Testing For Type 1 Diabetes
The incidence and prevalence of type 1 diabetes is increasing . Type 1 diabetic patients often present with acute symptoms of diabetes and markedly elevated blood glucose levels, and some are diagnosed with life-threatening ketoacidosis. Several studies suggest that measuring islet autoantibodies in relatives of those with type 1 diabetes may identify individuals who are at risk for developing type 1 diabetes. Such testing, coupled with education about diabetes symptoms and close follow-up in an observational clinical study, may enable earlier identification of type 1 diabetes onset. There is evidence to suggest that early diagnosis may limit acute complications and extend long-term endogenous insulin production .
A recent study reported the risk of progression to type 1 diabetes from the time of seroconversion to autoantibody positivity in three pediatric cohorts from Finland, Germany, and the U.S. Of the 585 children who developed more than two autoantibodies, nearly 70% developed type 1 diabetes within 10 years and 84% within 15 years . These findings are highly significant because, while the German group was recruited from offspring of parents with type 1 diabetes, the Finnish and American groups were recruited from the general population. Remarkably, the findings in all three groups were the same, suggesting that the same sequence of events led to clinical disease in both sporadic and genetic cases of type 1 diabetes.
How Do Doctors Diagnose Insulin Resistance And Prediabetes
Doctors use blood tests to find out if someone has prediabetes, but they dont usually test for insulin resistance. The most accurate test for insulin resistance is complicated and used mostly for research.
Doctors most often use the fasting plasma glucose test or the A1C test to diagnose prediabetes. Less often, doctors use the oral glucose tolerance test , which is more expensive and not as easy to give.
The A1C test reflects your average blood glucose over the past 3 months. The FPG and OGTT show your blood glucose level at the time of the test. The A1C test is not as sensitive as the other tests. In some people, it may miss prediabetes that the OGTT could catch. The OGTT can identify how your body handles glucose after a mealoften before your fasting blood glucose level becomes abnormal. Often doctors use the OGTT to check for gestational diabetes, a type of diabetes that develops during pregnancy.
People with prediabetes have up to a 50 percent chance of developing diabetes over the next 5 to 10 years. You can take steps to manage your prediabetes and prevent type 2 diabetes.
The following test results show Prediabetes2
- A1C5.7 to 6.4 percent
- FPG100 to 125 mg/dL
- OGTT140 to 199 mg/dL
You should be tested for prediabetes if you are overweight or have obesity and have one or more other risk factors for diabetes, or if your parents, siblings, or children have type 2 diabetes. Even if you dont have risk factors, you should start getting tested once you reach age 45.
Possible Complications For The Baby
Unlike type 1 diabetes, gestational diabetes generally occurs too late to cause birth defects. Birth defects usually originate sometime during the first trimester of pregnancy. The insulin resistance from the contra-insulin hormones produced by the placenta does not usually occur until approximately the 24th week. Women with gestational diabetes mellitus generally have normal blood sugar levels during the critical first trimester.
The complications of GDM are usually manageable and preventable. The key to prevention is careful control of blood sugar levels just as soon as the diagnosis of diabetes is made.
Infants of mothers with gestational diabetes are vulnerable to several chemical imbalances, such as low serum calcium and low serum magnesium levels, but, in general, there are two major problems of gestational diabetes: macrosomia and hypoglycemia:
Blood glucose is monitored very closely during labor. Insulin may be given to keep the mother’s blood sugar in a normal range to prevent the baby’s blood sugar from dropping excessively after delivery.
Recommended Reading: What Produces Insulin And Glucagon
Sodiumglucose Cotransporter 2 Inhibitors
Sodiumglucose cotransporter 2 inhibitors act on the kidney to reduce blood levels of glucose and are used to treat T2DM. In patients with T2DM, treatment with SGLT2is reduced infiltration of inflammatory cells into arterial plaques and decreased the mRNA expression levels of some cytokines and chemokines, such as TNF, IL-6 and monocyte chemoattractant protein 1 . However, SGLT2i treatment can cause ketoacidosis, especially in critically ill patients. Importantly, SGLT2is have profound effects on urinary glucose and sodium excretion, resulting in osmotic diuresis and potentially dehydration, and increased urinary uric acid excretion, which has been suggested to be a risk factor for acute kidney injury through both urate crystal-dependent and crystal-independent mechanisms. As such, the use of SGLT2is might be difficult in patients under critical care, who need meticulous control of their fluid balance. In addition, these drugs must be discontinued in the face of a reduced estimated glomerular filtration rate, which limits their glucose-lowering effects substantially, and will be a typical risk in critically ill patients. Nonetheless, an international study is ongoing to evaluate the effect of dapagliflozin versus placebo, given once daily for 30;days, in reducing disease progression, complications and all-cause mortality in all patients admitted with COVID-19 . The result of this study might help reveal the implications of the use of SGLT2is in such patients.
