Does Insulin Increase Blood Glucose
Insulin is the hormone that is responsible for breaking down glucose and turning it into energy. It helps glucose to enter into cells. Thus, it maintains a normal blood sugar level when there is a surge of glucose in the blood after having food.
So, instead of letting the blood sugar level rise, Insulin actually decreases the blood sugar level. However, if you are someone who is suffering from diabetes then an exceptional scenario needs to be considered. You might be someone who has been prescribed to inject insulin.
For some reason, you might accidentally inject less amount of insulin compared to the prescribed dosage. This will lead to raised blood sugar as the small amount of insulin that was administered wont be able to tackle the surge of glucose.
The hormone that is mainly responsible for increasing blood sugar is Glucagon. It breaks down the glucose storage and brings glucose to the bloodstream resulting in a rise in blood glucose.
Some Side Effects Can Be Serious If You Experience Any Of The Following Symptoms Call Your Doctor Immediately:
- rash and/or itching over the whole body
- shortness of breath
- large weight gain in a short period of time
- swelling of the arms, hands, feet, ankles, or lower legs
If you experience a serious side effect, you or your doctor may send a report to the Food and Drug Administration’s MedWatch Adverse Event Reporting program online or by phone .
Insulin And Glucose Concentrations
Insulin is responsible for regulating the glucose concentration inside the bloodstream. There is a direct relationship between glucose and insulin. As the glucose level falls, the insulin level also falls so that the individual doesnt get hypoglycemia. As the glucose level rises, so does the insulin level. In this way, the insulin can start to act to decrease the glucose concentrations in the bloodstream.
Read Also: Does Metformin Cause Stomach Pain
What Do The Test Results Also Tell Me About Isf
As explained above, Duration of Insulin Action is a measure of how long insulin continues to lower BG, while Insulin Sensitivity Factor is a measure of how much the BG is lowered .
In analyzing the test results above, it is important to note: if your childs target BG during this time is 7.0 mmol/L, then this correction dose of insulin did not reduce BG enough , as the lowest BG was 9.5 mmol/L, which is above target. This is related to the ISF setting it is NOT related to the IOB setting.
However, if your childs target BG during this time period is 9.5 , then the insulin dose given worked to lower BG to the target, thus this test would have verified the current ISF setting.
Fatty Acids And Insulin Resistance
In both obesity and type 2 diabetes, plasma FFA levels are elevated. Increasingly, there is evidence to support the contention that FFAs affect insulin action at the peripheral target tissues. The exact site of inhibition of insulin action has not yet been well defined however, FFA-induced defects at the level of glucose uptake into muscle, phosphorylation of glucose by glucose-6-phosphate, and glycogen synthesis have been demonstrated . It has been further proposed that the mechanisms by which TNF- and leptin cause insulin resistance, and whereby the TZDs improve insulin sensitivity, may be triggered indirectly, via a reduction in FFAs levels .
You May Like: Is Metformin Bad
Functional Measures Of Insulin Resistance
Another approach is to identify insulin resistant patients, based on functional markers of insulin resistance. McLoughlin et al were able to identify insulin resistant individuals from an overweight-obese cohort by looking at plasma triglyceride concentration, ratio of triglyceride to high-density lipoprotein cholesterol concentrations and insulin concentration. Using cut points of 1.47 mmol/L for triglyceride, 1.8 mmol/L for the triglyceride-high-density lipoprotein cholesterol ratio and 109 pmol/L for insulin, they achieved comparable sensitivity and specificity to the Adult Treatment Panel III to diagnose the metabolic syndrome.
Types Of Insulin Administration With Needles Pumps Pens And Why Insulin Is So Expensive
What does insulin do? Help your body turn food into energy, for starters. When you have diabetes, and youre either not producing insulin or your insulin function is off, all sorts of things can go wrong. From needles to pens to pumps to types of insulin, were here to empower you with clear answers to all your pressing questions.
In This Article:
Alvin Powers, MD, Mihail Zilbermint, MD, and Irl Hirsch, MD
Also Check: Type 1 Diabetes Too Much Insulin
Insulin And Type 2 Diabetes
Type 2 diabetes is characterised by the body not responding effectively to insulin. This is termed insulin resistance. As a result the body is less able to take up glucose from the blood. In the earlier stages of type 2 diabetes, the body responds by producing more insulin than it would normally need to.
If type 2 diabetes develops over a number of years, the extra demands on the pancreas to produce insulin can lead to a loss of insulin producing cells as they wear out.
