Can I Have A Negative Reaction To Insulin
One complication facing people with diabetes who use insulin is the potential for severe hypoglycemia, also known as insulin shock, which involves using too much insulin and causing your blood sugar to drop extremely low. This can cause coma, seizures, and heart attacks, says Dr. Powers. It requires treatment in a hospital but thankfully is highly treatable once you are there.
What Happens If I Have Too Much Insulin
If a person accidentally injects more insulin than required, e.g. because they expend more energy or eat less food than they anticipated, cells will take in too much glucose from the blood. This leads to abnormally low blood glucose levels . The body reacts to hypoglycaemia by releasing stored glucose from the liver in an attempt to bring the levels back to normal. Low glucose levels in the blood can make a person feel ill.
The body mounts an initial ‘fight back’ response to hypoglycaemia through a specialised set of of nerves called the sympathetic nervous system. This causes palpitations, sweating, hunger, anxiety, tremor and pale complexion that usually warn the person about the low blood glucose level so this can be treated. However, if the initial blood glucose level is too low or if it is not treated promptly and continues to drop, the brain will be affected too because it depends almost entirely on glucose as a source of energy to function properly. This can cause dizziness, confusion, fits and even coma in severe cases.
Some drugs used for people with type 2 diabetes, including sulphonylureas and meglitinides , can also stimulate insulin production within the body and can also cause hypoglycaemia. The body responds in the same way as if excess insulin has been given by injection.
What Happens If I Have Too Little Insulin
People with diabetes have problems either making insulin, how that insulin works or both. The main two types of diabetes are type 1 and type 2 diabetes, although there are other more uncommon types.
People with type 1 diabetes produce very little or no insulin at all. This condition is caused when the beta cells that make insulin have been destroyed by antibodies , hence they are unable to produce insulin. With too little insulin, the body can no longer move glucose from the blood into the cells, causing high blood glucose levels. If the glucose level is high enough, excess glucose spills into the urine. This drags extra water into the urine causing more frequent urination and thirst. This leads to dehydration, which can cause confusion. In addition, with too little insulin, the cells cannot take in glucose for energy and other sources of energy are needed to provide this energy. This makes the body tired and can cause weight loss. If this continues, patients can become very ill. This is because the body attempts to make new energy from fat and causes acids to be produced as waste products. Ultimately, this can lead to coma and death if medical attention is not sought. People with type 1 diabetes will need to inject insulin in order to survive.
You May Like: What Goes Wrong When Juvenile Diabetes Sets In
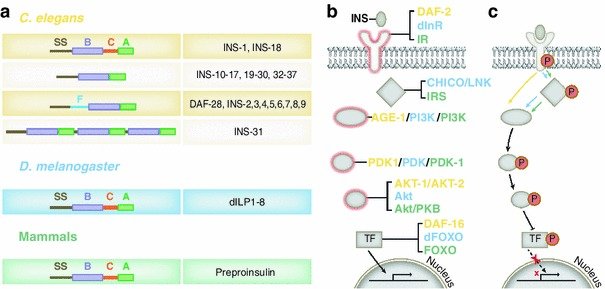
Demonstration Of Biosynthesis From A Single
The processes involved in insulin biosynthesis were elucidated by Donald Steiner and colleagues in the late 1960s and have been recently reviewed by him in a reflections article . Steiner showed, by incubating tissue slices from a rare insulin-producing adenoma of the pancreas in a medium containing tritium-labeled leucine and phenylalanine, that extracts from these incubated samples contained insulin as well as a higher molecular weight component of 910 kDa. This higher molecular weight component was then shown to consist of a single-chain polypeptide that he called proinsulin. Proinsulin contained the B-chain at its N-terminus and the A-chain at its C-terminus, with a connecting segment, the C-peptide, in the middle . The first reports of these findings were in 1967 , with the sequence of porcine proinsulin being reported in 1968 by Chance et al. from Eli Lilly.
The identification and characterization of the subtilisin-like convertases that carry out the proteolytic removal of the C-peptide to yield the two-chain insulin molecule was a major challenge and took a further 20 years .
How Glucose Moves Through Your Body
Our bodies can make glucose , but most of what we use, we get from eating. Glucose is present in all plants and animals, usually in more complex carbohydrate forms like lactose, sucrose, and starch. So whats a carbohydrate? Carbohydrates are a combination of hydrogen, carbon, and oxygen and one of the three macronutrients your body uses for energy. They can be simple or complex .
Heres a quick look at how glucose goes from that donut you eat to the energy that powers your bodys cells.
It may help to start with a basic view of the path glucose travels: from your mouth down into your small intestine then out into the bloodstream, where it takes a quick trip through the liver and moves through your body via your blood it leaks out of the capillaries, into the interstitial fluid around the cells, and finally through the cell membrane and into the cell.
Source: OpenStax Anatomy and Physiology
Sensing: As soon as you start eating, receptors on your tongue and in your gut and pancreas sense the presence of carbohydrates. This sets off a chain reaction of events to tell the body to process and use this fuel.
Signaling: As soon as the body detects glucose, a complex set of signaling instructions is triggered. For example, glucagon-like peptide-1 tells beta cells in the pancreas to produce and release more insulin, which helps direct the glucose to cells and helps the cells absorb it.
Also Check: Can Metformin Cause Hypoglycemia
What Are The Drawbacks To Insulin Treatment For Diabetes
The biggest issue with insulin right now is unaffordability. A box of rapid-acting insulin can cost $400 without insurance. As so many people continue to lose their health coverage, its becoming an enormous problem, Dr. Zilbermint says.
Consistently rising costs have led some patients to ration their insulin, which can be dangerous and even deadly. The cost of testing strips is also an issue, and both have led to a black market in testing strips and insulin. Its illegal, says Dr. Zilbermint, but its happening.
How Should I Store My Insulin
- Keep current insulin at room temperature to help alleviate injection discomfort.
- Insulin can usually be stored at room temperature for about a month. Once in use, insulin pens should be stored at room temperature. Expiration dates of insulin pens can vary depending upon the type of insulin. For disposable pens, you should discard the entire device when empty or when you reach the expiration date.
- Store extra insulin in the refrigerator.
- Dont expose insulin to excessive cold or heat.
Read Also: Is Metformin An Antibiotic
Preparation Of Solutions And Buffers
Stocks
-
Weigh 5 mg of insulin per 1 mL of 5 mM HCl .
-
Freeze in aliquots of 500 L to prepare 50 mL of medium or aliquots of 5 mL to prepare 500 mL of medium.
-
Human recombinant EGF:
-
Dissolve in 1 mL sterile H2O containing 0.1% BSA as a carrier protein .
-
Freeze in aliquots of not bigger than 10 L.
-
Use 2 L to prepare 100 mL of medium or 10 L to prepare 500 mL of medium.
-
Human recombinant bFGF:
-
Dissolve in 500 L sterile H2O containing 0.1% BSA as a carrier protein .
-
Freeze in aliquots of not bigger than 5 L.
-
Use 1 L to prepare 100 mL of medium or 5 L to prepare 500 mL of medium.
Proliferation Medium
For 100 mL, use the following composition:
| Components | |
|
|
Mark A. Sperling MD, … Moshe Phillip MD, in, 2014
So What Is A Hormone Really
Hormones are chemical components that are produced in one part of the body and function at an entirely different one . They include proteins, peptides and lipids, existing usually as precursor molecules . In addition hormones have various functions such as the regulation of metabolism and its development. A major role is to act as messengers and carry information around tissues in the body by binding receptors on cell surfaces or within a cell . Receptors are proteins on cell surfaces or within them with available sites for the signalling ligand molecule to bind on. The receptor’s major role is to act as the conductor for hormones and drugs to reach the body and the target they require. One of the main peptide hormones studied through years due to its importance and necessity is insulin, whose structure, synthesis and function are discussed further below.
Don’t Miss: Insulin Stimulates The
Fasting Plasma Glucose Test
Before your physical, your doctor will ask you to fast for eight hours. This is so they can measure your fasting plasma glucose, or the concentration of glucose in your blood. As you can imagine, if you ate a donut on your way to the appointment, your blood at that moment would show very high levels of blood sugar. Fasting gives us some approximation of your typical glucose concentration. Unfortunately, its still a single point in time, where, as we saw above, your level could be high or low depending on how well you slept the night before or how stressed you get at the doctors office.
So what results do you want to see? According to the American Diabetes Association , people fall into three categories depending on their fasting plasma glucose levels:
- Normal: Under 100 mg/dL
- Prediabetes: 100125 mg/dL
- Diabetes: Higher than 125 mg/dL
Its important to note that these are benchmarksa fasting glucose level of 99 mg/dL is still less than ideal. And people with prediabetic or diabetic levels can work to bring their glucose back down to healthy ranges.
How Do You Take Insulin Without A Syringe
- Insulin pens look like large writing pens and can help prevent under- and overdosing. They also dont require refrigeration, are conveniently prefilled, and are more durable than syringes.
- Insulin pumps are attached to a thin tube thats implanted under your skin. Pumps are computerized or motorized, and some models also act as glucose monitors. They deliver insulin before each meal along with small amounts through the course of the day. In the US, about 60% of people with diabetes use some form of insulin pump.
- Jet injection devices are a good option if you hate needles. A jet injector holds several doses of insulin. After placing it against your skin, you press a button, and the insulin is pushed through.
- Inhalable insulin comes in a premeasured inhaler and was first approved in 2014. Its short-acting and usually not covered by insurance, which makes it more cost prohibitive than other types of insulin for most people with diabetes.
Unless you have an insulin pump that also works as a glucose monitor, insulin dosing is based on self-monitoring your blood glucose levels. You can check them by doing finger pricks or wearing a device that continuously monitors them for you.
Don’t Miss: What Is The Normal Dose Of Metformin
What Does Insulin Do
Insulin is a hormone that is central to regulating glucose metabolism in the body to produce energy. Insulin causes cells in the liver, muscle, and fat tissue to take up glucose from the blood, which it then converts to glycogen which is stored in the liver and muscle. When insulin is absent, glucose is not taken up by body cells and the body begins to use fat as an energy source.
Regulator Of Endocannabinoid Metabolism
Insulin is a major regulator of endocannabinoid metabolism and insulin treatment has been shown to reduce intracellular ECs, the 2-arachidonoylglycerol and anandamide , which correspond with insulin-sensitive expression changes in enzymes of EC metabolism. In insulin-resistant adipocytes, patterns of insulin-induced enzyme expression is disturbed in a manner consistent with elevated EC synthesis and reduced EC degradation. Findings suggest that insulin-resistant adipocytes fail to regulate EC metabolism and decrease intracellular EC levels in response to insulin stimulation, whereby obese insulin-resistant individuals exhibit increased concentrations of ECs. This dysregulation contributes to excessive visceral fat accumulation and reduced adiponectin release from abdominal adipose tissue, and further to the onset of several cardiometabolic risk factors that are associated with obesity and type 2 diabetes.
Hypoglycemia, also known as “low blood sugar”, is when blood sugar decreases to below normal levels. This may result in a variety of symptoms including clumsiness, trouble talking, confusion, loss of consciousness, seizures or death. A feeling of hunger, sweating, shakiness and weakness may also be present. Symptoms typically come on quickly.
Also Check: Hyperglycemia Meal Plan
Human Versus Analogue Insulins
Insulin analogues are clearly helpful in managing T1DM, which requires complete replacement of endogenous insulin and accurate matching of the profile of action to daily needs. The degree to which both long-acting and rapid-acting analogues offer advantages over NPH and regular human insulin for T2DM is less well established and a focus of debate. Among the issues is that both the list price and the direct cost to patients can be much higher for the analogues.142,233,234 Both long-acting and rapid-acting insulin analogues have been shown in large studies to cause less frequent hypoglycemia than human insulins, but for some patients little difference may be found. The absolute risk of severe hypoglycemia in patients with T2DM is relatively small, approximately one-third to one-tenth as high as in similarly treated patients with T1DM. This risk can be further minimized with appropriate education of patients and expectant monitoring of glucose at times when hypoglycemia is most likely to occur, such as at night or during unplanned or strenuous activity. Allergies to currently available insulins are rare, as are chronic skin reactions, which include lipoatrophy and lipohypertrophy.
J.P. Hill, … V.A. Landells, in, 2011
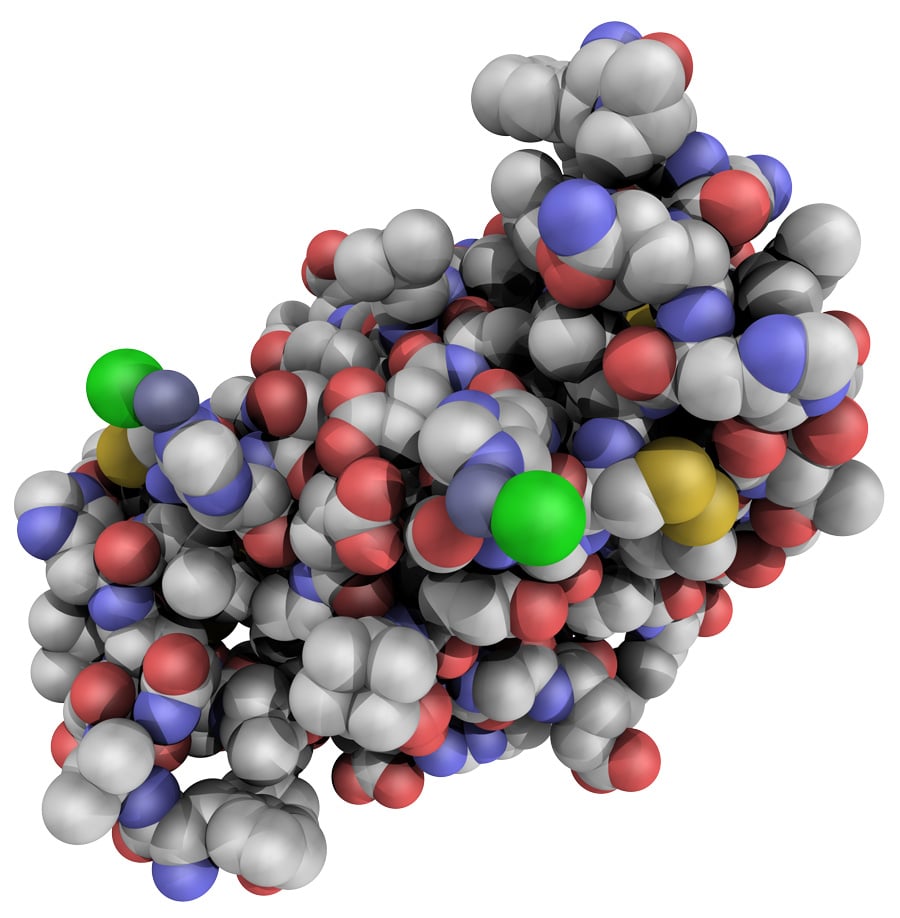
Insulin And Insulin Analogues
Insulin is a hormone secreted by -islets of Langerhans. It is a polypeptide with a molecular weight of 6000 Da, consisting of two amino acid chains A and B linked by two disulfide bridges. The A and B chain contains 21 and 30 amino acids, respectively . Insulin was the first therapy used in the treatment of DM regardless of the types . In order to enhance its effectivity, stability, and duration of action, number of insulin analogues were prepared and tested, for example, first generation rapid-acting insulin analogues such as insulin lispro and insulin aspart , second generation basal insulin analogues such as insulin glargine and insulin detemir , and third generation rapid-acting insulin analogues such as insulin glulisine .
