Did Steroids Bring On My Type 2 Diabetes
There has been debate as to whether corticosteroids are a cause for diabetes or whether steroids advance the development of existing type 2 diabetes
A study published in 2012, carried out by the University of Sydney, looked to investigate answers to the question.
The study, titled Steroid-Induced Diabetes: Is It Just Unmasking of Type 2 Diabetes? , found that those which developed new onset steroid induced diabetes had lower risk profiles than is typical of people with type 2 diabetes.
What To Do When You Stop Steroid Therapy
Its important to know what to do when you stop steroid therapy, to avoid negative health consequences, especially when managing diabetes.
Some strategies to help when stopping steroid therapy include:
- Work with your endocrinologist about tapering off the amount of insulin youre taking each day to reflect tapering down your steroid use
- Make sure you dont immediately stop taking your steroid therapy work with your prescribing physician to taper your medication. Abruptly stopping steroid therapy can make you very sick.
- Make sure you check your blood sugars more often than normal while tapering steroid therapy
- Carry extra low-snacks, as fluctuation in blood sugars is common while tapering other medications
- If your blood sugar remains high for more than 2 or 3 days after stopping steroid therapy, contact your doctor immediately
Molecular Basis Of Glucocorticoid Action On Glucose Regulation
The insulin-mediated pathways of glycogen synthesis and protein degradation and synthesis are directly influenced by glucocorticoids . Skeletal muscle is responsible for the majority of insulin-mediated glucose uptake. Insulin recruits GLUT4 glucose transporters to the cell surface enabling glucose uptake into cell. Glucocorticoids impair insulin-mediated glucose uptake by directly interfering with components of the insulin signalling cascade, such as glycogen synthase kinase-3, glycogen synthase and GLUT4 translocation . An increase in protein degradation and decrease in protein synthesis is due to glucocorticoid inhibition of post-insulin receptor cascades involving PKB/Akt and mTOR pathways.
Molecular basis of glucocorticoid action. See text for details. After van Raalte et al.
Don’t Miss: Prognosis Of Diabetes Type 1
How Can Diabetes Be Managed While On Steroids
Steroids are known to increase blood glucose levels and so one should avoid steroids whenever possible. But, certain therapies like chemotherapy and certain critical conditions demand the need of steroids therapy. While it is unavoidable to take these drugs in some cases, you can manage to control your blood sugar levels while on steroids in the following ways :
- Let your doctor be informed about the pre-diabetic condition, this could help prescribe different medications that do not interfere with blood glucose levels.
- Adjust the blood-glucose-lowering medications according to the timing, dosage of the steroids and its response observed in an individual.
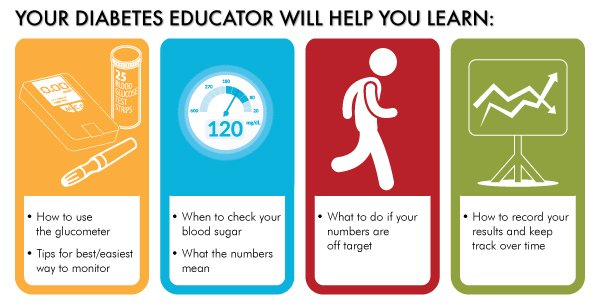
- Constant checking of your blood sugar level is advised.
- Your Diabetes specialist may advise an increase in your insulin intake depending on the blood glucose levels.
- Regular monitoring of urine and blood ketones is important to avoid severe complications.
- It is crucial to consult your doctor if the blood glucose levels are not getting stable despite an increase in insulin and oral medications.
- Maintain a healthy diet with low sugar intake with foods that help control your blood sugar levels while on steroids.
- Sometimes, the blood glucose levels can drop significantly, it is always advised to carry the juice, glucose tablets, a bar of chocolate, etc.
Tips For Diabetes Management While On Steroids
Both Scheiner and Bell say they find it surprising how few PWDs actually know about these steroid effects on glucose levels and how many healthcare professionals dont explain the likely effects to someone with diabetes before giving a steroid injection or prescription.
The advice that PWDs who might be taking steroids should be getting is pretty clear, per this Medical News Today report:
- Check blood glucose levels more often than usual. Experts recommend doing this four or more times a day.
- Work with your doctor to increase the dosage of insulin or oral D-medication, depending on blood sugar levels and other health considerations.
- Monitor urine or blood ketones to be sure BG levels arent approaching dangerously high.
- See a doctor immediately if BG levels do rise too high while taking steroids, and increased insulin or oral medication doses do not bring the levels down.
- As a person gradually reduces their dosage of steroids, they should also reduce the equivalent dosage of insulin or oral medication until it returns to the original dosage. It is important never to stop taking steroids suddenly, as this may cause severe illness.