Depending on their level of insulin resistance, people with type 2 diabetes may also need to take insulin injections to manage their blood sugar levels.
Insulin And The Circulatory System
Insulin is secreted into the bloodstream and helps the cells of the body make use of glucose. It is the responsibility of the circulatory system to provide the insulin for all the cells of the body. As long as enough insulin is produced by the body, the glucose is able to be used and the cells of the body thrive.
If there isnt enough insulin in the circulatory system, glucose levels go up and there can be complications, such as diabetic nephropathy , diabetic retinopathy , diabetic neuropathy , and heart disease.
A lack of insulin in the bloodstream results in starvation of the cells. As the cells cant make use of glucose, they start to break down fat to be used as cellular fuel. If glucose in the bloodstream becomes extremely high, ketones can build up in the body. Ketones are the metabolic byproduct of other sources of fuel the body is using. When ketones build up, there can be obvious symptoms, such as a dry mouth, nausea, vomiting, and a sweetness in the breath. When this happens, it is called diabetic ketoacidosis.
Read Also: How Long Do Type 2 Diabetics Live
The Discovery Of Insulin
In 1889 German scientists Minkowski and von Mering noted, from their experimental work with animals, that total pancreatectomy led to the development of severe diabetes. They hypothesised that a substance secreted by the pancreas was responsible for metabolic control. Others later refined this hypothesis, noting diabetes to be associated with destruction of the islets of Langerhans. While Minkowski, as well as Zuelzer in Germany and Scott in the USA attempted, with inconsistent results, to isolate and administer the missing pancreatic islet substance, Belgian investigator de Meyer in 1909 proposed the name insuline, as did British researcher Schaefer in 1916.
