Can Improve Patients Daily Lives
Our findings might mean that insulin production can be partially restored if we can find a way of stopping the disease process. The potential for insulin production is greater than previously thought. The risk of developing health problems later on is lower for those who manage to maintain a certain level of insulin production. Less supplementary insulin means that you will be better off as a patient, says Krogvold.
Insulin And The Circulatory System
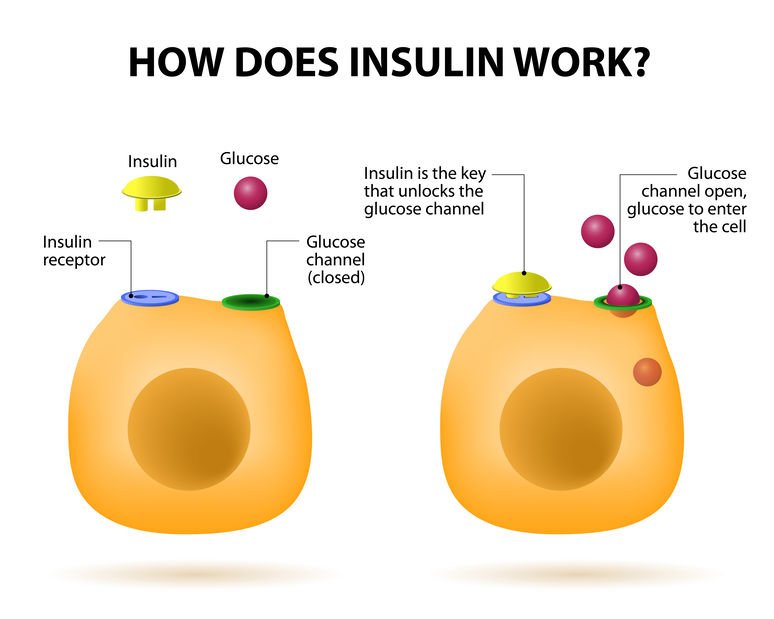
Insulin is secreted into the bloodstream and helps the cells of the body make use of glucose. It is the responsibility of the circulatory system to provide the insulin for all the cells of the body. As long as enough insulin is produced by the body, the glucose is able to be used and the cells of the body thrive.
If there isnt enough insulin in the circulatory system, glucose levels go up and there can be complications, such as diabetic nephropathy , diabetic retinopathy , diabetic neuropathy , and heart disease.
A lack of insulin in the bloodstream results in starvation of the cells. As the cells cant make use of glucose, they start to break down fat to be used as cellular fuel. If glucose in the bloodstream becomes extremely high, ketones can build up in the body. Ketones are the metabolic byproduct of other sources of fuel the body is using. When ketones build up, there can be obvious symptoms, such as a dry mouth, nausea, vomiting, and a sweetness in the breath. When this happens, it is called diabetic ketoacidosis.
Synthesis And Release Of Insulin
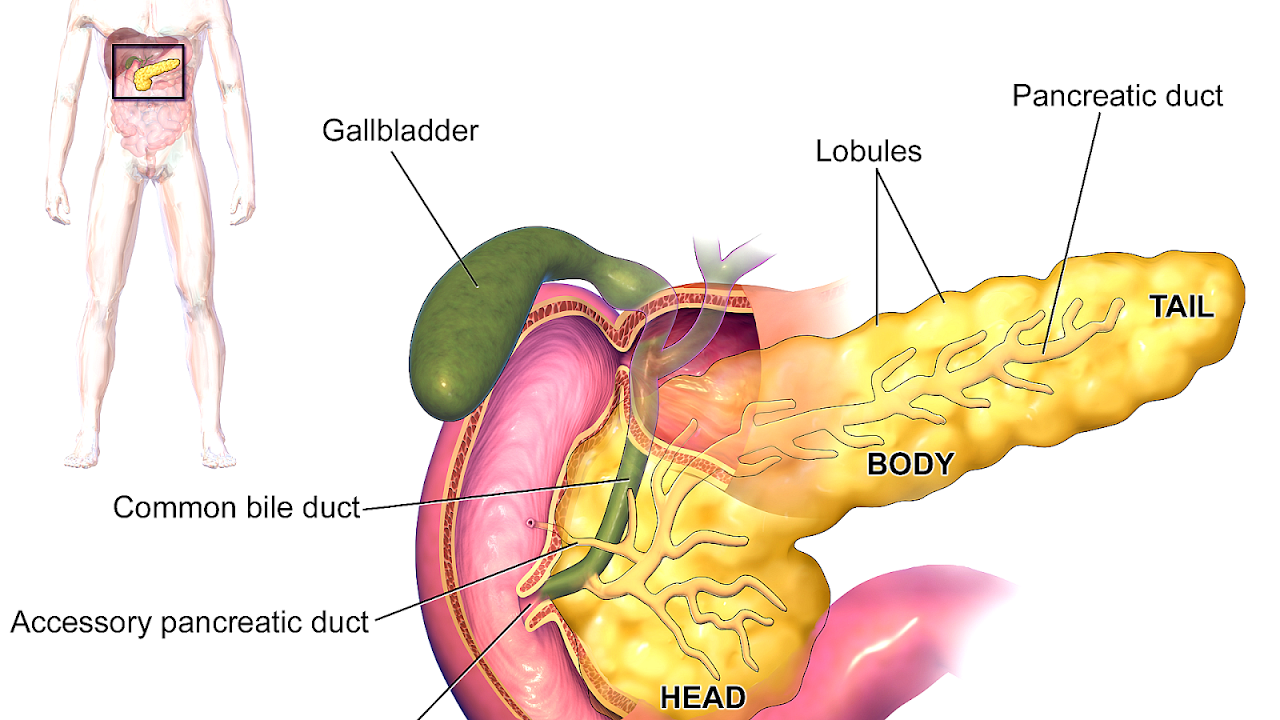
Insulin is coded on the short arm of chromosome 11 and synthesised in the cells of the pancreatic islets of Langherhans as its precursor, proinsulin. Proinsulin is synthesised in the ribosomes of the rough endoplasmic reticulum from mRNA as pre-proinsulin. Pre-proinsulin is formed by sequential synthesis of a signal peptide, the B chain, the connecting peptide and then the A chain comprising a single chain of 100 amino acids. Removal of the signal peptide forms proinsulin, which acquires its characteristic 3 dimensional structure in the endoplasmic reticulum. Secretory vesicles transfer proinsulin from the RER to the Golgi apparatus, whose aqueous zinc and calcium rich environment favours formation of soluble zinc-containing proinsulin hexamers. As immature