- Carry glucose tablets, juice, or candy at all times, in case blood sugar levels drop suddenly from the additional D-medication being taken.
In addition to that textbook advice, Scheiner adds some practical tips:
Bell says dealing with these steroid-related BG rises usually means increasing short-acting insulin and/or insulin pump basal rates.
Recommended Reading: Metformin Blurred Vision
Dealing With Elevated Blood Glucose
For nondiabetics, acute hyperglycemia results from prednisone are usually mild, and blood glucose levels gradually return to normal once the drug is tapered off. If you chronically use prednisone at high dosages, you may develop steroid-induced diabetes, and your doctor will provide appropriate treatment. This may mean starting diabetes medications such as insulin. If you are diabetic previous to prednisone therapy, you doctor may increase your dosage of insulin. These decisions are dependent on your overall glucose control or A1C and blood glucose patterns. Check your blood glucose more frequently, about 4 to 6 times a day for several days, and discuss your glucose log with a certified diabetes educator or endocrinologist. Do the same while tapering off prednisone, since your blood glucose levels are likely to drop. Reducing diabetes medications may be necessary to prevent hypoglycemia.
How Is Steroid Induced Diabetes Treated
The treatment for diabetes you are put on may depend on the extent of insulin resistance and how high your blood glucose levels are. It may be possible to treat your diabetes with diet and physical activity but you may need oral anti-diabetic medication or insulin.
If you have been diagnosed with diabetes, you will need to attend health screenings at least once annually so your health can be monitored and treated appropriately.
Recommended Reading: Metformin Joint Pain Side Effects
Prednisone And Low Blood Pressure
If you are being weaned off of prednisone and are taking medications to help lower your blood pressure, be sure to discuss the effect the changes in prednisone could have on your blood pressure and monitor for the symptoms of low blood pressure.
Symptoms of low blood pressure can include:
- Dizziness or feeling lightheaded
- Blurred vision
Nasal Steroids And Blood Sugar
The side profile of oral steroids in extensive, especially when taken long term. In terms of blood sugar, they can increase levels by:
- Promoting gluconeogenesis .
- Reducing insulin sensitivity, decreasing glucose uptake into cells.
Nevertheless for nasal steroids, when taking into account the significantly different route of administration, doses used and bioavailability, they are not thought to cause significant side effects in most individuals.
In regard to blood sugar levels specifically, one study that looked at budesonide noted no suppression of cortisol and no increase in blood sugars. Another noted no significant systemic side effects whatsoever.
However, one study noted that while most intranasal steroids didn’t increase blood sugar levels or A1c, triamcinolone did :
References
Read Also: Articles About Diabetes Mellitus
Signs And Symptoms Of Steroid
If your blood sugar levels are only slightly higher than usual, you may not have any of the symptoms of steroid-induced diabetes at all. But as your blood sugar levels rise, signs and symptoms may include:
- going to the toilet a lot, especially at night
- feeling really thirsty
- feeling more tired than usual
- losing weight without trying to.
Your doctor might ask you to check your blood sugar levels while on steroids. If you notice any of these symptoms, its important to let your GP know.
Risk Factors Of Steroid
There are some factors that may mean you are more likely to develop diabetes if you are taking steroids. These include if you:
- are over 40 and white, or over 25 and African-Caribbean, Black African or South Asian
- have a close family member with type 2 diabetes
- are of African-Caribbean, Black African or South Asian descent
- have had high blood pressure
- are living with obesity.
Weve got lots more information about the different diabetes risk factors. If you are taking steroids as part of your treatment for a health condition, or if you are about to start, use our Know Your Risk tool to find out your risk of developing diabetes.
Recommended Reading: Metformin Low Blood Sugar
Will Prednisone Raise Blood Pressure
Prednisone raises blood pressure in many people who take it. One reason is that prednisone and other corticosteroids cause the body to retain fluid. Extra fluid in the circulation can cause an increase in blood pressure. Anyone who takes prednisone should have his or her blood pressure monitored regularly.
How Do Oral Steroids Affect My Glucose Levels
Individuals who find themselves taking oral steroids like predisone for a medical condition are likely to see their blood sugar go haywire while on the medication. There are many different ways of getting steroids in the body, like oral , inhaled, liquid drops , topical , and intravenous. Depending on the condition, a particular route may be favored over another. For a poison ivy rash, a cream might be ideal. For severe asthma, inhaled or intravenous might. For chronic sinusitis, oral pills may be prescribed. For styes, a eyedropper liquid form might be used. Oral and intravenous are the mostly likely to have a significant effect on glucose levels and metabolism.
Steroids are generally prescribed for their anti-inflammatory and immune suppressing properties, but have several side effects, of which one of the most severe is hyperglycemia .
