Diabetic Blisters May Heal On Their Own
Its rare, but sometimes people with diabetes erupt in blisters . The blisters occur on the backs of fingers, hands, toes, feet, and sometimes on the legs or forearms. These skin sores resemble burn blisters. Having diabetic neuropathy puts you at higher risk of developing these blisters. Heres the good news: They are usually painless and heal on their own in a few weeks. Keeping blood glucose under control is the only treatment for this diabetes skin problem.
What Causes Dry Skin On Feet
These cracks commonly develop on the heels while dry feet can take place on any part of the foot due to reasons like neurological disorders, usage of hard soaps, unsuitable shoes for the skin and prolonged standing on hard floors
- The sweat glands of the feet are destroyed due to years of prolonged standing and being excessively overweight as it causes additional pressure on the feet.
- Too much of hot showers, hot baths or foot baths can lead to dry feet as exposure to hot water leads to breaking down of the natural skin barriers allowing moisture to escape resulting to excessive dry skin on feet.
- Medical patients of Diabetics and hypothyroidism have less sweating, increasing dryness of the skin. Diabetics patients experience damage in the nerves of the feet. Dry skin makes its way due to uncontrolled blood sugar. The natural moisture of the skin is affected with poor blood supply and gives rise to complications in the body.
- Dry climate leads to dry skin as it removes the moisture in the skin like in the winter season you might face the maximum skin problems.
- Skin problems with atopic and psoriasis lead in developing dry and rough patches affecting the skin.
- Swimming in chlorinated pools harms the natural moisture of the body.
- Hormonal imbalances due to aging increases dry skin as it loses the elasticity and lipids in process like menopause.
Following are the two pictures of dry skin on feet:
Close up photo of a person with dry skin on heel
Cracked skin on foot
The Connection Between Diabetes And Itchy Skin
Diabetes can make the body lose too much fluid through urination and evaporation through the skin. The result: dry, itchy skin that can be bothersome and sometimes uncomfortable.
Itching, especially in the lower legs and feet, can also be caused by poor circulation, which is common with diabetes. Some people experience a skin reaction to their diabetes medication or insulin injections.
In addition, itching can be brought on by diabetes complications including nerve damage, kidney disease and liver disease. Certain medications for other health problems common in people with diabetes, such as high blood pressure and high cholesterol, can make the skin itchy, too.
Scientists suspect that those with type 2 diabetes may be vulnerable to itchy skin for yet another reason: Their skins barrier function is impaired. Exactly how and why this happens is still being studied.
Recommended Reading: How Long Does It Take To Lower Blood Sugar With Medication
What You Can Do For Softer Supple Skin:
- Keep your blood glucose and blood pressure in your target range.
- See a podiatrist routinely and for anything that bothers you.
- Use a humidifier in areas with low humidity and during the winter months.
- Be a detective. Talk with your healthcare provider about other causes for dry skin, such as those listed above. Once youve detected what the problem is, together you can make up a plan to improve your skin.
- Age healthfully. Theres nothing you can do to turn back the clock, but you can prevent complications and live a healthier life by managing your diabetes.
- You can also keep your skin moist but applying your moisturizer while your skin is damp to lock in the moisture.