storage vesicles form from the Golgi, enzymes acting outside the Golgi convert proinsulin to insulin and C-peptide. Insulin forms zinc-containing hexamers which are insoluble, precipitating as chemically stable crystals at pH 5.5. When mature granules are secreted into the circulation by exocytosis, insulin, and an equimolar ratio of C-peptide are released. Proinsulin and zinc typically comprise no more than 6% of the islet cell secretion.
You May Like: Glucotrol Vs Metformin
Yeast Expression System For The Production Of Insulin
Yeast is a preferred host for expression of various heterologous proteins that require post-translational modifications for its biological activity. Yeast cell has the ability to carry out numerous post-translational modifications such as phosphorylation, O-linked glycosylation, N-linked glycosylation, acetylation and acylation. Recombinant proteins are expressed in soluble form in yeast and properly folded in functionally active form. Production of biopharmaceuticals using yeast expression system is also very cost effective and is amenable to scale up using large bioreactors. However, one major concern for producing therapeutic glycoprotein for human application is that yeast N-glycosylation is of the high-mannose type, which confers a short half-life in vivo and hyperâimmunogenicity and thus render the therapeutic glycoprotein less effective. Various attempts have been made to humanize yeast N-glycosylation pathways in order to produce therapeutic glycoproteins with humanized N-glycosylation structure .
Insulin Receptors And Insulin Binding
Insulin mediates its actions through binding to insulin receptors. The insulin receptor was first characterised in 1971. It consists of a heterotetramer consisting of 2 and 2 glycoprotein subunits linked by disulphide bonds and is located on the cell membrane. The gene coding for the insulin receptor is located on the short arm of chromosome 19. Insulin binds to the extracellular subunit, resulting in conformational change enabling ATP to bind to the intracellular component of the subunit. ATP binding in turn triggers phosphorylation of the subunit conferring tyrosine kinase activity. This enables tyrosine phosphorylation of intracellular substrate proteins known as insulin responsive substrates . The IRS can then bind other signalling molecules which mediate further cellular actions of insulin.
PI 3-kinase promotes the translocation of glucose transporter proteins, glycogen, lipid and protein synthesis, anti-lipolysis and the control of hepatic gluconeogenesis. PI 3-kinase acts via serine and threonine kinases such as Akt/protein kinase B , protein kinase C and PI dependent protein kinases1& 2 . The RAS pathway activates transcription factors and stimulates the growth promoting actions of insulin. Thus broadly, PI 3-kinase mediates insulins metabolic effects, e.g. cellular glucose uptake, while RAS significantly mediates insulins mitogenic effects, together with other less well described actions. These pathways are presented schematically in .
Recommended Reading: How Long Does Metformin Er Stay In Your System
When To Contact A Medical Professional
- Chest pain or pressure, shortness of breath, or other signs of angina
- Loss of consciousness
Also call your provider if you have:
- Blood sugar levels that are higher than the goals you and your provider have set
- Numbness, tingling, or pain in your feet or legs
- Problems with your eyesight
- Sores or infections on your feet
- Frequent feelings of depression or anxiety
- Symptoms that your blood sugar is getting too low
- Symptoms that your blood sugar is too high
- Blood sugar readings that are below 70 mg/dL
You can treat early signs of hypoglycemia at home by drinking orange juice, eating sugar or candy, or by taking glucose tablets. If signs of hypoglycemia continue or your blood glucose level stays below 60 mg/dL , go to the emergency room.
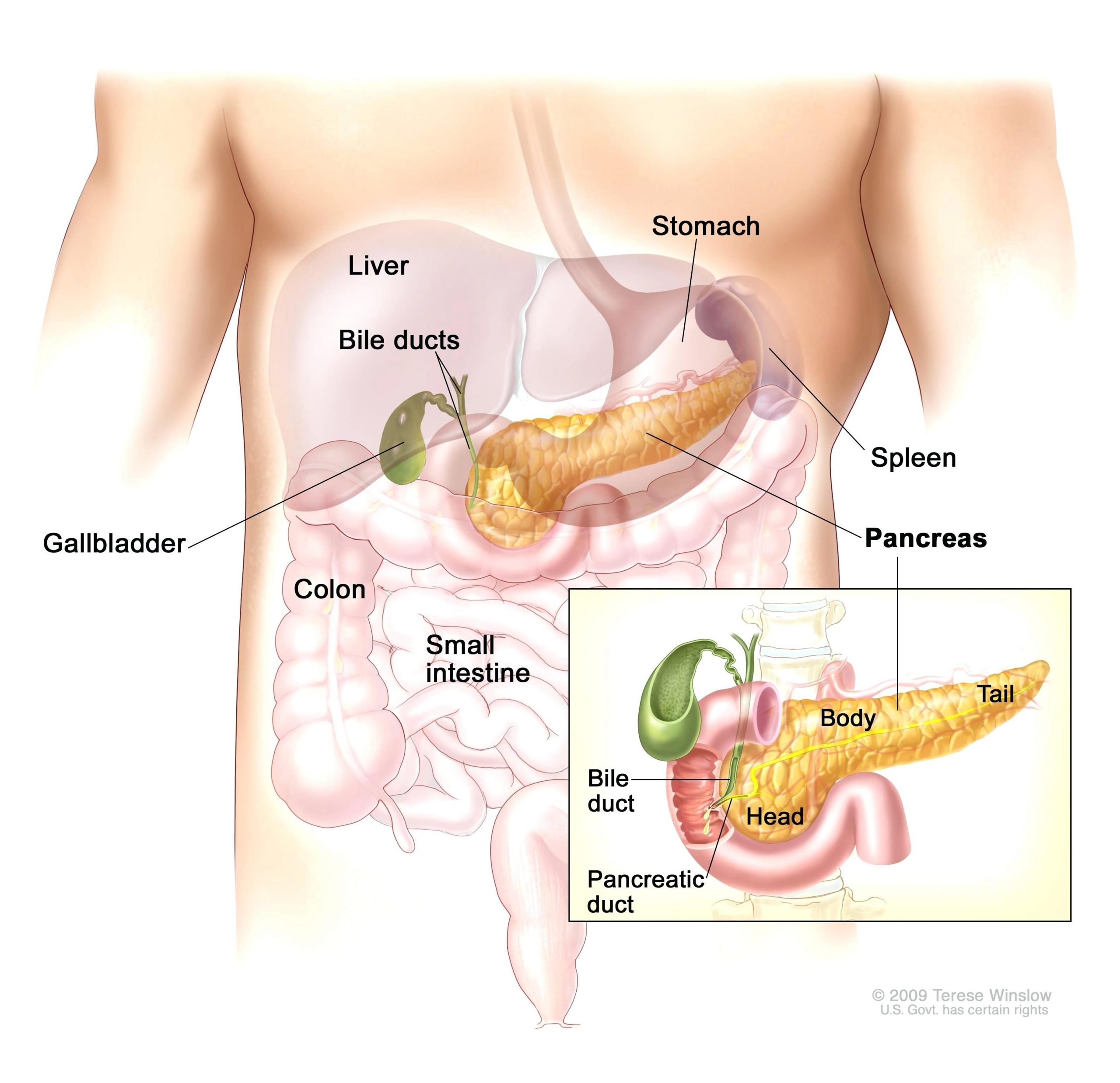
Produced In The Pancreas
When you eat, food travels to your stomach and small intestines, where its broken down into nutrients that include glucose. The nutrients are absorbed and distributed via your bloodstream.
The pancreas is a gland located behind your stomach that performs an essential role in the digestion process. It creates enzymes that break down the fat, starches, and sugar in the food. It also secretes insulin and other hormones into your bloodstream.
Insulin is created in the beta cells of the pancreas. Beta cells comprise about 75% of pancreatic hormone cells.
Other hormones produced by the pancreas are:
- glucagon, which alerts your liver to raise your blood sugar if it gets too low
- gastrin, which stimulates the production of gastric acid in your stomach
- amylin, which helps control your appetite
You May Like: Metformin Food Interactions
Pharmacological Influences On Insulin Action And Insulin Resistance
A wide range of pharmacological agents have been associated with impaired glucose tolerance. Antihypertensive agents such as diuretics and -blockers, corticosteroids, oral contraceptives, nicotinic acid and antipsychotic agents have been reported to impair glucose tolerance, as have the anti-retroviral protease inhibitors used to treat human immunodeficiency virus infection. The mechanisms vary -blockers impair insulin secretion from the pancreas by blockade of -adrenoceptors, thiazide diuretics are thought to act by depleting potassium levels, corticosteroids and oral contraceptives have counter-regulatory hormonal activity, and the HIV-1 protease inhibitors result in partial lipodystrophy with loss of peripheral subcutaneous fat and accumulation of truncal adipose tissue leading to insulin resistance.
Can Your Body Produce Too Much Insulin
Tumors of the pancreas that produce too much insulin are called insulinomas. Insulinomas keep making insulin, and can make your blood sugar drops too low . A high blood insulin level causes a low blood sugar level . Most insulinomas are non-cancerous tumors.
Is 30 units of insulin a lot?
Generally, to correct a high blood sugar, one unit of insulin is needed to drop the blood glucose by 50 mg/dl. This drop in blood sugar can range from 30-100 mg/dl or more, depending on individual insulin sensitivities, and other circumstances.
Also Check: Is Diabetes Type 2 Hereditary
Vi Regulation Of Insulin Release
Insulin release from pancreatic b cells is tightly regulated, and allows the sensitive response of insulin levels to calorigenic nutrients in the body. Glucose, free fatty acids, and amino acids serve as fuel stimuli for insulin release, promoting insulin granule exocytosis. Additional hormonal factors influence the regulation pathway. Pharmacological agents can also be used to augment insulin release.
A. Glucose-stimulated insulin secretion
Figure 5. Hyperglycemic clamp illustration. Example of hyperglycemic clamp testing in obese adolescents with normal glucose tolerance , impaired glucose tolerance , and type 2 diabetes . In the hyperglycemic clamp in healthy, non-diabetic individuals, glucose concentration is briskly elevated by administering a suitable intravenous glucose infusion at time 0. This elicits a rapid and short-lived insulin secretion peak due to release of preformed insulin vesicles, followed by a drop towards basal levels and then by a relatively rapid return to a sustained increase in insulin in the second half of the clamp as dextrose infusion is continued. This example illustrates the loss, in first and second phase insulin secretion, as individual progress from normal to impaired glucose tolerance, to type 2 diabetes. In the latter, the first phase insulin response is essentially lost and the second phase insulin response is reduced. ).
B. Proteins and Amino Acids
C. Lipids and Free Fatty Acids
D. Incretin Hormones
When The Blood Glucose Level Goes Up
- Blood sugar rises
- The pancreas detects the rise
- The pancreas pumps out insulin into the blood
- Insulin helps the uptake of glucose into muscles and other cells
- This causes the blood glucose level to fall to its normal set point and
- The pancreas detects the fall and switches off insulin production.
Also Check: Side Effects From Insulin
Who Gets Type 2 Diabetes
What makes people more likely to develop type 2 diabetes? No one knows for sure. But experts have a few ideas about what puts a person at greater risk:
- Most people who have type 2 diabetes are overweight.
- People with family members who have diabetes get diabetes more often.
- People who are older than 10 are more likely to develop type 2 diabetes than younger kids.
Insulin And Type 1 Diabetes
In type 1 diabetes, the body produces insufficient insulin to regulate blood glucose levels.
Without the presence of insulin, many of the bodys cells cannot take glucose from the blood and therefore the body uses other sources of energy.
Ketones are produced by the liver as an alternative source of energy, however, high levels of the ketones can lead to a dangerous condition called ketoacidosis.
People with type 1 diabetes will need to inject insulin to compensate for their bodys lack of insulin.
Recommended Reading: Is It Safe For A Diabetic To Get A Tattoo
Enhancing Healthcare Team Outcomes
Insulin is a widely used medicine in hospital settings for the management of hyperglycemia. Insulin is regarded as a high alert medication as its misuse is associated with significant risks such as hypoglycemia, and medical errors are common when using it in hospitals. Deal et al. found that most commonly reported errors were related to missed doses of insulin , timing errors , and missed documentation of doses . These problems reveal several system errors that merit attention. Rousseau et al. identified various problems causing errors in the hospital use of insulin such as frequent staff turnover, the involvement of various healthcare providers, none of which are specifically responsible for overall glycemic management, lack of perception of insulin as a high alert medication, rapidly evolving diabetes management and lack of education of staff on insulin management. To minimize these errors following measures should be undertaken,
- Availability of standardized protocols
- Communication between nurses on different shifts
- Adequate communication between nurses, physicians, and pharmacists
- Training professionals in insulin therapy of inpatients
Insulin Secretion In Response To Stimuli
Response to Glucose
In healthy individuals glucose stimulated pancreatic secretion is biphasic. Intravenous administration of glucose is associated with a rapid first phase of insulin release within 1 minute, peaking at 35 minutes, and lasting about 10 minutes the slower onset second phase of insulin secretion begins shortly after the glucose bolus but is not apparent until 10 minutes later, lasts the duration of the hyperglycaemia and is proportional to the glucose concentration immediately prior to the glucose administration. The first phase of insulin secretion represents release of insulin already synthesised and stored in secretory granules the second phase represents secretion of both stored and newly synthesised insulin. Overall insulin secretion relates to the total dose of glucose and its rate of administration maximal pancreatic response occurs with 20 g of glucose given intravenously over 3 minutes in humans.
In contrast to the reproducible pattern of insulin secretion in response to intravenous glucose, insulin secretion following oral glucose is much more variable. With an oral glucose load, gastric emptying and gastrointestinal motility affect glucose absorption, gastro-intestinal hormones and neural input associated with glucose ingestion modify the insulin response, and insulin secretion continues some time after glucose ingestion.