One of our founders who normally has extremely stable glucose levels had to take a week of prednisone for a respiratory illness. His normal flat line glucose went from this:
Stable, low glucose levels in the 60-70 mg/dL range
to this:
Highly erratic glucose with large swings up to 150 mg/dL
Exaggerated elevation of glucose with slow return to normal
Oral steroids affect glucose regulation through a number of different mechanisms, all of which can lead to increased glucose levels in the blood. Here are some of the main causes:
You May Like: Hypoglycemia Induced Hypertension
Prednisone And Blood Pressure
A reported side effect of prednisone is increased blood pressure. Two reasons prednisone can increase blood pressure is the drugs impact on fluid balance and weight.
When taking prednisone, the body holds on to sodium and loses potassium. This change in electrolyte balance causes:
- Fluid retention
- Weight gain
- Bloating
When you are retaining water, it increases the total volume of fluid that is being pushed through your blood vessels by your heart and this can cause increases in your blood pressure.
Another way that prednisone can increase blood pressure is weight gain. Corticosteroids increase your appetite and changes your bodys response to both insulin and sugar. An increased appetite leads to excess calorie intake and as a result weight gain.
Research has shown that people who are obese have a five times higher risk of developing high blood pressure. Studies have also found that a weight loss of just 10%, for those who are overweight or obese, significantly lowered their risk of developing high blood pressure.
How Do Steroid Medications Affect Blood Glucose Levels
If you have diabetes and are taking steroid medication, your blood glucose levels are likely to increase. Steroid medications can raise blood glucose levels by reducing the action of insulin and making the liver release stored glucose into the bloodstream.
The timeframe in which these medications begin to affect your blood glucose levels can vary depending on how you are taking them.
- Oral steroids: Blood glucose levels may begin to rise within a few days of starting oral steroids. Their effect on blood glucose levels will depend on the time, dose and type of steroid you are taking.
- Steroid injections: Blood glucose levels may rise soon after the injection and may remain high for 3-10 days afterwards.
Creams used for skin conditions, and inhaled steroids used for asthma and ear and eye drops are unlikely to affect blood glucose levels.
If you need to take steroid medication, talk to your doctor about how it may affect your blood glucose levels and ask for advice on how to manage this. Ask your doctor or pharmacist for an information sheet about this medication.
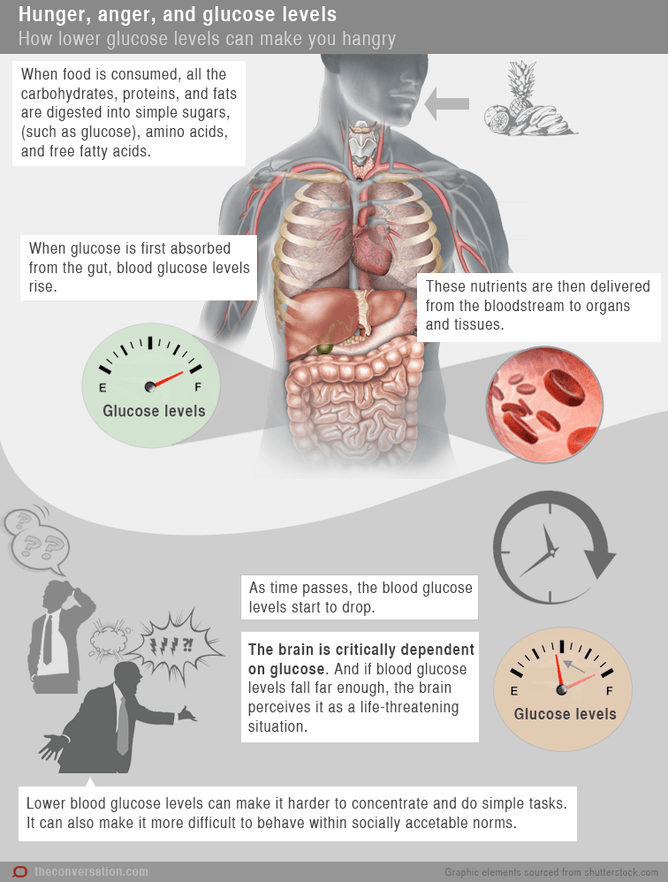
High blood glucose levels can make you feel unwell, tired or lacking in energy, and thirsty. It can also make you pass urine more often.
Seek advice from your doctor or a credentialled diabetes educator on monitoring your blood glucose levels while taking steroid medication.
If you are taking steroid medication, talk to your doctor about how this may affect your blood glucose levels.
