highest-ranking Democrat, from Oregon.
The three US insulin makers deny working with each other or PBMs.
Eli Lilly spokesman Greg Andrew Kueterman told Medscape Medical News that the company “makes independent decisions about list price increases.”
Similarly, a Sanofi spokesman said the company “makes all of its pricing decisions independently.”
And Michael Bachner, Novo Nordisk’s director of media relations, told Medscape Medical News that the company’s “pricing decisions are made independently and are based on a number of market dynamics, some of which include our competitors’ activities, current formulary access, and discussions with payers.”
Also Check: Which Of The Following Is Not Associated With Type 2 Diabetes
Committee Found Companies Raised Prices To Balance Out Rebates
To balance out rising rebates, insulin manufacturers in turn “aggressively” raised the list price of their insulin, the committee found.
“The investigation found that Novo Nordisk and Sanofi not only closely monitored the others’ price increases, they actually increased prices in lockstep sometimes within hours or days of each other a practice known as ‘shadow pricing,'” said the committee.
Internal emails also show that in 2014 Lilly executives decided to enact a list price increase for Humalog earlier than expected when the company heard Novo Nordisk had decided to increase list prices for its and Levemir products.
The committee documented list price increases of 50%-70% for insulins, sometimes over just a 3-year period.
The investigation also found after reviewing internal documents that drug makers often set prices based on whether it might harm a PBM’s or health plan’s bottom line. The goal was to keep those clients happy and to preserve market share, said the committee.
PBMs did not do anything to discourage the increases in list prices, said the committee. Instead, “PBMs used their size and aggressive negotiating tactics, like the threat of excluding drugs from formularies, to extract more generous rebates, discounts, and fees from insulin manufacturers.”
The PBM industry’s lobbying group, the Pharmacy Management Care Association , said it shared the committee’s “urgency in addressing affordability and access for insulin-dependent patients,” in a statement.
Senate Report Blasts Insulin Makers For High Prices
January 21, 2021 A new, bipartisan report from a key congressional committee is sharply critical of the three major drug manufacturers that sell insulin in the U.S. The companies Eli Lilly, Novo Nordisk, and Sanofi already have been all over the news recently for their pricing behavior. They also are the ringleaders of a group of drug companies that are circumventing federal law by refusing to provide 340B drug pricing program discounts to safety-net providers for drugs dispensed at community pharmacies.
The influential Senate Finance Committee released the report, which is the result of a two-year investigation by the panel. It concludes that the insulin-producing companies Eli Lilly, Novo Nordisk, and Sanofi aggressively raised the of their insulin products absent significant advances in the efficacy of the drugs. Those price increases often were the result of shadow pricing, where one company tracks whether its competitors are raising prices and raises its own price shortly after.
The investigation found that the three companies negotiated discounts with pharmacy benefit managers to be included in their drug formularies and then raised WAC prices. Each of the companies closely monitored the pricing decisions of their competitors and increased prices in lockstep. Sanofi and Novo Nordisk often announced price hikes within hours or days of each other, the report noted.
The committee reviewed pricing for insulin pens and reported that:
LATEST ARTICLES DELIVERED
You May Like: Is Greek Yogurt Ok For Diabetics
The Cost Of Insulin A Silver Lining
The good news: The drug companies now have plans in place to make insulin more accessible and more affordable.
Eli Lilly: 1-800-545-6962, can help with Humolog, Humulin and Humalog mix to those who qualify. 1-866-310-7549, can help with Levemir, Novolog, Novolog 70/30 mix, and Novolin to those who qualify.Sanofi: 1-888-847-4877, offers free or discounted Apidra, Lantus or Toujeo in a savings card to those who are eligible.
Please always consult with your physician if you cant afford your insulin. Do not stop taking insulin or change the dosage without guidance from your health care provider. They will always work with you and make the best recommendations.
Insulin has become more expensive but there are ways to deal with it. This is a difficult and delicate situation since insulin is not a luxury but a necessity. Change will hopefully come soon with biosimilar insulins close to approval. We must insist that patients have proper access to insulin and all the medications they need for a better quality of life.
NOTE: Consult your Doctor first to make sure my recommendations fit your special health needs.
What Is A Fqhc / Community Health Center
Federally Qualified Health Centers, or FQHCs, are care clinics that qualify for specific reimbursement systems under Medicare and Medicaid and receive federal Health Center Program grant money intended to finance care for uninsured populations. Their patients are disproportionately poor, uninsured, and minorities. They receive subsidies in the form of federal grants and enhanced Medicaid reimbursement. They are located in underserved rural communities and central cities, where other providers are unable economically or unwilling to locate.
The National Association of Community Health Centers confirmed that its member health centers already provide deeply discounted drug prices to the low-income families they serve. In a press release, NACHC explained that the regulation, , was based on a fundamental misunderstanding that would have imposed extensive administrative burdens and targeted EpiPens and insulin dispensed by health centers and purchased under the federal 340B drug discount program. The 340B rule would have blocked Community Health Centers from receiving future grant funding unless they provided a complete pass-through of 340B discounts on insulin and epi-pens to low-income patients. Community Health Centers strongly opposed the order, arguing that it would add significant bureaucratic obligations to operations while making a minimal impact on the costs of drugs it already provides to patients.
Read Also: Does Type 2 Diabetes Need Insulin
So Why The Price Change
One reason for higher pricing on these insulins are because of an annual tax on brand name pharmaceutical companies. This exempts generic drugs and was started in 2012 as part of the ACA . It originated as a $ 28 billion tax in 2012 and will grow to $40 billion in 2018 if left in place.
The drug companies Eli Lilly, Novo-Nordisk and Sanofi have Drug Savings Cards in place which allow patients who are qualified to decrease 30-day insulin supplies to $25.00 a month depending on the insulin.
Another reason for present higher costs is because brand names are coming off patent due to expiration. For example, the patent for Lantus came off patent in December, 2016. Patents for Humalog and Novolog, both rapid acting insulins, will expire soon too. These companies may keep present prices higher in anticipation of biosimilar insulins. A biosimilar insulin is made from the same protein structure and should have similar glucose lowering effects. Biosimilar insulins are subject to more stringent approval standards than small molecule regular generic drugs. Biosimilar insulins are more difficult to achieve a perfect copy than generic tablet drugs. The first biosimilar insulin called Abasaglar will be available in pen form around the end of December 2016. Everyone is interested in seeing how biosimilar insulins play out in terms of cost and effectiveness on blood sugars.
Hanie Redmond Pharmd Cde Bc
Without a doubt, insulin is lifesaving, and just a day or so without it will require hospitalization and could lead to death for those patients.
If someone has type 1 diabetes or if someone has had damage to their pancreas, these are instances where their body doesnt produce any insulin, Stephanie Redmond, PharmD, CDE, BC-ADM, founder of Diabetes Doctor, tells Verywell. Without a doubt, insulin is lifesaving, and just a day or so without it will require hospitalization and could lead to death for those patients.
Recommended Reading: How Does Glipizide Lower Blood Sugar
Reasons Why Insulin Is So Outrageously Expensive
20 Jan 2019, 6:08 p.m. in #insulin4all USA by T1International
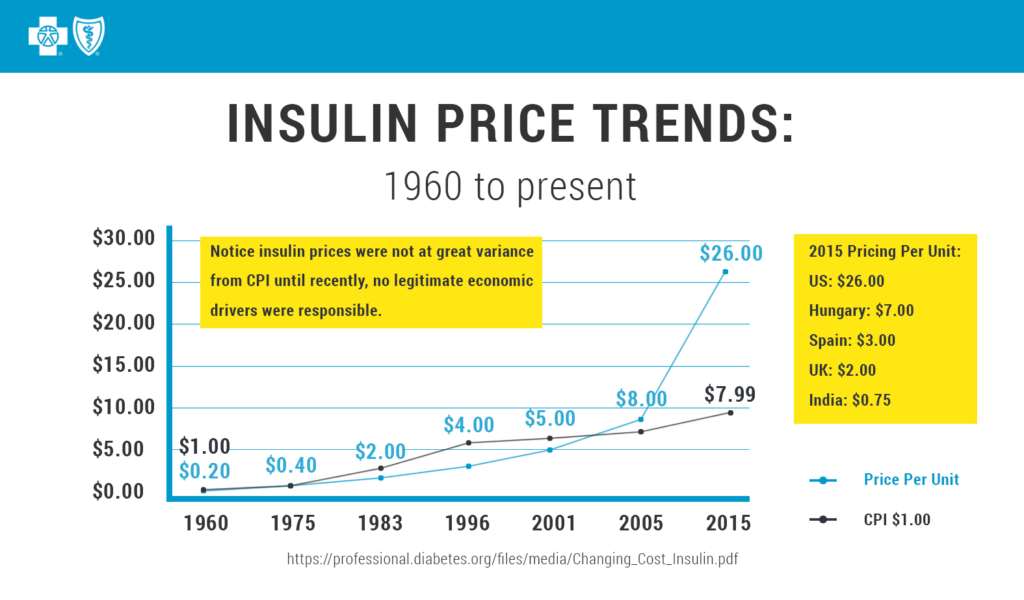
Why does insulin cost so much to patients in the USA and around the world? Why is insulin, a widely sold drug of which most forms are now off-patent, so incredibly expensive? These are simple questions, but ones with a number of complicated answers. This post will break some of those answers down and point you in the direction further reading if you want to dive deeper.
1. Only 3 Companies Control 90% of the Global Insulin Market
The big three insulin producers Eli Lilly, Novo Nordisk and Sanofi dominate more than 90% of the world insulin market by value. Often only one of these companies supplies insulin in a country, which means they more or less hold a monopoly there and can set prices as they wish. In some countries, notably China and India, there are domestic insulin companies that can help drive down the price. This means we need more companies in markets like the USA to help bring prices down. Well touch on that a bit further down the list.
2. No Generic Insulin
3.Pay-for-Delay Schemes & Lawsuits
4. Patents
5. Politics
6. Price Fixing
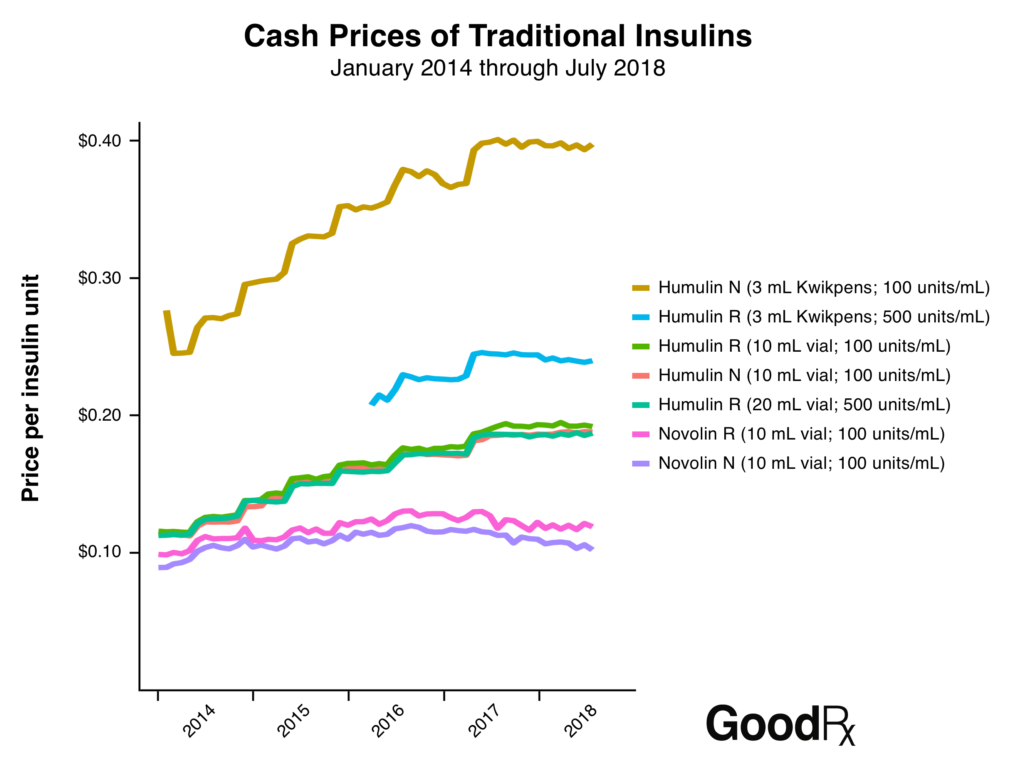
These Business Insider graphs pretty much say it all.
Several lawsuits alleging some form price-fixing are currently in the works. You can read more here and here.
7. Pharma Marketing Schemes
8. Payment for Influence
What Can be Done?
The Deadly Costs Of Insulin
In an era when healthcare is extremely expensive, there are many opinions on how involved our federal government should be in bringing drug prices down. However, there is one particular drug-pricing crisis that many can agree needs to be addressed sooner rather than later: the insulin crisis.
In an era when healthcare is extremely expensive, there are many opinions on how involved our federal government should be in bringing drug prices down. However, there is one particular drug-pricing crisis that many can agree needs to be addressed sooner rather than later: the insulin crisis.
For decades now, insulin prices have been soaring to new heights. Heights that the founders and creators of the drug, Frederick Banting and Charles H. Best, likely never imagined would be reached.
