Insulin Pump Therapy With Automated Insulin Suspension
There is a pump that currently has a threshold suspend. This means that a sensor inserted just under the skin, reads glucose every 5 minutes and transmits it directly to the pump. The pump stops delivering insulin for two hours if glucose levels fall below patients lowest glucose target unless the person can acknowledge that they are okay and resume insulin delivery immediately. In a way that is good, if the patients glucose is low and can lose consciousness. However, if the patients glucose is normal and the sensor sends a false low glucose level to the pump and it stops the insulin, the person can end up with very high blood sugar if they dont resume the insulin right away. A problem I have found with some patients often on this particular pump due to sometimes the inaccuracy of the sensor.
A Pump May Be A Good Choice For:
- People who like the idea of a pump. If this is what you want, or what you want for your child, and it can be used it safely, then it should be used.
- Active people, who benefit from changes in basal rates or suspending the pump when exercising.
- People who have frequent low blood sugar reactions.
- Anyone who has delays in absorption of food from the stomach .
- Women planning pregnancy.
- People who want to use the pumps bolus calculator functions to determine insulin doses.
Tip From The Trenches
We originally set my sons IOB setting at 3.5 hours. When we changed it to 4 hours, the reduction in BG swings was noticeable. It seems that this was happening: when the pump calculated a correction dose at 3.5 hours, it did so assuming that there was no insulin still acting. But, apparently, my sons body takes a little longer to use up his insulin, so at 3.5 hours, there WAS still active insulin remaining. As a result, when we gave a correction dose we were over-correcting, resulting in below-target BGs later. When we started taking this unused insulin into account, we empowered the pump to calculate a more appropriate dose. ~Michelle
The above information was reviewed for content accuracy by clinical staff of the Alberta Childrens Hospital Diabetes Clinic.
Don’t Miss: Acceptable A1c Levels
Disadvantages Of Using A Diabetes Insulin Pump
Although there are many good reasons as to why using an insulin pump can be an advantage, there are some disadvantages.
The disadvantages of using an insulin pump are that it:
- Can cause weight gain
- Can cause diabetic ketoacidosis if your catheter comes out and you dont get insulin for hours
- Can be expensive
- Can be bothersome since you are attached to the pump most of the time
- Can require a hospital stay or maybe a full day in the outpatient center to be trained
There are pluses and minuses to using an insulin pump. Even though using an insulin pump has disadvantages, most pump users agree the advantages outweigh the disadvantages.
Conventional Insulin Pump Therapy
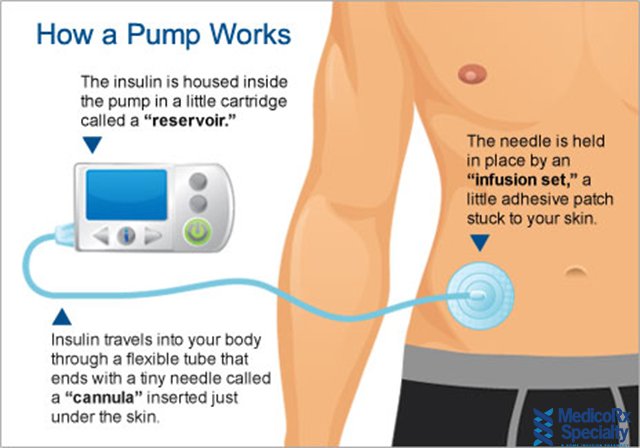
An insulin pump is a small, digital device that continuously delivers rapid-acting insulin through a small catheter inserted into the subcutaneous tissue and secured in place on the skin with adhesive . In most insulin pumps, the infusion set connects to the pump by plastic tubing, and insulin infuses from the pump through the tubing to the infusion set cannula and into the subcutaneous tissue . Some pumps, referred to as patch pumps, do not use tubing and instead adhere directly to the skin. Patch pumps deliver insulin through the infusion cannula and are programmed from a remote device using wireless technology .
Insulin pump with tubing. The tubing connects the insulin pump, which contains the reservoir where the insulin is held, to the infusion cannula inserted in the subcutaneous tissue.
Insulin pump without tubing . Tubeless patch pumps contain the insulin reservoir and the infusion cannula and adhere directly to the skin. A handheld device is used to program insulin delivery and insert the infusion cannula.
Commercially Available Insulin Pumps, United States, as of March 2019
Don’t Miss: What Pasta Can Diabetics Eat
Pump Safety Is A Commitment
The one requirement for using a pump is that you and/or your caregivers are ready and willing to do what it takes to use the pump safely. Checking blood sugar is important because it will warn you if your pump stops working right or your infusion set stops working. This can cause high blood sugar levels and cause diabetes ketoacidosis , which is very serious and dangerous. Checking blood sugar levels frequently will alert you to this possibility and will prevent the development of ketones.
Potential Benefits Of Pump Therapy
The expected benefits of insulin pump therapy are summarized in . Insulin pump use provides a near-physiologic basal-bolus insulin delivery method that, in theory, mimics normal pancreatic function better than injections . Precise insulin dosages can be programmed and administered, giving the patient increased flexibility in daily living with regard to mealtimes, travel, work schedule, etc. . Observational studies, meta-analyses, and randomized clinical trials have demonstrated improvements in long-term glycemic control when compared with daily multiple-dose insulin injections . Evidence from clinical studies suggests that pump therapy is associated with a decreased risk of severe hypoglycemia and the need for emergent medical care . The latter translates into reduction in the cost of care and utilization of health care resources . Quality of life measures have shown improvement with pump therapy compared with MDII .
You May Like: Tight Control Diabetes
Is An Insulin Pump Right For Me How Do I Know It Is Right For Me
If you or a person that has diabetes and uses insulin, an insulin pump might be the right choice. ;Ask your diabetes educator to tell you about what features might be best for your needs. Insulin pumps are a long term decision, and its normal to rely on a pump for 4 to 5 years, so its important to discuss different options with your health care provider so that you can assess the features and choose a pump that is right for you.
Insulin pumps are not for everybody. Not all patients with Type 2 diabetes are recommended to use an insulin pump, especially if the diabetes is already under control using oral medications. They are also not recommended for patients with pre-diabetes. Its best to speak to your physician about whether you should use an insulin pump or not.
Tips For Using Insulin Pump Therapy
If used properly, insulin pumps and their related components are reliable and safe. But as with any technology, problems can sometimes occur. It’s important to be aware of potential problems and what to do if they arise, to maintain blood sugar levels and avoid side effects.
Tips for proper insulin pump therapy include:
- Watch for cannulas becoming kinked, or leakage in the reservoir or the infusion sets. Kinked cannulas and insulin leaks can lead to interruption of insulin flow, blockages, or mechanical failures.
- Check your pump for damage, such as a cracked display or jammed buttons.
- Make sure your battery is working, check the battery indicator and replace the battery as needed. Check for a loose or damaged battery cap to avoid unexpected power loss.
- Don’t expose your pump to water if it is not waterproof. Also avoid exposing the internal casing to water by changing the battery only in a dry area and making sure that the battery cover is not worn out or missing.
- Understand your personal settings. Be sure to adjust the program to account for changes in activity or diet.
- Change the infusion set according to the instructions for the infusion set you are using and the recommendations of your doctor or health care team.
- Pay attention to device alerts, such as beeps or vibrations. Make sure the volume is set high enough so that you can hear it.
Recommended Reading: Does Walmart Sell Insulin Over The Counter
How Do Insulin Pumps Work
Insulin pumps deliver insulin by continuous infusion through a single subcutaneous site which is replaced, on average, every three days. Only rapid-acting insulin is used, and the analogue insulins have gained popularity over regular insulin for this purpose . A pump delivers programmable basal insulin around the clock which is tailored to the patients 24-h glucose profile. The insulin requirements may be affected by the individuals physiology, the type and duration of daily activity, work schedule, exercise, illness, concomitant medications, etc. Most patients utilize multiple basal rates over a 24-h period, but some may use a single rate. Almost all pumps have the capability of programming basal rates that are modifiable every hour and also have a temporary basal rate feature for special situations. Patients can also deliver bolus insulin which infuses over a few minutes to a few hours. Insulin boluses cover meals and correct for high blood glucose levels. For the pump to accurately calculate bolus insulin amounts, the carbohydrate content of food and the blood glucose level are required. Insulin delivery via the pump can be suspended by the patient if necessary.
How Insulin Pumps Work
Insulin pumps are worn externally and deliver a continuous amount of fast-acting insulin 24 hours a day.
There are three main components to insulin pump therapy:
- a pump , which pumps the insulin into your body
- a reservoir or a cartridge, where insulin is held
- an infusion set, which includes a thin tube that runs from the reservoir in the pump to the infusion site on your body, and a short cannula that is inserted under your skin
The main steps to using the pump include placing the insulin-filled reservoir inside the pump, and inserting the cannula under your skin using a needle. The cannula is held in place with an adhesive patch for 24 to 72 hours, after which time it should be replaced. A tube connects the cannula to the reservoir in the pump and delivers a set amount of insulin into your body.
Two types of insulin doses are delivered to your body by the pump:
- Basal insulin doses are delivered continuously over 24 hours and keep your blood sugar levels stable between meals and overnight.
- Bolus insulin doses are delivered when you push a button on the pump – you can use them when you eat to correct high blood sugar levels.
The pump can be worn in many places on your body. It can be attached to your waistband, pocket, bra, armband, or underwear. When you sleep, you can lay it next to you on your bed or nightstand. You can disconnect the pump for activities such as swimming or showering. Insulin pumps that are not waterproof should not be exposed to water.;
Don’t Miss: Do Bananas Raise Your Blood Sugar
What It The Insulin Pump Function
Insulin pump is a treatment method used instead of needle therapy in diabetes mellitus. Insulin pump is an ideal method for pediatric use, provided that blood sugar measurement is guaranteed much more than needle treatment and a great responsibility is given to how the pump should be used. Individuals using insulin pumps should be under the control of a physician who can transfer the requirements of diabetic care to the patient and know how to use the insulin pump, according to needle therapy.