Recommended Reading: Is Metformin Bad For Your Heart
Effects Of Steroids On Diabetes
Corticosteroids tend to drive blood sugars higher, sometimes much higher. Wil Dubois, a diabetes expert and blogger with type 1 diabetes, reports taking prednisone for muscle spasms: I took my first pill at a blood sugar of 96 mg/dL. An hour later I was at 552 mg/dL. I ran my insulin pump dry fighting the blood sugar. My insulin might as well have been water.
According to Medtronics Diabetes Clinical Manager Beth Spencer Kline, MSN NP-C, CDE, steroids increase the livers release of glucose and cause insulin resistance, which lead to insulin working less efficiently.
According to diabetes.co.uk, high blood sugars usually go back down when steroids are stopped, but long-term use can cause permanent problems and even drive a person with prediabetes into type 2. This is true of oral, injectable, and topical steroids.
How Steroids Affect Blood Sugar
Steroids mimic cortisol, which is a stress hormone. Cortisol raises blood sugar and blood pressure.
Steroids can make the body more insulin-resistant over time. This means that cells dont respond to the hormone insulin the way they should, or the body isnt making enough insulin.
As a result, insulin resistance can occur, as the liver is releasing too much sugar, making the pancreas release more insulin to compensate. Over time, this can cause the pancreas to stop producing insulin, resulting in high blood sugar.
If steroids arent taken for a long time, then blood sugars can return to normal once the steroids are discontinued. However, for people taking steroids long-term, the risk of insulin resistance increases.
For those with diabetes, blood sugars often noticeably increase after steroids are administered. Those without diabetes may be unaware that their blood sugars are elevated since they dont typically check their blood sugar levels.
Recommended Reading: Metformin And Insulin Combination Therapy
Preventing High Blood Pressure
If you are already taking blood pressure medications when you began taking prednisone, your healthcare provider may adjust these medications. They may just recommend monitoring your blood pressure to assess how your body is responding to prednisone.
If you develop high blood pressure while taking prednisone, your healthcare provider may recommend starting blood pressure medication to help.
Lifestyle changes can be implemented to help prevent high blood pressure. Eating a balanced diet of fruits, vegetables, whole grains, and healthy fats can help with maintaining a health weight.
It also helps to limit the total amount of salt in your diet. It is recommended to limit your salt intake 2 grams or 2000 milligrams sodium per day. This includes the sodium that naturally occurs in food, salt added during processing, and any salt you add to your foods.
Try these tips to help reduce your overall salt intake:
- Keep saltshakers off of the table and avoid adding salt after you’re done cooking.
- Cook with other herbs and spices that don’t have salt added to them, such as black pepper, oregano, cumin, onion powder, garlic powder, and any spice blend without sodium.
- When purchasing canned or processed foods, choose those labeled low sodium or no salt added.
- Read the label to see how many milligrams of sodium it has per serving and the serving size.
- Rinse can foods to help remove a lot of the extra salt that is added during processes to help preserve the food.
Steroid Medications And Diabetes Fact Sheet
This fact sheet is available in two formats.
You can download and print out the PDF version.
Or you can read it as a website page below.
Some people with diabetes may need to take steroid medications to help manage other conditions, such as asthma, arthritis, autoimmune diseases and dermatitis, or as part of chemotherapy.
Steroid medications reduce pain and inflammation, and they can also be used to prevent nausea during medical procedures .
Your body produces steroid hormones to help it fight stress, injury and disease. Steroid medications have a similar effect to the hormones produced by the body. There are many different types of steroid medications, including cortisone, hydrocortisone, prednisolone, prednisone and dexamethasone.
Steroid medications can be taken in various ways, including:
- orally
- with an inhaler
- as drops for eyes or ears
- as a cream applied to the skin.
Also Check: Does High Blood Sugar Mean You Have Diabetes
Other Stories Of Prednisone And Diabetes:
Joe also experienced a critical blood sugar level after taking prednisone:
As a child I was diagnosed with an autoimmune condition called dermatomyositis. Growing up I had periodic treatment with prednisone.
When I was 27 I was on a 2 week course of prednisone . Then my doctor called me himself and told me to go straight to the hospital since my blood glucose was 740. I have not been on prednisone since.
As I got older I had minimal problems with the dermatomyositis. But in the last 5 years my diabetes has been out of control and considered very brittle. My doctor has had to change my insulin type four times in the last nine months. I feel most of my problems are the result of my long time use of prednisone.
Cheri had her type 2 diabetes go critical after a big dose of prednisone!
I had to go to the ER today for a severe allergic reaction. They hooked me up to the IV within 5 minutes of me walking in and they gave me a few meds into the IV including 120 mg of prednisone. The doctor sent me home with a prescription of prednisone . I was to take 3 pills once a day for 5 days. He did say it would affect my type 2 diabetes, but WOW he never said it would go to 499 tonight!
Miriam shares her experience with prednisone and diabetes:

