Insulin Makers Say They Are Held Captive By Pbms
The insulin makers maintain they have done the best they could in response to the dominance of the PBM industry.
The committee report “underscores how the health care system has evolved in recent years, exposing some people to higher prices at the pharmacy,” said Lilly’s Kueterman.
“Despite Sanofi paying billions in rebates that lower insulin costs for middlemen, people’s costs at the pharmacy counter have continued to rise,” said the Sanofi spokesman.
And Novo Nordisk’s Bachner maintains, “The information in the committee’s report and its accompanying documentation reflect a limited picture of the efforts put forth by our company and other companies to manage formulary access.”
“This glimpse into the complexity of pricing, formularies, and the healthcare system demonstrates why Novo Nordisk continues to advocate for comprehensive solutions,” he added.
The report details how drug companies set a list price and then use rebates to compete for positions on health plans’ formularies.
The PBMs which negotiate with drug companies on behalf of the health plans have become all powerful, with the three largest, CVS Caremark, Express Scripts, and OptumRx, managing drug benefits for some 250 million Americans, the committee reported.
PBMs play a key role in whether and how drugs are added to a formulary. They generally pass most of a rebate on to health plans, but also retain a portion and charge additional fees based on a percentage of a drug’s list price.
The Astronomical Price Of Insulin Hurts American Families
essay
A woman from Minnesota holds up her U.S. bottle of NovoLog insulin and a Canadian box of NovoRapid, which she bought at a pharmacy in Ontario, Canada, June 29, 2019
Drug companies charge more for insulin in the United States than in nearly three dozen other countries RAND researchers examinedand it’s not even close. The average list price for a unit of insulin in Canada was $12. Step across the border into America, and it’s $98.70.
Those differences help explain why insulin has become a symbol of the high cost of American health care. Its prices have shot up in recent years, for reasons that are opaque at best, with those who can least afford it often paying the most. Reining in those prices has become the rare political cause embraced by Democrats and Republicans alike.
This isn’t just some academic question: ‘How do our prices compare with those in other countries?’ said Andrew Mulcahy, a senior policy researcher at RAND who specializes in health care economics and led the study. It’s becoming a very practical question, because there are ideas out there to do something about it, and they can benefit from this kind of analysis.
The U.S. Department of Health and Human Services asked RAND to investigate how American insulin prices compare with those in other parts of the world. Researchers obtained list prices for all types of insulin from 33 countries in Europe, Asia, Australia, and the Americas. Plotted on a graph, the U.S. prices stand alone.
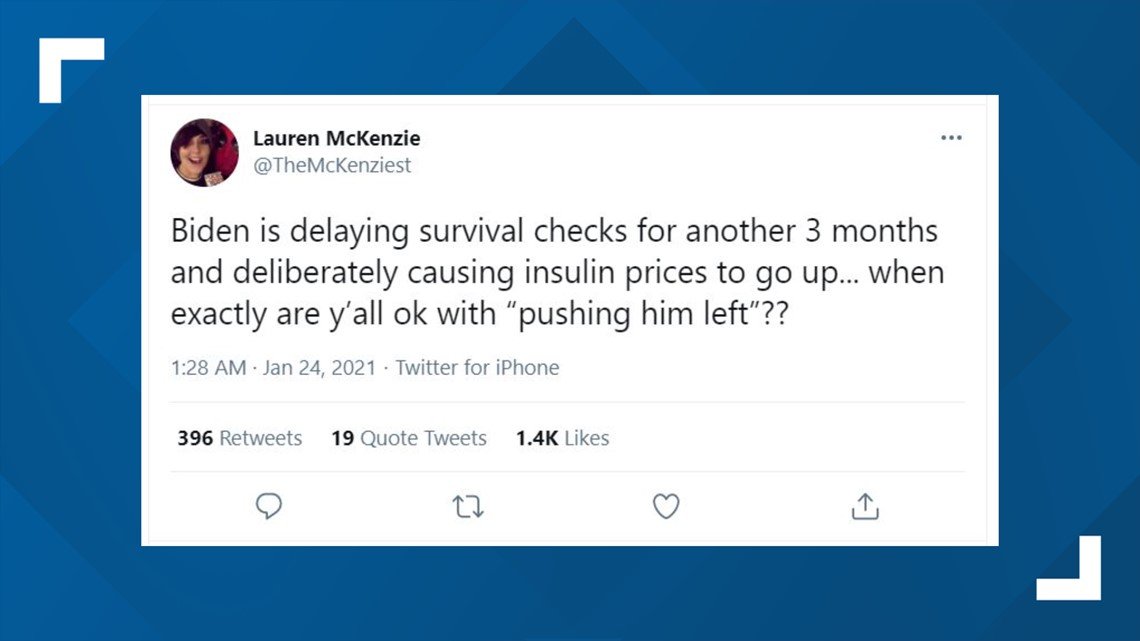
Our Ruling: Missing Context
We rate this claim about the Biden administration’s action to be MISSING CONTEXT, based on our research. Some patients who use insulin and EpiPens the fraction who are served by federally qualified health centers may benefit from Trump’s order, but others could suffer if it results in decreased access for the centers to the 340B drug discount program. Also, the freeze through March 22 does not represent final action on the program, so it’s premature to call it a “reversal.”