Response to Arginine
Effects of Lipids
Response to Mixed Meal
Incretin Hormones
Effects of Neural and Hormonal Stimuli
You May Like: What Percentage Of Type 2 Diabetics Take Insulin
V Insulin Secretory Pathway
The pancreatic b-cells act as a self-contained system to secrete insulin in response to changes in ambient blood glucose concentration, in order to maintain glucose homeostasis. Glucose is freely taken up into the b-cell via GLUT transporters, metabolized to produce ATP, which triggers a cascade of signals within the b cell necessary for glucose-induced insulin secretion. While GLUT2 has been traditionally assumed as the major mediator of glucose uptake into b-cells based on extrapolation from rodent studies and subsequent confirmation of GLUT2 transporters on human -cells , more recent studies in human islets suggest that the other insulin-independent glucose transporters GLUT1 and GLUT3 play a more important role, and are the main glucose transporters in human islet -cells . This redundancy explains why individuals with variants in the gene encoding GLUT2 do not have significant abnormalities in insulin secretion .
Figure 4. Diagrammatic illustration of insulin secretion. A low background secretion exists upon which is superimposed insulin secretory bursts stimulated by food intake. ).
Insulin And Blood Glucose Levels
Insulin helps control blood glucose levels by signaling the liver and muscle and fat cells to take in glucose from the blood. Insulin therefore helps cells to take in glucose to be used for energy.
If the body has sufficient energy, insulin signals the liver to take up glucose and store it as glycogen.
The liver can store up to around 5% of its mass as glycogen.
Some cells in the body can take glucose from the blood without insulin, but most cells do require insulin to be present.
Read Also: How Do I Know If My Blood Sugar Is High
Production Of Hormones To Control Blood Sugar Levels
A small proportion of the pancreas is made up of other types of cells called islets of Langerhans. These cells sit in tiny groups, like small islands, scattered throughout the tissue of the pancreas. The islets of Langerhans contain alpha cells which secrete glucagon and beta cells which secrete insulin.
Insulin and glucagon are hormones that work to regulate the level of sugar in the body to keep it within a healthy range. Unlike the acinar cells, the islets of Langerhans do not have ducts and secrete insulin and glucagon directly into the bloodstream.
Depending on what youve eaten, how much exercise your muscles are doing, and how active your body cells are, the amount of glucose in your bloodstream and cells varies. These 2 hormones have the job of keeping tight control of the amount of glucose in your blood so that it doesnt rise or fall outside of healthy limits.
Diabetics Need Insulin Therapy Because They Can’t Make Their Own
Insulin therapy tries to mimic natural insulin secretion what happens automatically in non-diabetics.
The ultimate goal of insulin therapy is to mimic normal insulin levels. Unfortunately, current insulin replacement therapy can only approximate normal insulin levels. Insulin therapy for type 2 diabetes ranges from one injection a day to multiple injections and using an insulin pump . The more frequent the insulin injections, the better the approximation of natural or normal insulin levels. Discuss with your medical provider the insulin regimen that is best for you.
You May Like: Do Type 1 Diabetics Take Insulin
What Happens If I Have Too Little Insulin
People with diabetes have problems either making insulin, how that insulin works or both. The main two types of diabetes are type 1 and type 2 diabetes, although there are other more uncommon types.
People with type 1 diabetes produce very little or no insulin at all. This condition is caused when the beta cells that make insulin have been destroyed by antibodies , hence they are unable to produce insulin. With too little insulin, the body can no longer move glucose from the blood into the cells, causing high blood glucose levels. If the glucose level is high enough, excess glucose spills into the urine. This drags extra water into the urine causing more frequent urination and thirst. This leads to dehydration, which can cause confusion. In addition, with too little insulin, the cells cannot take in glucose for energy and other sources of energy are needed to provide this energy. This makes the body tired and can cause weight loss. If this continues, patients can become very ill. This is because the body attempts to make new energy from fat and causes acids to be produced as waste products. Ultimately, this can lead to coma and death if medical attention is not sought. People with type 1 diabetes will need to inject insulin in order to survive.
The Insulin Resistance Syndrome
The insulin resistance syndrome describes the cluster of abnormalities which occur more frequently in insulin resistant individuals. These include glucose intolerance, dyslipidaemia, endothelial dysfunction and elevated procoagulant factors, haemodynamic changes, elevated inflammatory markers, abnormal uric acid metabolism, increased ovarian testosterone secretion and sleep-disordered breathing. Clinical syndromes associated with insulin resistance include type 2 diabetes, cardiovascular disease, essential hypertension, polycystic ovary syndrome, non-alcoholic fatty liver disease, certain forms of cancer and sleep apnoea.
Also Check: Does Black Coffee Affect Blood Sugar