The insulin pump performs an insulin release called the basal dose, which periodically provides insulin to meet metabolic needs and body functions. Patients send a meal before the meal before they eat. As long as mid-range insulin is used, as in the case of needle therapy in the treatment of insulin pump, the patient will not have to feed on meal times based on the insulin injection schedule, which he must apply in pencil therapy.
The insulin pump is an alachronic device that releases body insulin by means of a tube connected to a catheter placed in the hip, belly, upper arm or leg region. The catheter is replaced every three days.
Many insulin pumps can calculate the meal or correction bolus.
Minimed 630g Insulin Pump With Optional Cgm

The MiniMed 630G insulin pump delivers precise doses of insulin to your body. When combined with our CGM, it takes action for you with the SmartGuard Suspend on low feature – providing protection that can help keep your glucose levels stable. ,3
Individuals pictured and/or quoted here were compensated for spending the day with us and allowing us to photograph them and their family. Their thoughts and opinions are their own.
Important Safety Information: MiniMed 770G System With SmartGuard TechnologyThe MiniMed 770G system is intended for continuous delivery of basal insulin and administration of insulin boluses for the management of type 1 diabetes mellitus in persons two years of age and older requiring insulin as well as for the continuous monitoring and trending of glucose levels in the fluid under the skin. The MiniMed 770G System includes SmartGuard technology, which can be programmed to automatically adjust delivery of basal insulin based on continuous glucose monitoring sensor glucose values and can suspend delivery of insulin when the SG value falls below or is predicted to fall below predefined threshold values.
The Medtronic MiniMed 770G System consists of the following devices: MiniMed 770G Insulin Pump, the Guardian Link Transmitter, the Guardian Sensor , one-press serter, the Accu-Chek® Guide Link blood glucose meter, and the AccuChek®Guide Test Strips. The system requires a prescription.
Also Check: What Is The Normal A1c Range
How Much Does An Insulin Pump Cost
Insulin pumps arent always covered by insurance companies. In many cases, to get insurance coverage for an insulin pump, your doctor will need to approve it as medically necessary.
If they arent covered by insurance, insulin pumps can be costly you can expect to pay about $6,000 for the device itself. Thats not counting the cost of batteries, sensors, and other supplies, which can run you another $3,000 to $6,000 annually. Finally, youll need to pay separately for insulin delivered by a pump!
Whats The Best Insulin Pump
This really depends on many factors, both personal and institutional. So many different things go into ones choice on a big diabetes device purchase like this, ranging from the specific features you prefer, to how it works with other technology and smartphones, and whether it includes tubing or is a tubeless patch pump.
Access and affordability are also huge factors that make this decision for many people, because insurance plans dont always like to cover expensive medical devices like these or they have specific criteria that must be met in order to buy a particular insulin pump.
Talking to your healthcare professional about the different options and what might work best for your diabetes management is always advisable, as well as reviewing credible and reliable information online about how the various technologies work.
User reviews can also make a big difference in deciding on which insulin pump may be right for you. You can start by checking out our product reviews here at DiabetesMine on Medtronic, Omnipod and Tandem pumps.
As the saying goes, it all depends on you and whats important for your life with diabetes.
Also Check: How Long Do Type 1 Diabetics Live
Getting Started With An Insulin Pump
Once you have talked with your diabetes care team and have become comfortable with all of the options on your insulin pump, you and your team will need to do the following in order to get you started.
Other Factors To Consider:
- The insulin pump doesnt take away the need to check blood sugar.
- There are technical aspects to using a pumpsetting it up, putting it in, interacting with itthat are more complicated in some ways than using injections.
- If it breaks or falls off, the person wearing it needs to be ready to give insulin by;injection;any time it is needed.
- It can be expensive, so find out which pumps are covered by your insurance and if those pumps meet your needs.
- All pumps are an extra piece of hardware attached to your body, either with tubing or attached to your skin. There are many clever ways to wear pumps and hide them from view, but they do take a bit of getting used to at first.
Recommended Reading: How To Test For Diabetes Insipidus
Interoperability And Homemade Diabetes Tech
The future of insulin pumping definitely appears to be connecting these devices to CGMs for improved blood glucose control. This of course has pushed to the forefront the issue of device interoperability and do-it-yourself technology.
Behind this evolution has been pressure from the patient community rallying behind a #WeAreNotWaiting mantra pushing to get innovative technology out more quickly and allow data and device integration.
Many of the folks creating DIY connected systems are using older, discontinued insulin pumps such as the Minimed Revel and Paradigm models. Despite an FDA warning and mainstream media concern that surfaced in 2019, thousands of people are now safely and successfully using these homemade systems.
Meanwhile, FDA has published new interoperability protocols to help the established medtech industry create products that are more modular and can work together safely and seamlessly. For insulin pumps like the Tandem t:slim X2, that means gaining a marking that new pump as interoperable technology.
This is important to keep in mind when shopping for new insulin pump technology.

