Production Of Hormones To Control Blood Sugar Levels
A small proportion of the pancreas is made up of other types of cells called islets of Langerhans. These cells sit in tiny groups, like small islands, scattered throughout the tissue of the pancreas. The islets of Langerhans contain alpha cells which secrete glucagon and beta cells which secrete insulin.
Insulin and glucagon are hormones that work to regulate the level of sugar in the body to keep it within a healthy range. Unlike the acinar cells, the islets of Langerhans do not have ducts and secrete insulin and glucagon directly into the bloodstream.
Depending on what youve eaten, how much exercise your muscles are doing, and how active your body cells are, the amount of glucose in your bloodstream and cells varies. These 2 hormones have the job of keeping tight control of the amount of glucose in your blood so that it doesnt rise or fall outside of healthy limits.
The Primary Hormones That Are Produced By The Pancreas Include:
- Insulin this hormone works by allowing the bodys cells to absorb glucose from the bloodstream and use it as energy. This in turn helps to reduce high blood sugar levels.
- Gastrin gastrin hormone stimulates specific cells in the stomach that aids in digestion.
- Glucagon this hormone helps insulin to maintain a normal blood sugar level by stimulating the cells to release glucose when it is too low.
- Vasoactive intestinal peptide vasoactive intestinal peptide helps to control absorption and secretion of water from the intestines.
- Somatostatin in case other hormones such as glucagon and insulin are too high, the hormone somatostatin will be released to help maintain blood sugar.
I The Dual Nature Of The Pancreas
The pancreas is a complex gland active in digestion and metabolism through secretion of digestive enzymes from the exocrine portion and hormones from the endocrine portion. The exocrine pancreas, which accounts for more than 95-98% of the pancreas mass , is structurally comprised of lobules, with acinar cells surrounding a duct system. The endocrine pancreas makes up only 2% of the pancreatic mass and is organized into the islets of Langerhans small semi-spherical clusters of about 1500 cells dispersed throughout the pancreatic parenchyme which produce and secrete hormones critical for glucose homeostasis. The existence of islets was described by Paul Langerhans in 1869, and the functional role of islets in glucose homeostasis was first demonstrated in 1890 when Joseph von Mering and colleagues showed that dogs developed diabetes mellitus following pancreatectomy . Though islet mass may vary between individualsan example is the increase in the setting of adult obesity the average adult human pancreas is estimated to contain one to two million islets . In humans, the concentration of islets is up to two times higher in the tail compared to the head and neck. However, the cellular composition and architectural organization of cell types within the islets is preserved throughout the pancreas .
Read Also: What To Do If A Diabetic Feels Dizzy
The Discovery Of Insulin
In 1889 German scientists Minkowski and von Mering noted, from their experimental work with animals, that total pancreatectomy led to the development of severe diabetes. They hypothesised that a substance secreted by the pancreas was responsible for metabolic control. Others later refined this hypothesis, noting diabetes to be associated with destruction of the islets of Langerhans. While Minkowski, as well as Zuelzer in Germany and Scott in the USA attempted, with inconsistent results, to isolate and administer the missing pancreatic islet substance, Belgian investigator de Meyer in 1909 proposed the name insuline, as did British researcher Schaefer in 1916.
What Are The Drawbacks To Insulin Treatment For Diabetes
The biggest issue with insulin right now is unaffordability. A box of rapid-acting insulin can cost $400 without insurance. As so many people continue to lose their health coverage, its becoming an enormous problem, Dr. Zilbermint says.
Consistently rising costs have led some patients to ration their insulin, which can be dangerous and even deadly. The cost of testing strips is also an issue, and both have led to a black market in testing strips and insulin. Its illegal, says Dr. Zilbermint, but its happening.