Compared to human insulin preparations, the rapid-acting analogues dissociate more rapidly, and therefore, have a more rapid onset of action, with higher peak serum concentration, and a more rapid tailing off effect. The longer duration of action of the insulin analogues, relative to protaminated or zinc-retarded human insulin, potentially offers a better coverage in between-meal period. Their flatter pharmacodynamic profile, with a much lower peak of action, reduced the risk of hypoglycemia . However, with all such advancement in the preparation of insulin analogues, there was no discernable clinical advantage over the classical insulin preparation .
Figure 2. Assembling nature of human insulin: proinsulin, insulin and its derivatives.
You May Like: Which Of The Following Symptoms Is Not Associated With Type 1 Diabetes
Insulin And Insulin Preparations
Insulin
Diabetes mellitus type 1 is a disease caused by the lack of insulin and its treatment requires insulin supplementation.
Insulin produced by the pancreatic cells and is one of the most important hormones in mammalians regulating carbohydrate and fat metabolism in the body for energy production and many other vital activities. Insulin performs also unique functions within the central nervous system . It crosses the bloodbrain barrier, affecting feeding and cognition through CNS mechanisms largely independent of glucose utilization, and regulates lipid metabolism and cholesterol synthesis. Insulin also reduces myocardial O2 consumption and increases cardiac efficiency. It seems to augment cardiomyocyte contraction, while it affects favorably myocardial relaxation, stimulates vascular endothelial growth factor and thereby angiogenesis, suppresses apoptosis, promotes cell survival, and ameliorates both myocardial microcirculation and coronary artery resistance, leading to increased blood perfusion of myocardium . More than 250 books, 80,000 reviews, and half a million articles have been published about insulin.
For 30 years, diabetic patients were successfully treated with insulin without researchers knowing the chemical structure of the hormone, which is a 51-amino-acid polypeptide.
Fig. 26.1. Structure of insulin.
Two disulfide bridges covalently tether the chains, and chain A contains an internal disulfide bridge .
Insulin Preparations
What About Insulin’s Structure It Seems To Be Very Complicated
Insulin is a peptide hormone composed of 51 amino acids and has a molecular weight of 5808 Da. It is produced in the islets of Langerhans in the pancreas. The name comes from the Latin insula for “island”. Insulin’s structure varies slightly between species of animals. Insulin from animal sources differs somewhat in “potency” in humans because of those variations. Pig insulin is especially close to the human version. Insulin was the first protein whose amino acid sequence was identified and the first to be synthesized. It is initially synthesized as a precursor molecule known as proinsulin and on cleavage it gives two peptides chains, one comprising of 21 amino acids and the other of 30 amino acids, being mostly conserved in humans and animals . The two chains are joined together by two disulfide bonds between two cysteine residues, where a disulfide bond is the linkage bond between two sulfurs as shown below.
Figure 1. The two chains comprising the insulin structure, A and B, indicating also a disulfide bond between cysteines , since they are very important in stabilizing the two chains together. Chain structure from Ref. .
The insulin hexamer with two of the main binding sites shown next to it. From Ref..
Read Also: Normal Dosage For Metformin