Insulin Resistance Treatment And Prevention
You can take steps to reverse insulin resistance and prevent type 2 diabetes:
- Exercise. Go for at least 30 minutes a day of moderate activity 5 or more days a week. If you’re not active now, work up to that.
- Get to a healthy weight. If you’re not sure what you should weigh or how to reach a weight loss goal, ask your doctor. You may also want to talk with a nutritionist and a certified personal trainer.
- Eat a healthy diet. Think fruits, vegetables, whole grains, nuts, beans, fish, legumes, and other lean protein.
- Take medications. Your doctor may prescribe a medication called metformin to help keep your blood sugar in check.
Don’t Miss: Can Diabetics Eat Dominos Pizza
Thromboembolic Risk In Patients With Diabetes Mellitus
Several publications have reported an increased thromboembolic risk among patients with diabetes mellitus outside the specific situation of SARS-CoV-2 infection. For example, a population-based study found that patients with T2DM exhibited an increased risk of venous thromboembolism compared with controls . Furthermore, the risks of pulmonary embolism were greater in the patients with T2DM than in the controls . Another study found that the incidence of deep vein thrombosis after total knee replacement was statistically significantly higher in patients with diabetes mellitus than in those without. Diabetes mellitus was also found to be associated with an increase of more than twofold in the risk of ulcer formation after DVT. Thus, patients with diabetes mellitus are already in a high-risk category for a thromboembolic event or stroke,.
To prevent such complications, patients with diabetes mellitus who are at risk of SARS-CoV-2 infection should try not to be sedentary for long periods, as regular physical activity is associated with decreased incidence of thromboembolism. Instead, these individuals should try to engage in physical activity to improve blood circulation. Appropriate simple exercises for performance at home are available and effective and should be recommended. Patients who experience pain in their legs, shortness of breath or chest pain must not hesitate to contact their physician owing to suspected thromboembolic complications.
Pathogenesis Of Insulin Resistance In Skeletal Muscle
Muhammad A. Abdul-Ghani
1Division of Diabetes, University of Texas Health Science Center at San Antonio, 7703 Floyd Curl Dr, San Antonio, TX 78229, USA
Academic Editor:
Abstract
Insulin resistance in skeletal muscle is manifested by decreased insulin-stimulated glucose uptake and results from impaired insulin signaling and multiple post-receptor intracellular defects including impaired glucose transport, glucose phosphorylation, and reduced glucose oxidation and glycogen synthesis. Insulin resistance is a core defect in type 2 diabetes, it is also associated with obesity and the metabolic syndrome. Dysregulation of fatty acid metabolism plays a pivotal role in the pathogenesis of insulin resistance in skeletal muscle. Recent studies have reported a mitochondrial defect in oxidative phosphorylation in skeletal muscle in variety of insulin resistant states. In this review, we summarize the cellular and molecular defects that contribute to the development of insulin resistance in skeletal muscle.