You May Like: How Long Do Type 1 Diabetics Live
Physiology Of Insulin Secretion
Glucose is the principal stimulus for insulin secretion, though other macronutrients, hormones, humoral factors and neural input may modify this response. Insulin, together with its principal counter-regulatory hormone glucagon, regulates blood glucose concentrations. Pancreatic cells secrete 0.251.5 units of insulin per hour during the fasting state, sufficient to enable glucose insulin-dependent entry into cells. This level prevents uncontrolled hydrolysis of triglycerides and limits gluconeogenesis, thereby maintaining normal fasting blood glucose levels. Basal insulin secretion accounts for over 50% of total 24 hour insulin secretion. Following secretion of insulin into the portal venous system, 60% is subsequently removed by the liver so portal vein insulin concentrations reaching the liver approach triple that of the peripheral circulation. In healthy lean individuals circulating venous fasting insulin concentrations are about 315 mIU/L or 1890 pmol/L. Meal-related insulin secretion accounts for the remaining fraction of the total daily output.
Epinephrine Cortisol And Growth Hormone:
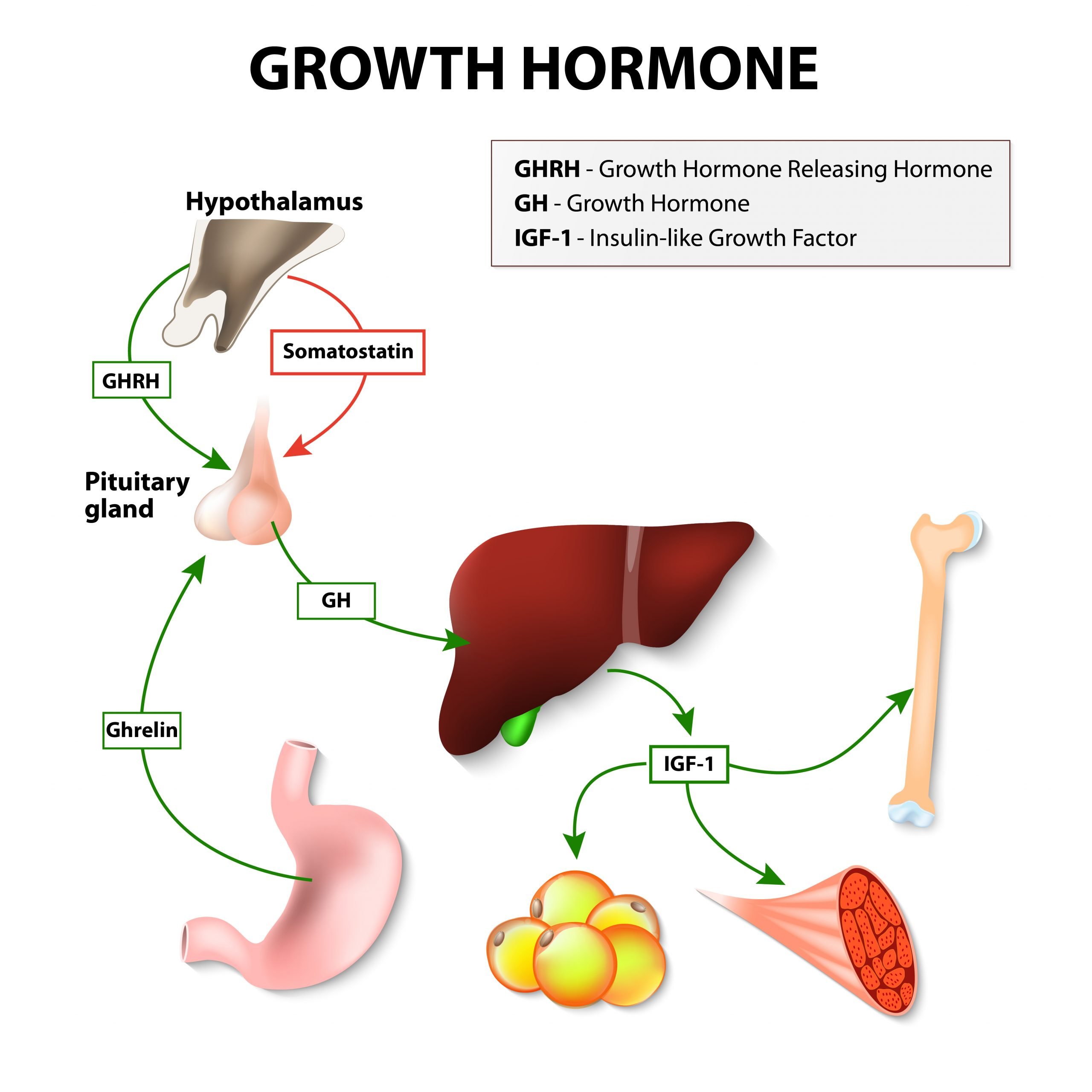
Epinephrine, cortisol, and growth hormone are other hormones that help maintain blood sugar levels. They, along with glucagon are called stress or gluco-counter-regulatory hormones which means they make the blood sugar rise.