You May Like: Greek Yogurt And Diabetes
White House Mandates Pfizer Vaccines For Millions Of Citizens Before The Fda Clinical Or Safety Reviews Have Been Made Public
There have been several initiatives carried out in the commercial sector to address insulin affordability. Last year, for example, the insurer Cigna and its pharmacy benefit management division Express Scripts announced a program designed to cap out-of-pocket costs for diabetic patients at $25 a month.
Moreover, the recent advent of biosimilar insulin products may help reduce out-of-pocket costs, as could the possibility of automatic interchangeability of biosimilar insulin and originator products.
Nevertheless, for a comprehensive approach to improving insulin affordability that reaches a larger number of diabetic patients the federal government would need to get involved, and it has to a certain extent.
Trump Administration has lowered out-of-pocket insulin costs for some
President Trump has made some dubious claims on insulin prices, including one he uttered during a September presidential debate. There, he boasted that he had helped lower the price of insulin to the point that its so cheap, its like water.
Trump also signed an executive order in July that would require federally qualified health centers to share the steep savings they receive through the 340B program with indigent patients, specifically for epinephrine and insulin products. But, this only applies to a very small portion hospitals participating in the 340B program. And, it doesnt resolve the much larger issue that the 340B program discounts arent generally winding up where theyre supposed to.
‘vicious Cycle’ Sent Insulin Costs Through Roof: Senate Committee
Alicia Ault
US insulin manufacturers and the pharmaceutical benefits management industry are refuting a report by a prominent Senate committee finding that the two sectors acted synergistically to increase the cost of insulin for patients with diabetes.
The Senate Committee on Finance issued findings from a 2-year investigation on January 14, releasing a 90-page report and more than 1700 pages of documents containing internal emails, contracts, and presentations.
“We found that the business practices of and the competitive relationships between manufacturers and middlemen have created a vicious cycle of price increases that have sent costs for patients and taxpayers through the roof,” said Committee Chairman Chuck Grassley in a statement.
“This industry is anything but a free market when PBMs spur drug makers to hike list prices in order to secure prime formulary placement and greater rebates and fees,” Grassley said.
Also Check: Advantages And Disadvantages Of Metformin
President Trump Announces Lower Out Of Pocket Insulin Costs For Medicares Seniors
Today, under President Trumps leadership, the Centers for Medicare & Medicaid Services announced that over 1,750 standalone Medicare Part D prescription drug plans and Medicare Advantage plans with prescription drug coverage have applied to offer lower insulin costs through the Part D Senior Savings Model for the 2021 plan year. Across the nation, participating enhanced Part D prescription drug plans will provide Medicare beneficiaries access to a broad set of insulins at a maximum $35 copay for a months supply, from the beginning of the year through the Part D coverage gap. The model follows on the Trump Administrations previously announced 13.5 percent decline in the average monthly basic Part D premium since 2017 to the lowest level in seven years.
Under President Trumps leadership, for the first time, CMS is enabling and encouraging Part D plans to offer fixed, predictable copays for beneficiaries rather than leaving seniors paying 25 percent of the drugs cost in the coverage gap. Both manufacturers and Part D sponsors responded to this market-based solution in force and seniors that use insulin will reap the benefits.