1. Introduction
| Insulin signaling | Reduced insulin receptor tyrosine phosphorylation |
| Impaired GLUT 12 translocation | |
| Glucose metabolism | |
| Impaired glycogen synthase |
2. Normal Skeletal Muscle Metabolism
3. Insulin Resistance in Skeletal Muscle
3.2.1. Long-Chain Fatty Acid Transport into the Muscle
4.9. Glycolysis
Read Also: What Happens If A Diabetic Eats Too Much Sugar
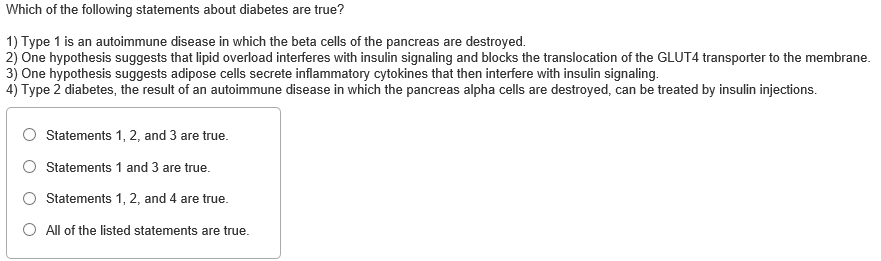
Which Of The Following Is Not True Of Insulin A It Is
Correct; insulin resistance does not result in extremely rapids rates of lipolysis in adipose tissue, b, TRUE or FALSE: Atrial natriuretic peptide is a hormone that controls blood pressure in part by increasing the urinary excretion of sodium, hormonal changes occur as one leaves the fed state and enters the fasting state, Many competing insulin products were established previously under the Hatch-Waxman Act, TRUE OR FALSE? A,Which of the following is true about insulin products and the BPCIA? The BPCIA now governs a large variety of insulin and human growth hormone products, Glucagon increases and increases lipolysis.TRUE or FALSE: Most type 2 diabetics do not produce insulin, Mixtures of insulin can sometimes be combined in the same syringe, produced in pancreas by the beta cells of the islets of Langerhans that is important for regulating the amount of glucose in the blood, Insulin converts glucose into glycogen in the liver and muscles, It is released into the blood when blood glucose is high, Concerning this system, Insulin
What Causes Insulin Resistance
Scientists are beginning to get a better understanding of how insulin resistance develops. For starters, several genes have been identified that make a person more or less likely to develop the condition. It’s also known that older people are more prone to insulin resistance. Lifestyle can play a role, too. Being sedentary, overweight or obese increases the risk for insulin resistance. Why? It’s not clear, but some researchers theorize that extra fat tissue may cause inflammation, physiological stress or other changes in the cells that contribute to insulin resistance. There may even be some undiscovered factor produced by fat tissue, perhaps a hormone, that signals the body to become insulin resistant.
Doctors don’t usually test for insulin resistance as a part of standard diabetes care. In clinical research, however, scientists may look specifically at measures of insulin resistance, often to study potential treatments for insulin resistance or type 2 diabetes. They typically administer a large amount of insulin to a subject while at the same time delivering glucose to the blood to keep levels from dipping too low. The less glucose needed to maintain normal blood sugar levels, the greater the insulin resistance.
Also Check: Regular Insulin Patient Teaching
Insulin Resistance In The Bipoc Community
according to a March 2019 study in Diabetes and Vascular Disease Research.according to a systematic review and meta-analysis in Diabetes Care.
- 5 percent of non-Hispanic whites
- 2 percent of Asian Americans
- 7 percent of non-Hispanic blacks
- 5 percent of Hispanics
- 7 percent of American Indians/Alaskan Natives
More on Health Disparities Affecting BIPOC Individuals
What Causes Gestational Diabetes Mellitus
Although the cause of GDM is not known, there are some theories as to why the condition occurs.
The placenta supplies a growing fetus with nutrients and water, and also produces a variety of hormones to maintain the pregnancy. Some of these hormones can have a blocking effect on insulin. This is called contra-insulin effect, which usually begins about 20 to 24 weeks into the pregnancy.
As the placenta grows, more of these hormones are produced, and the risk of insulin resistance becomes greater. Normally, the pancreas is able to make additional insulin to overcome insulin resistance, but when the production of insulin is not enough to overcome the effect of the placental hormones, gestational diabetes results.
You May Like: What Happens If A Type 2 Diabetic Stops Taking Insulin
Classification And Diagnosis Of Diabetes
Diabetes can be classified into the following general categories:
Type 1 diabetes
Type 2 diabetes
Gestational diabetes mellitus
Specific types of diabetes due to other causes, e.g., monogenic diabetes syndromes , diseases of the exocrine pancreas , and drug- or chemical-induced diabetes
This section reviews most common forms of diabetes but is not comprehensive. For additional information, see the American Diabetes Association position statement Diagnosis and Classification of Diabetes Mellitus .
Assigning a type of diabetes to an individual often depends on the circumstances present at the time of diagnosis, with individuals not necessarily fitting clearly into a single category. For example, some patients cannot be clearly classified as having type 1 or type 2 diabetes. Clinical presentation and disease progression may vary considerably in both types of diabetes.
What Are The Symptoms Of Insulin Resistance And Prediabetes
Insulin resistance and prediabetes usually have no symptoms. Some people with prediabetes may have darkened skin in the armpit or on the back and sides of the neck, a condition called acanthosis nigricans. Many small skin growths called skin tags often appear in these same areas.