Epinephrine is released from nerve endings and the adrenals, and acts directly on the liver to promote sugar production . Epinephrine also promotes the breakdown and release of fat nutrients that travel to the liver where they are converted into sugar and ketones.
Cortisol is a steroid hormone also secreted from the adrenal gland. It makes fat and muscle cells resistant to the action of insulin, and enhances the production of glucose by the liver. Under normal circumstances, cortisol counterbalances the action of insulin. Under stress or if a synthetic cortisol is given as a medication , cortisol levels become elevated and you become insulin resistant. When you have Type 1 diabetes, this means your may need to take more insulin to keep your blood sugar under control.
Growth Hormone is released from the pituitary, which is a part of the brain. Like cortisol, growth hormone counterbalances the effect of insulin on muscle and fat cells. High levels of growth hormone cause resistance to the action of insulin.
Don’t Miss: What Is A Normal A1c For A Non Diabetic
Who Gets Type 2 Diabetes
What makes people more likely to develop type 2 diabetes? No one knows for sure. But experts have a few ideas about what puts a person at greater risk:
- Most people who have type 2 diabetes are overweight.
- People with family members who have diabetes get diabetes more often.
- People who are older than 10 are more likely to develop type 2 diabetes than younger kids.
What Are The Signs & Symptoms Of Type 2 Diabetes
People who have type 2 diabetes may not know it because the symptoms aren’t always obvious and they can take a long time to develop. Some people don’t have any symptoms at all.
But when a person gets type 2 diabetes, he or she may:
- pee a lot because the body tries to get rid of the extra blood sugar by passing it out of the body in the urine
- drink a lot to make up for all that peeing
- feel tired all the time because the body can’t use sugar for energy properly
Also, people whose bodies are having problems using insulin or who are overweight may notice something called acanthosis nigricans. This can cause a dark ring around the neck that doesn’t wash off, as well as thick, dark, velvety skin under the arms, in between fingers and toes, between the legs, or on elbows and knees. This skin darkening can lighten over time with improvement in insulin resistance.
In addition, girls with insulin resistance may have polycystic ovary syndrome . In PCOS, the ovaries get bigger and develop fluid-filled sacs called cysts. Girls with this condition often have irregular periods or may stop having periods, and they might have excess facial and body hair.
Read Also: What Is A High Blood Sugar Reading
What Will Insulin Be Like In The Future
Pharmaceutical companies are working on very long-acting versions of insulin that could last for a week. There is also an ultra-fast version of insulin under development that will act in less than 15 minutes.
Another group of researchers is looking at glucose responsive insulin , which would react to the needs of your body in real time. It would have nanosensors bound to the insulin so that when insulin is needed, it releases, and when it isnt, it stops, according to Dr. Hirsch.
Hormones Of The Pancreas
Regulation of blood glucose is largely done through the endocrine hormones of the pancreas, a beautiful balance of hormones achieved through a negative feedback loop. The main hormones of the pancreas that affect blood glucose include insulin, glucagon, somatostatin, and amylin.
Insulin lowers BG levels, whereas glucagon elevates BG levels.
Somatostatin is formed in the delta cells of the pancreas and acts as the pancreatic policeman, balancing insulin and glucagon. It helps the pancreas alternate in turning on or turning off each opposing hormone.