The Part D Senior Savings Model builds on steps the Trump Administration has already taken to strengthen Medicare and improve the quality of care for patients with diabetes. CMS has taken the following actions to address the needs of beneficiaries with diabetes:
Overall Insulin Epipen Pricing Isn’t Affected
Nationally, 30 million Americans suffer from diabetes, according to the American Diabetes Association. And nearly one in 50 Americans are at risk for anaphylaxis brought on by certain foods, insect bites, medications and latex, according to a 2013 study by the Asthma and Allergy Foundation of America.
But not all of those patients require insulin or epinephrine. And most who live in extreme poverty, or less than 200% of the federal poverty level an equation that works out to $34,840 for a family of two already receive free or discounted prescription drugs, a national health policy expert said.
Karyn Schwartz, a senior fellow at the Kaiser Family Foundation, a nonpartisan nonprofit that analyzes health policy, said some patients served by the 1,400 federally backed health centers nationally, such as those with high deductibles or those who are uninsured and paying list prices for the drugs, would have benefitted from the new pricing rule.
But it’s hard to say how many, she said. It’s also difficult to speculate about how many new patients would switch care to a community health center to take advantage of the discounted insulin and EpiPen prices, she said.
Also Check: Metformin Glipizide Combination Side Effects
Dangers Of Insulin Rationing
Alec Smith was diagnosed with type 1 diabetes older than most, at the age of 24. The cost of insulin and other supplies was $250 a month, expensive but bearable.
Then he had to get off his mother’s insurance at the age of 26 and, unable to find a reasonable plan, tried to go to the pharmacy and pay out-of-pocket. The cost was $1,300 for a month’s supply.
“He left without anything, thinking he could make what he had in his supplies last until payday,” says his mother, Nicole Smith-Holt, of Richfield, MN.
“He died about 4 days before his paycheck.”
The cause of death was ketoacidosis, when the body can’t use sugar in the blood for energy so it burns fat and muscle instead, making high levels of acids called ketones build up. Lack of insulin causes ketoacidosis. “Almost on a daily basis, people are reaching out to me , saying they’re facing the same type of struggles. I’m hearing about people who are not able to test their blood sugars on a daily basis,” says Smith-Holt.
Hirsch, the University of Washington doctor, says such cases highlight the dangers of rationing insulin.
“Whether you have type 1 or type 2 diabetes, you are going to end up with higher blood sugars. And over periods of time, that can result in really bad downstream effects. But it’s much worse than that,” he says.
Turning to the black market for insulin could be equally dangerous, and it’s something Hirsch never advises his patients to do.
Others, meanwhile, are taking the industry on.
Debate On The Real Impact Of The Proposal
The executive order signed by former President Trump was meant to require federally qualified health centers who purchase insulins and epinephrine in the 340B program to pass the savings from discounted drug prices directly on to medically underserved patients.
The statement made by the US Health and Human Services about the rule said that the proposal would increase access to life-saving insulin and epinephrine for the patients who face especially high costs among the 28 million patients who visit every year.
The rule was finalized in December of last year. However, upon publishing it, the HHS itself acknowledged that the rules economic impact will most likely be minimal since the majority of patients who get their insulin from community health centers already purchase the medication on a discounted price.
The health centers involved also said the same thing. They stated that they already pass on those savings and they even called the rule an administrative burden that paints them as predators and enemies that price-gouge patients.
Read Also: Disadvantages Of Metformin
What Is The Federal Register
The Office of the Federal Register publishes regulations in the Federal Register, which is considered the official newspaper of the federal government. Executive orders, such as the one in question, are published in the Federal Register to explain how the president has instructed various executive agencies on how to manage operations and gives the public an opportunity to review and comment on them.
In July 2020, Trump signed a series of executive orders that he proposed as a solution for lowering the high premium prices of prescription drugs, including the price of insulin. Per the Executive Order on Access to Affordable Life-Saving Medications, the Department of Health and Human Services is required to enable Americans without access to affordable insulin and injectable epinephrine through commercial insurance or Federal programs, such as Medicare and Medicaid, to purchase these pharmaceuticals from an FQHC at a price that aligns with the cost at which the FQHC acquired the medication.
HHS finalized the rule in late December but acknowledged the economic impact is expected to be minimal since the vast majority of patients who get insulin from Community Health Centers already get discounted medication. In some cases, those patients receive a one-month supply of insulin for just $7, according to the report published in the Federal Register.