In his run for the presidency, President Donald Trump campaigned on the promise to lower the cost of overpriced prescription drugs. Since taking up his position in the Oval Office, Trump has been working to negotiate pricing with big-name pharmaceutical companies. Some of these companies have compromised under pressure and have agreed to lower drug costs.
Unfortunately, insulin is not one of the drugs that has seen any significant price reduction yet.
These proposals and others like them are coming about simply because the price of insulin doesnt make sense logically, financially, or morally.
Painting the Bigger Picture
How Does This Affect Medicare Beneficiaries?
Alec Raeshawn Smith
Recommended Reading: What Is A Normal A1c For A Non Diabetic
Policy Recommendations To Bring Down Insulin Prices
Reed and DeGette in the report recommended 11 policy proposals to address the rising cost of insulin:
- Allow generic drugmakers to manufacturer older, off-patent versions of insulin
- Cap out-of-pocket costs for prescription drugs designed to treat chronic conditions
- Encourage the development of generic insulin products by addressing extensions on patents
- Link a patient’s out-of-pocket costs to negotiated prices instead of list prices
- Promote the development and use of value-based contracts between insulin makers and PBMs
- Promote the use of standardized fees and other payment arrangements instead of rebates between insulin makers and wholesalers
- Restrict the number of changes an insurer can make to a formulary each year
- Require insulin makers, PBMs, and health insurers disclose the value of rebates to other entities in the insulin supply chain
- Require manufacturers disclose how they determine the list price of insulin products
- Standardize the process for patients to challenge formulary restrictions and
- Standardize a process for drug formularies to disclose patient cost-sharing information .
Robin Feldman Professor Of Law Uc Hastings College Of Law San Francisco
One would have to see how these orders were implemented to know how powerful and effective they will be.
We are still seeing many struggle in clinical practice with affordability, says Redmond. So it is unclear to most healthcare providers who gets these insulin cap benefits. Even myself as an expert would really love any more guidance on this. There are eligibility requirements that many patients still dont meet.