Amylin is a hormone, made in a 1:100 ratio with insulin, that helps increase satiety, or satisfaction and state of fullness from a meal, to prevent overeating. It also helps slow the stomach contents from emptying too quickly, to avoid a quick spike in BG levels.
In a healthy liver, up to 10% of its total volume is used for glycogen stores. Skeletal muscle cells store about 1% of glycogen. The liver converts glycogen back to glucose when it is needed for energy and regulates the amount of glucose circulating between meals. Your liver is amazing in that it knows how much to store and keep, or break down and release, to maintain ideal plasma glucose levels. Imitation of this process is the goal of insulin therapy when glucose levels are managed externally. Basalbolus dosing is used as clinicians attempt to replicate this normal cycle.
Test Your Knowledge
Apply Your Knowledge
Online Resource
You May Like: What Is The First Sign Of Diabetes
Mechanisms Of Insulin Secretion
Increased levels of glucose induce the first phase of glucose-mediated insulin secretion by release of insulin from secretory granules in the cell. Glucose entry into the cell is sensed by glucokinase, which phosphorylates glucose to glucose-6-phosphate , generating ATP. Closure of K+-ATP-dependent channels results in membrane depolarization and activation of voltage dependent calcium channels leading to an increase in intracellular calcium concentration this triggers pulsatile insulin secretion. Augmentation of this response occurs by both a K+-ATP channel-independent Ca2+-dependent pathway and K+-ATP channel-independent Ca2+-independent pathways of glucose action. Other mediators of insulin release include activation of phospholipases and protein kinase C and by stimulation of adenylyl cyclase activity and activation of cell protein kinase A, which potentiates insulin secretion. This latter mechanism may be activated by hormones, such as vasoactive intestinal peptide , PACAP, GLP-1, and GIP. These factors appear to play a significant role in the second phase of glucose mediated insulin secretion, after refilling of secretory granules translocated from reserve pools.
Chemical Coordination And Integration Class 11 Mcqs Questions With Answers
Solving the Chemical Coordination and Integration Multiple Choice Questions of Class 11 Biology Chapter 22 MCQ can be of extreme help as you will be aware of all the concepts. These MCQ Questions on Chemical Coordination and Integration Class 11 with answers pave for a quick revision of the Chapter thereby helping you to enhance subject knowledge. Have a glance at the MCQ of Chapter 22 Biology Class 11 and cross-check your answers during preparation.
I. Select the correct answer from the following questions:
Question 1.Blood pressure is under the control of Pituitary
Also Check: What Is A Normal A1c For A Non Diabetic
Insulin Receptors And Insulin Binding
Insulin mediates its actions through binding to insulin receptors. The insulin receptor was first characterised in 1971. It consists of a heterotetramer consisting of 2 and 2 glycoprotein subunits linked by disulphide bonds and is located on the cell membrane. The gene coding for the insulin receptor is located on the short arm of chromosome 19. Insulin binds to the extracellular subunit, resulting in conformational change enabling ATP to bind to the intracellular component of the subunit. ATP binding in turn triggers phosphorylation of the subunit conferring tyrosine kinase activity. This enables tyrosine phosphorylation of intracellular substrate proteins known as insulin responsive substrates . The IRS can then bind other signalling molecules which mediate further cellular actions of insulin.
PI 3-kinase promotes the translocation of glucose transporter proteins, glycogen, lipid and protein synthesis, anti-lipolysis and the control of hepatic gluconeogenesis. PI 3-kinase acts via serine and threonine kinases such as Akt/protein kinase B , protein kinase C and PI dependent protein kinases1& 2 . The RAS pathway activates transcription factors and stimulates the growth promoting actions of insulin. Thus broadly, PI 3-kinase mediates insulins metabolic effects, e.g. cellular glucose uptake, while RAS significantly mediates insulins mitogenic effects, together with other less well described actions. These pathways are presented schematically in .