Policy Recommendations To Bring Down Insulin Prices
Reed and DeGette in the report recommended 11 policy proposals to address the rising cost of insulin:
- Allow generic drugmakers to manufacturer older, off-patent versions of insulin
- Cap out-of-pocket costs for prescription drugs designed to treat chronic conditions
- Encourage the development of generic insulin products by addressing extensions on patents
- Link a patient’s out-of-pocket costs to negotiated prices instead of list prices
- Promote the development and use of value-based contracts between insulin makers and PBMs
- Promote the use of standardized fees and other payment arrangements instead of rebates between insulin makers and wholesalers
- Restrict the number of changes an insurer can make to a formulary each year
- Require insulin makers, PBMs, and health insurers disclose the value of rebates to other entities in the insulin supply chain
- Require manufacturers disclose how they determine the list price of insulin products
- Standardize the process for patients to challenge formulary restrictions and
- Standardize a process for drug formularies to disclose patient cost-sharing information .
Also Check: How Does High Blood Sugar Feel
How The Companies Justify Their Price Increases
With Type 1 diabetes, which affects about 5 percent of people with diabetes in the US, the immune system attacks the insulin-producing cells in the pancreas, leaving the body with little or none of the hormone. In Type 2 diabetes, the pancreas still makes insulin, but the body has grown resistant to its effects. In both cases, patients rely on insulin medication to keep energy from food flowing into their bodies.
The US is a global outlier on money spent on the drug, representing only 15 percent of the global insulin market and generating almost half of the pharmaceutical industrys insulin revenue. According to a recent study in JAMA Internal Medicine, in the 1990s Medicaid paid between $2.36 and $4.43 per unit of insulin by 2014, those prices more than tripled, depending on the formulation.
The doctors and researchers who study insulin say it is yet another example along with EpiPens and of companies raising the cost of their products because of the lax regulatory environment around drug pricing. They are doing it because they can, Jing Luo, a researcher at Brigham and Womens Hospital, told Vox in 2017, and its scary because it happens in all kinds of different drugs and drug classes.
In countries with single-payer health systems, governments exert much more influence over the entire health care process.
The US doesnt do that. Instead, America has long taken a free market approach to pharmaceuticals.
Committee Found Companies Raised Prices To Balance Out Rebates

To balance out rising rebates, insulin manufacturers in turn “aggressively” raised the list price of their insulin, the committee found.
“The investigation found that Novo Nordisk and Sanofi not only closely monitored the others’ price increases, they actually increased prices in lockstep sometimes within hours or days of each other a practice known as ‘shadow pricing,'” said the committee.
Internal emails also show that in 2014 Lilly executives decided to enact a list price increase for Humalog earlier than expected when the company heard Novo Nordisk had decided to increase list prices for its and Levemir products.
The committee documented list price increases of 50%-70% for insulins, sometimes over just a 3-year period.
The investigation also found after reviewing internal documents that drug makers often set prices based on whether it might harm a PBM’s or health plan’s bottom line. The goal was to keep those clients happy and to preserve market share, said the committee.
PBMs did not do anything to discourage the increases in list prices, said the committee. Instead, “PBMs used their size and aggressive negotiating tactics, like the threat of excluding drugs from formularies, to extract more generous rebates, discounts, and fees from insulin manufacturers.”
The PBM industry’s lobbying group, the Pharmacy Management Care Association , said it shared the committee’s “urgency in addressing affordability and access for insulin-dependent patients,” in a statement.
Also Check: Negative Side Effects Of Metformin
Cdc Cuts Quarantine Time For Health Care Workers With Negative Test
WASHINGTON President Trump on Tuesday will announce a prescription plan drastically reducing the cost of insulin for American seniors who rely on Medicare.
The deal struck with the nations insulin manufacturers and health care providers will limit the co-pay for a months supply of insulin to $35 a 66 percent reduction to current costs, White House counselor Kellyanne Conway said.
The initiative will apply to the 1 in 3 Medicare enrollees who have diabetes, which is approximately 3 million people.
The announcement comes on the heels of hearings into the rising cost of insulin in the United States, with one diabetic groom-to-be dying in 2019 after switching to a cheaper version to help pay for his wedding.
Having more predictable out of pocket costs will help seniors adhere to their doctors orders, Conway told reporters on a briefing call.
The initiative will be unveiled during an event in the White House Rose Garden with Trump and the nations health care executives.
The plan, effective from January 2021, will save seniors approximately 56 percent or an average of $446 each year in insulin co-pays, said Seema Verma, administrator of the Centers for Medicare and Medicaid Services.