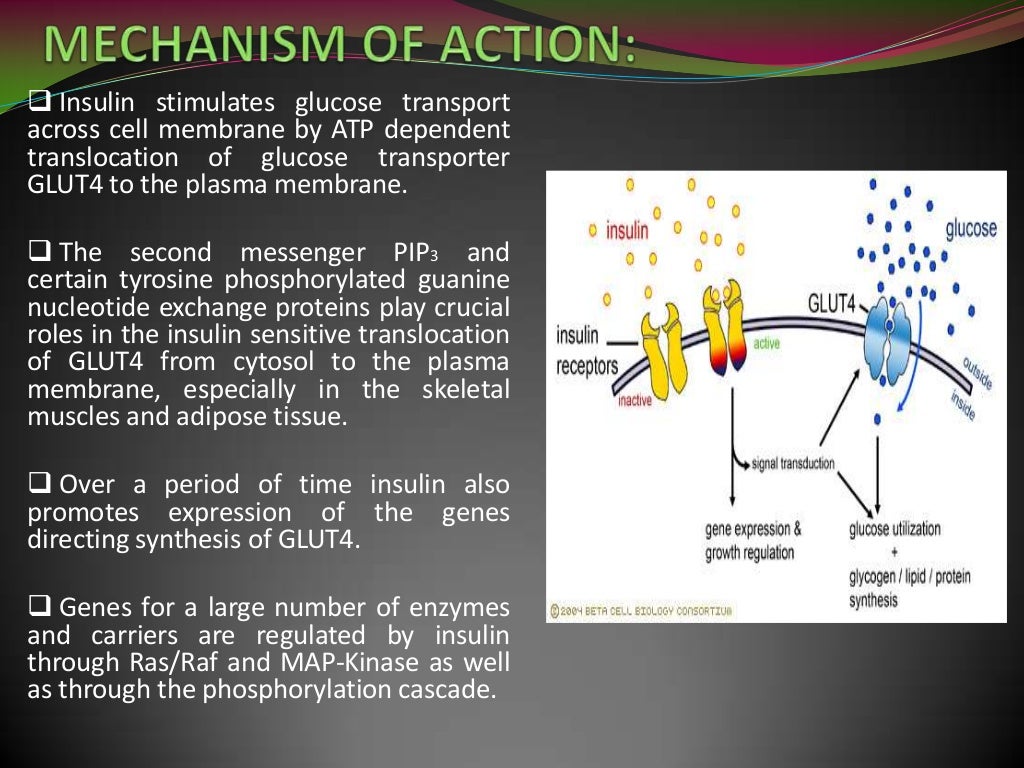
Insulin Receptors And Insulin Binding
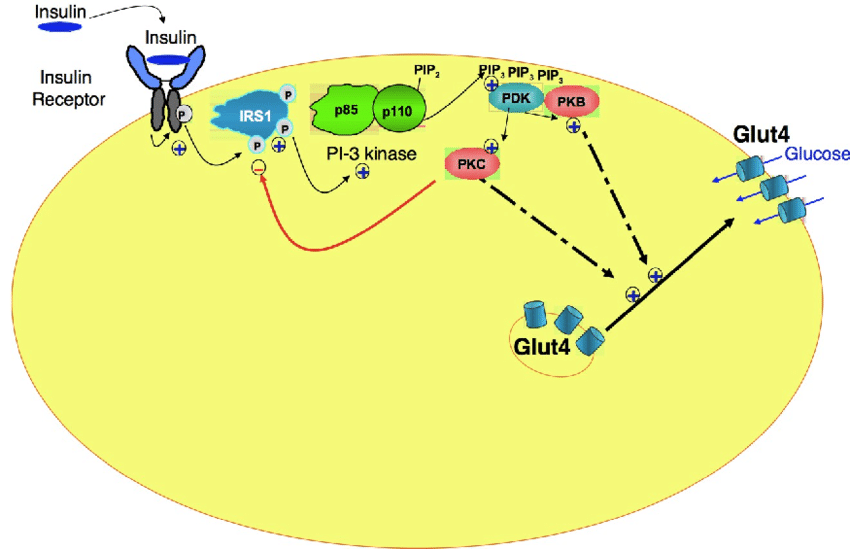
Insulin mediates its actions through binding to insulin receptors. The insulin receptor was first characterised in 1971. It consists of a heterotetramer consisting of 2 and 2 glycoprotein subunits linked by disulphide bonds and is located on the cell membrane. The gene coding for the insulin receptor is located on the short arm of chromosome 19. Insulin binds to the extracellular subunit, resulting in conformational change enabling ATP to bind to the intracellular component of the subunit. ATP binding in turn triggers phosphorylation of the subunit conferring tyrosine kinase activity. This enables tyrosine phosphorylation of intracellular substrate proteins known as insulin responsive substrates . The IRS can then bind other signalling molecules which mediate further cellular actions of insulin.
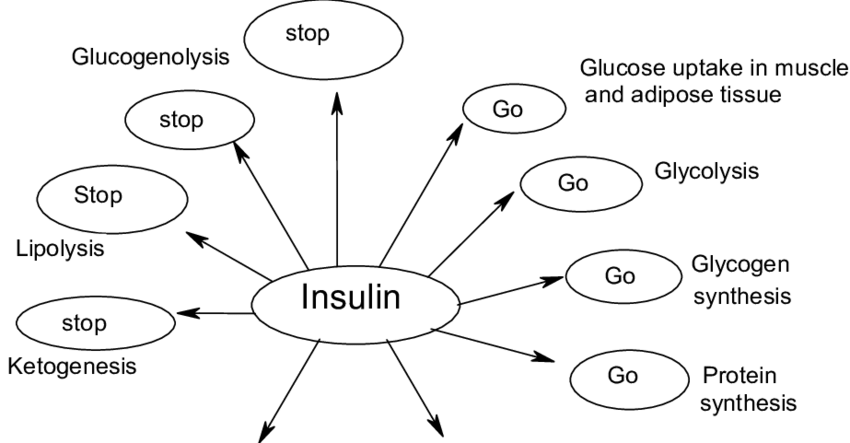
PI 3-kinase promotes the translocation of glucose transporter proteins, glycogen, lipid and protein synthesis, anti-lipolysis and the control of hepatic gluconeogenesis. PI 3-kinase acts via serine and threonine kinases such as Akt/protein kinase B , protein kinase C and PI dependent protein kinases1& 2 . The RAS pathway activates transcription factors and stimulates the growth promoting actions of insulin. Thus broadly, PI 3-kinase mediates insulins metabolic effects, e.g. cellular glucose uptake, while RAS significantly mediates insulins mitogenic effects, together with other less well described actions. These pathways are presented schematically in .