Insulin Secretion In Response To Stimuli
Response to Glucose
In healthy individuals glucose stimulated pancreatic secretion is biphasic. Intravenous administration of glucose is associated with a rapid first phase of insulin release within 1 minute, peaking at 35 minutes, and lasting about 10 minutes the slower onset second phase of insulin secretion begins shortly after the glucose bolus but is not apparent until 10 minutes later, lasts the duration of the hyperglycaemia and is proportional to the glucose concentration immediately prior to the glucose administration. The first phase of insulin secretion represents release of insulin already synthesised and stored in secretory granules the second phase represents secretion of both stored and newly synthesised insulin. Overall insulin secretion relates to the total dose of glucose and its rate of administration maximal pancreatic response occurs with 20 g of glucose given intravenously over 3 minutes in humans.
In contrast to the reproducible pattern of insulin secretion in response to intravenous glucose, insulin secretion following oral glucose is much more variable. With an oral glucose load, gastric emptying and gastrointestinal motility affect glucose absorption, gastro-intestinal hormones and neural input associated with glucose ingestion modify the insulin response, and insulin secretion continues some time after glucose ingestion.
Response to Arginine
Effects of Lipids
Response to Mixed Meal
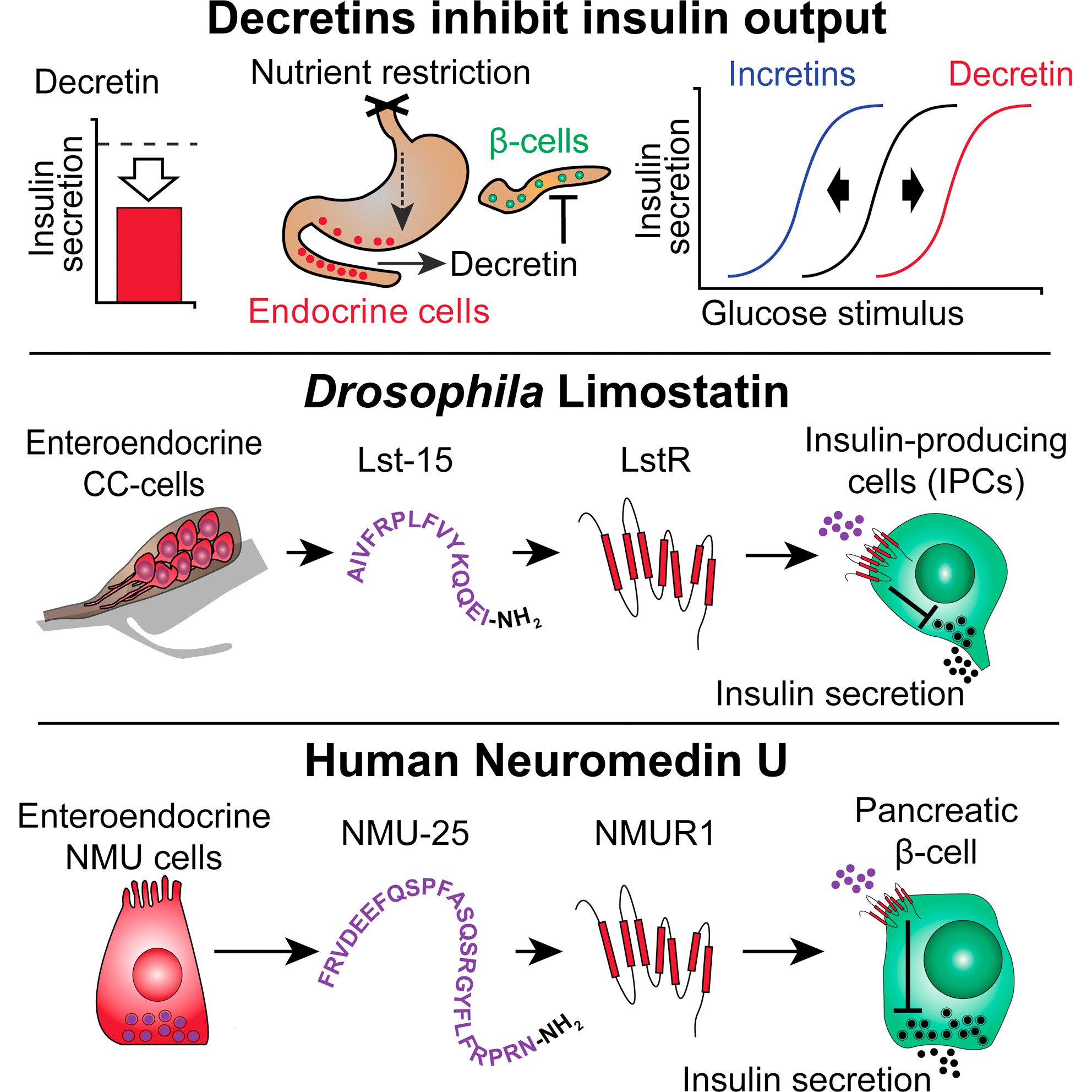
Incretin Hormones
Effects of Neural and Hormonal Stimuli
Recommended Reading: Which Pancreatic Cells Release Insulin And Glucagon
What Is The Function Of The Pancreas
A pancreas that is functioning normally produces chemicals which are responsible for digesting food that we eat. The pancreas plays a role in two different systems, that is the exocrine system and the endocrine system. The exocrine tissue in the pancreas secretes an alkaline fluid that consists of several enzymes. These enzymes work by breaking down the food we eat into small particles that can be absorbed by the intestines.
Iii Insulin Gene Transcription
The insulin gene on chromosome 11 is primarily expressed in pancreatic b cells, but is expressed in low levels in the brain, thymus, and in the yolk sak during fetal development . It has three exons and two introns, and its transcription results in the 446 base pair preproinsulin mRNA .
Figure 1. Various levels of glucose regulation of insulin gene expression. Glucose stimulates nuclear translocation of Pdx-1 promotes Pdx-1 and MafA phosphorylation and binding to the insulin promoter and stimulates transcription of the insulin gene, pre-mRNA splicing, translation, and mRNA stability. ).