As with any legal order, the devil’s in the detail, Robin Feldman, Arthur J. Goldberg Distinguished Professor of Law at UC Hastings College of Law San Francisco, tells Verywell. One would have to see how these orders were implemented to know how powerful and effective they will be. We are, however, going to need some systemic changes to try to address the problems that are driving drug prices higher in general, and insulin prices higher specifically.
You May Like: Can Diabetics Eat Macaroni And Cheese
Will The Freeze Effect Medicares Insulin Discount
No. The Biden Administrations regulatory freeze does not impact a new insulin discount that took effect on January 1, 2021. That discount, announced last year by President Trump and CMS, allows seniors who sign up for an enhanced Medicare plan to receive a 30-day supply of insulin for $35. The discount requires seniors to join a Medicare drug plan or Medicare Advantage Plan that participates in the insulin savings model, so only those individuals who are willing to pay for the enhanced coverage are eligible to receive the $35 price cap.
We hope this information on if President Biden raise the cost of insulin is helpful. Stay on top of your health insurance by CALLING us at 410-1320
Your Worst Nightmareis That Your Child Is Going To Wind Up With The Same Horrible Illness
The skyrocketing prices for insulin don’t come as a surprise for Mandy Seaton.
The wife and mother who lives on Columbus’ North Side has battled Type 1 diabetes for almost 32 years, ever since spending a week in the hospital when she was 13.
A blood sugar reading of under 140 is considered normal. Hers was 980.
“I was very lucky I didnt go into diabetic ketoacidosis,” Seaton said, citing a sometimes-fatal condition caused by a severe lack of insulin.
Although dealing with a chronic condition is difficult, “its also taught me how to be really strong and have a lot of perseverance and tenacity. I just made up my mind that my diabetes is not going to stop me,” she said.
Seaton lived in South America for 10 months, ran a marathon and traveled to Mongolia.
She said her toughest struggle both physically and mentally came with her pregnancy and delivery of son Ronin, now 9.
“Your worst nightmare is that your child is going to wind up with the same horrible illness you have, the pre-school teacher said.
At first, Ronin had no problems. But when he was 4, his mother recognized the symptoms right away.
Now, mother and son often do their tests and treatments together. Due to recent strides in technology, she and her husband can monitor their son’s blood sugar via their smart phones, even when the third-grader returns to classes this week at Colerain Elementary School.
While things are OK now, Seaton realizes that “in an instant, it could change” if they lose health insurance.
You May Like: How Many Points Does Metformin Lower Blood Sugar
The Complicated World Of Insurance
When Marissa is on a Medicaid plan, she’s only allowed to renew her prescription a day or two before her insulin runs outand there have been times when renewing it on that timeline was impossible, such as when she had to travel out of state for a funeral. There are no accommodations made for people with diabetes experiencing any sort of hardship or emergency they have to be tied to the schedule of their insulin prescription, period.
Plus, if Marissa has to switch insurance plans, it can take awhile to get her prescription switched over. In those instances, she has to ration her supply of medication. How do you ration insulin? Simple, says Marissa: Just stop eating.
“If I don’t eat, there’s more insulin in my pump for other day-to-day activities,” she said. “Instead of eating breakfast, lunch and dinner, I’ll drink coffee for breakfast, eat a bar for lunch, and eat dinner.”
How do you ration insulin? Simple: Just stop eating.
For Marissa, rationing while using an insulin pump is less of a life-and-death scenario than rationing while taking insulin shots. “If you do shots, rationing means giving yourself less insulin than you actually need,” she said. Patients who ration with insulin shots are the ones who end up dying from related complications more often.
RELATED:10 Tips for Saving Money on Prescription Drugs
“With my current managed plan, I am allowed to get supplies for my current pump for free,” she said. “That just wouldn’t be feasible in Tennessee.”