Recommended Reading: Can Metformin Lower Blood Pressure
Structure And Chemical Properties Of Insulin
Insulin was found to be a polypeptide in 1928 with its amino acid sequence identified in 1952. It is in fact a dipeptide, containing A and B chains respectively, linked by disulphide bridges, and containing 51 amino acids, with a molecular weight of 5802. Its iso-electric point is pH 5.5. The A chain comprises 21 amino acids and the B chain 30 amino acids. The A chain has an N-terminal helix linked to an anti-parallel C-terminal helix the B chain has a central helical segment. The two chains are joined by 2 disulphide bonds, which join the N- and C-terminal helices of the A chain to the central helix of the B chain. In pro-insulin, a connecting peptide links the N-terminus of the A chain to the C-terminus of the B chain.
What Are Alternative Medications For People With Diabetes That Arent Insulin
- Metformin a pill that stops sugar production in the liver
- Glitazones pills that remove sugar from the bloodstream
- Sufonylureas and glinides pills that increase the release of insulin from your pancreas
- Starch blockers pills that slow starch absorption
- Incretin therapies and amvlin analogs pills and injections that reduce sugar production in the liver and slow food absorption. Types of the former include DPP4 inhibitors and GLP1 analogs .
- SGLT2 inhibitors pills that are taken before meals that prevent the reabsorption of glucose
You May Like: How To Reduce Side Effects Of Metformin
What Severe Complications Can Occur Because Of Rationing Or Running Out Of Insulin
Diabetic ketoacidosis is an emergency condition that results if you dont have enough insulin to regulate your blood sugar. DKA causes your body to break down fat for energy in the absence of insulin. This leads to a dangerous accumulation of acids known as ketones in your blood that can cause your brain to swell and your body to go into shock.
Signs of diabetic ketoacidosis include:
- Thirst or a very dry mouth
- Frequent urination
- High levels of ketones in your urine
- Fatigue
- Nausea, vomiting, or stomach pain
- Difficulty breathing
- A fruity or acetone odor on your breath
- Confusion or acting drunk while sober
DKA is so common and can come on so quickly that it is the first sign of Type 1 diabetes in 20% of cases, and the way many type 1 diabetics are first diagnosed with the condition. If you go into diabetic ketoacidosis, dont try to hide it or make light of it. Treat it as the emergency it is and get to a hospital as soon as possible to recover. Ive had people tell me theyre tired of taking insulin, or that theyre rationing it due to cost. In type 1 diabetes, thats all it takes to end up in a life-threatening situation, says Dr. Zilbermint.
How Do You Take Insulin Without A Syringe
- Insulin pens look like large writing pens and can help prevent under- and overdosing. They also dont require refrigeration, are conveniently prefilled, and are more durable than syringes.
- Insulin pumps are attached to a thin tube thats implanted under your skin. Pumps are computerized or motorized, and some models also act as glucose monitors. They deliver insulin before each meal along with small amounts through the course of the day. In the US, about 60% of people with diabetes use some form of insulin pump.
- Jet injection devices are a good option if you hate needles. A jet injector holds several doses of insulin. After placing it against your skin, you press a button, and the insulin is pushed through.
- Inhalable insulin comes in a premeasured inhaler and was first approved in 2014. Its short-acting and usually not covered by insurance, which makes it more cost prohibitive than other types of insulin for most people with diabetes.
Unless you have an insulin pump that also works as a glucose monitor, insulin dosing is based on self-monitoring your blood glucose levels. You can check them by doing finger pricks or wearing a device that continuously monitors them for you.
Recommended Reading: Metformin Dehydration
B Mitochondrial Energetics Oxidative Stress And Insulin Resistance
However, the relationship between mitochondrial activity and insulin action is more complex than the simple model outlined above, in which insulin-resistant myocytes store rather than oxidize lipid. Interestingly, after several weeks of high-fat feeding, rodents develop skeletal muscle insulin resistance in parallel with increased capacity for fatty acid oxidation ex vivo . This may reflect an adaptive response that insufficiently compensates for increased lipid availability, leading to IMCL accumulation and insulin resistance . Indeed, even potent activation of FAO, by pharmacological AMPK activation or acetyl-CoA carboxylase 2 deletion, is insufficient to protect mice from HFD-induced muscle insulin resistance, highlighting the primacy of ATP demand rather than substrate supply in mitochondrial energetics . Alternatively, there is evidence that increased relative -oxidative flux may itself drive insulin resistance in skeletal muscle, contrary to the initial hypothesis that impaired lipid oxidation drives muscle insulin resistance. This hypothesis is supported by several models in which blocking -oxidative flux improves muscle insulin sensitivity, even despite IMCL accumulation . However, increased FAO is certainly not necessary for lipid-induced muscle insulin resistance, as demonstrated by the muscle insulin resistance of constitutively glucose-oxidizing Pdk2/4/ mice .