Transcription of the insulin gene to preproinsulin mRNA is sophisticated and reflects the tight regulation by transcription factors and recruited coactivators. Pdx-1, NeuroD1 and MafA are important transcription factors in b cell function, respond to elevated glucose levels. Individual b cells respond to ambient glucose with differential insulin secretion, and these changes are apparent at the level of gene transcription . At the level of the islet, rapid increase in blood glucose results in rapid elevation in preproinsulin mRNA in the endocrine pancreas. A rapid decrease in blood glucose results in a slow decline in preproinsulin mRNA.
This is due to the unusual stability of preproinsulin mRNA, further stabilized by increased glucose concentrations . The specific regulation of this molecules translation is the primary mechanism of insulin production control .
Read Also: How Long Do Type 1 Diabetics Live
When The Blood Glucose Level Goes Up
- Blood sugar rises
- The pancreas detects the rise
- The pancreas pumps out insulin into the blood
- Insulin helps the uptake of glucose into muscles and other cells
- This causes the blood glucose level to fall to its normal set point and
- The pancreas detects the fall and switches off insulin production.
V Insulin Secretory Pathway
The pancreatic b-cells act as a self-contained system to secrete insulin in response to changes in ambient blood glucose concentration, in order to maintain glucose homeostasis. Glucose is freely taken up into the b-cell via GLUT transporters, metabolized to produce ATP, which triggers a cascade of signals within the b cell necessary for glucose-induced insulin secretion. While GLUT2 has been traditionally assumed as the major mediator of glucose uptake into b-cells based on extrapolation from rodent studies and subsequent confirmation of GLUT2 transporters on human -cells , more recent studies in human islets suggest that the other insulin-independent glucose transporters GLUT1 and GLUT3 play a more important role, and are the main glucose transporters in human islet -cells . This redundancy explains why individuals with variants in the gene encoding GLUT2 do not have significant abnormalities in insulin secretion .
Figure 4. Diagrammatic illustration of insulin secretion. A low background secretion exists upon which is superimposed insulin secretory bursts stimulated by food intake. ).
Also Check: Is Greek Yogurt Good For Diabetics