Even though blood glucose levels are not high enough to cause symptoms for most people, a few research studies have shown that some people with prediabetes may already have early changes in their eyes that can lead to retinopathy. This problem more often occurs in people with diabetes.
Don’t Miss: Can Type 2 Diabetics Eat Bananas
What Are The Risks Factors Associated With Gestational Diabetes Mellitus
Although any woman can develop GDM during pregnancy, some of the factors that may increase the risk include the following:
-
Overweight or obesity
-
Family history of diabetes
-
Having given birth previously to an infant weighing greater than 9 pounds
-
Race
-
Prediabetes, also known as impaired glucose tolerance
Although increased glucose in the urine is often included in the list of risk factors, it is not believed to be a reliable indicator for GDM.
Symptoms Of Insulin Resistance
You can’t tell that you have insulin resistance by how you feel. You’ll need to get a blood test that checks your blood sugar levels.
Likewise, you wonât know if you have most of the other conditions that are part of insulin resistance syndrome without seeing your doctor.
Some signs of insulin resistance include:
- A waistline over 40 inches in men and 35 inches in women
You May Like: What Happens If You Stop Taking Diabetes Medication
Use Of Antidiabetic Medications
Based on the data from previous basic and clinical studies and the most recent information available from current publications, we propose some guidelines for the use of glucose-lowering medications in patients with T2DM and COVID-19, according to the clinical status of COVID-19, which is based on the WHO clinical progression scale . Few published recommendations exist for the use of these medications during the COVID-19 pandemic. In patients with COVID-19, we should be prepared for acute hyperglycaemia , and we face the need to provide appropriate glycaemic control effectively and rapidly. The choice of agents should be guided mainly by their presumed effectiveness and by potential or actual adverse effects. In line with the review by Drucker, we recommend DPP4is and GLP1 analogues in patients with mild to moderate symptoms because these agents have proven glucose-lowering efficacy in hospital settings, as well as in outpatient clinics. However, insufficient data are available to support the use of these agents instead of insulin in critically ill patients with T2DM and COVID-19, especially if the therapy needs to be initiated under conditions of severe illness . The anti-inflammatory actions of DPP4is and GLP1 analogues suggest the need for clinical trials with such agents in patients with T2DM and COVID-19.
Fig. 4: Use of antidiabetic medications in patients with T2DM and COVID-19.
What Is The Treatment For Gestational Diabetes Mellitus
Specific treatment for gestational diabetes will be determined by your doctor based on:
-
Your age, overall health, and medical history
-
Extent of the disease
-
Your tolerance for specific medications, procedures, or therapies
-
Expectations for the course of the disease
-
Your opinion or preference
Treatment for gestational diabetes focuses on keeping blood glucose levels in the normal range. Treatment may include:
-
Special diet
-
Insulin injections
You May Like: What Is A Normal A1c For A Non Diabetic
Factors Influencing Insulin Biosynthesis And Release
Insulin secretion may be influenced by alterations in synthesis at the level of gene transcription, translation, and post-translational modification in the Golgi as well as by factors influencing insulin release from secretory granules. Longer-term modification may occur via influences on cell mass and differentiation. Given insulins pivotal role in glucose utilisation and metabolism, it is not surprising that glucose has multiple influences on insulin biosynthesis and secretion. However, other factors such as amino acids, fatty acids, acetylcholine, pituitary adenylate cyclase-activating polypeptide , glucose-dependent insulinotropic polypeptide , glucagon-like peptide-1 , and several other agonists, together in combination, also influence these processes.
Cellular Mechanisms Of Insulin Resistance
In relation to external factors, the increase in free fatty acids induced by obesity can trigger insulin resistance through lipid accumulation . This may activate atypical PKC that inhibits insulin signaling and insulin-stimulated glucose uptake in skeletal muscles, as well as decreases the insulin-stimulated hepatic glycogen synthesis . This can lead to insulin resistance and increased glucose delivery by the liver . Additionally, FFA triggers insulin resistance by direct activation of Toll-like Receptor 4 and the innate immune response .
Furthermore, obesity is associated with inflammatory factors characterized by an increase in the accumulation of ATMs . The inflammatory factors increase lipolysis and promote hepatic triglyceride synthesis, and hyperlipidemia due to increased fatty acid esterification. ATM also stimulates inflammatory cytokines that inhibit insulin signaling and expedites hepatic gluconeogenesis, and postprandial hyperglycemia .
Don’t Miss: What Do You Do If You Take Too Much Insulin