The Effects Of Insulin On The Body
Insulin is a natural hormone produced by your pancreas that controls how your body uses and stores blood sugar . Its like a key that allows glucose to enter cells throughout your body.
Insulin is a vital part of metabolism. Without it, your body would cease to function.
When you eat, your pancreas releases insulin to help your body make energy out of glucose, a type of sugar found in carbohydrates. It also helps you store energy.
In type 1 diabetes, the pancreas is no longer able to produce insulin. In type 2 diabetes, the pancreas initially produces insulin, but the cells of your body are unable to make good use of the insulin. This is called insulin resistance.
Unmanaged diabetes allows glucose to build up in the blood rather than being distributed to cells or stored. This can wreak havoc with virtually every part of your body.
Blood tests can quickly indicate whether your glucose levels are too high or too low.
Complications of diabetes include kidney disease, nerve damage, heart problems, eye problems, and stomach problems.
People with type 1 diabetes need insulin therapy to live. Some people with type 2 diabetes must also take insulin therapy to control their blood sugar levels and avoid complications.
If you have diabetes, insulin therapy can do the job your pancreas cant. The following types of insulin are available:
Read Also: Metformin Medicine Side Effects
What Is The Role Of Insulin In Diabetes
Insulin is the hormone that plays the biggest role in diabetes. The impairment or lack of secretion of insulin will lead to the formation of diabetes mellitus. There are two types of diabetes:
- Insulin Dependent Diabetes Mellitus also known as type-1 diabetes.
- Non-Insulin Dependent Diabetes Mellitus is also known as type-2 diabetes.
The role of insulin in both types of diabetes is explained as follows:
C Insulin Suppression Of Glucagon Secretion
Glucagon action is important for normal glucose homeostasis , and given its potent anti-insulin effects on the liver in particular, it is not surprising that an elegant and tightly controlled reciprocal paracrine regulatory system has evolved to favor either insulin or glucagon secretion, but not both, in any given metabolic state . It was shown in 1970 that insulin-deficient diabetes was a state of relative hyperglucagonemia and -cell hyperresponsiveness to the glucagon secretagogue arginine , and subsequent studies confirmed that insulin acts in a paracrine manner to suppress glucagon release from the islet . Insulin per se is sufficient to suppress glucagon levels during euglycemia and hypoglycemia in humans with type 1 diabetes , and fasting glucagon levels are correlated with insulin resistance in nondiabetic humans . Mice lacking the insulin receptor in -cells provided direct genetic evidence for this mechanism these mice exhibited hyperglucagonemia in the fed state and during insulin tolerance tests . The mechanism for insulin suppression of -cell glucagon secretion is incompletely elucidated but has been shown to involve PI3K activity and phosphodiesterase-mediated degradation of cAMP . Overall, the importance of glucagon in insulin action and diabetes is underappreciated the inability of mice lacking the glucagon receptor to develop diabetes upon -cell destruction is only one of many striking illustrations of this .
Recommended Reading: Metformin Maximum Dose
How Well Does Insulin Treat Diabetes
Efficacy of insulin
- In a 24 week study of patients with type 1 diabetes, regular human subcutaneous insulin before breakfast and dinner plus human insulin isophane suspension twice daily reduced HbA1c by 0.4% from baseline and fasting glucose by -6 mg/dl.
- In a 24 week study of patients with type 2 diabetes, regular human subcutaneous insulin before breakfast and dinner plus human insulin isophane suspension twice daily reduced HbA1c by 0.6% from baseline and fasting glucose by -6 mg/dl.
Conditions For Testing Dia
2:00am: 9.53:00am: 9.6
BG readings dropped from 10pm to 2am , then did not drop further after that. Therefore, it makes sense to set the DIA setting at 4 hours. If your childs pump allows IOB to be set in half hour increments, you could check BG at half-hour points after the 3-hour mark, to see if your childs individual IOB setting is actually 3.5 hours. In this case, in the context of the above example, if the 1:30am BG reading was 9.5, then the insulin actually stopped lowering BG at 1:30 , so you may choose to set IOB at 3.5 hours, rather than 4 hours. If the 1:30am reading was 10.2, then BG did not stop dropping until 2 am, so you may choose to set DIA/IOB at 4 hours.
Don’t Miss: Are Overnight Oats Good For Diabetics