NOTE: The information is not intended to be a replacement or substitute for consultation with a qualified medical professional or for professional medical advice related to diabetes or another medical condition. Please contact your physician or medical professional with any questions and concerns about your medical condition.
Diabetes Can Affect Every Part Of The Body Including The Skin
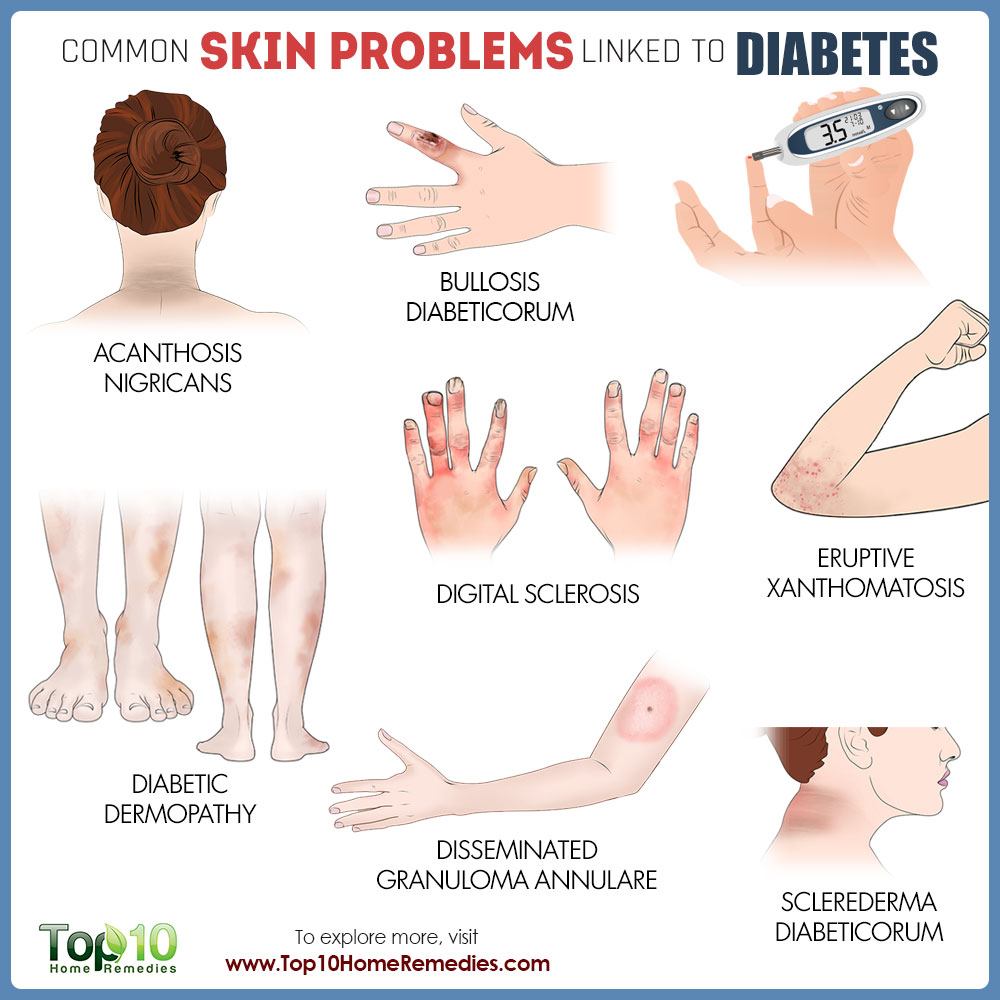
In fact, skin problems are sometimes the first sign that a person has diabetes.
Some are cause for concern, while others may simply be a cosmetic issue . Regardless, you should keep an eye out for changes in your skin and talk to your doctor about any concerns you haveits better to be safe than sorry. Luckily, most skin conditions can be prevented or easily treated if caught early.
Some of these problems are skin conditions anyone can have, but people with diabetes get more easily. These include bacterial infections, fungal infections, and itching. Other skin problems happen mostly, or only, to people with diabetes. These include diabetic dermopathy, necrobiosis lipoidica diabeticorum, diabetic blisters, and eruptive xanthomatosis. Expand the items below to learn more about each skin condition and discover helpful skin care tips.
You May Like: Can I Eat Sugar While Taking Metformin
Diabetes Dry Skin Best Remedies
Both type 1 diabetes and type 2 diabetes can be associated with skin problems, including dry skin. No one knows exactly why dry skin is associated with diabetes but most diabetic experts agree that things like diabetic dry skin conditions can be easily managed with simple tips, including the following:
Vitiligo Causes Skin To Lose Color
Vitiligo is a skin problem in which the skin cells that make melanin are destroyed, leading to irregular, blotchy patches that often occur on the hands, face, or chest. Although the cause of vitiligo is unknown, experts believe it is an autoimmune condition like type 1 diabetes, and research published in July 2016 in BioMed Research International described the link between the two conditions. There’s no cure, but light therapy and steroids are used to manage vitiligo. If you have the condition, it’s important to wear a sunscreen of at least 30 SPF, since depigmented skin has no natural sun protection.
You May Like: What Is A Normal A1c Level Non Diabetic
Allergic Reactions To Medications
Nearly any diabetes medicationincluding insulincan trigger an allergic reaction that brings on symptoms that affect the skin, such as itching, swelling, rash, or redness.
Why it happens: Allergic reactions to medications occur because a person has a pre-existing sensitivity to either the drug itself or to an inactive ingredient in the drug, such as a preservative. Some people who use injectable medications experience skin reactions that are limited to the area where the needle was inserted.
What to do: Call your healthcare provider if you have an allergic reaction to a diabetes medication. He or she may instruct you to take an over-the-counter medication to relieve itching in the short term, and then will discuss trying a different drug to treat your diabetes.
If skin changes brought on by medication are accompanied by difficulty breathing or other alarming symptoms, get emergency help immediately.
Diabetes: 12 Warning Signs That Appear On Your Skin
Diabetes can affect many parts of your body, including your skin. When diabetes affects the skin, its often a sign that your blood sugar levels are too high. This could mean that:
-
You have undiagnosed diabetes, or pre-diabetes
-
Your treatment for diabetes needs to be adjusted
If you notice any of the following warning signs on your skin, its time to talk with your doctor.
Don’t Miss: Therapeutic Effect Of Insulin
What Are Common Skin Changes That I May See
- A smooth, dark thickness in the skin on your neck, groin, face, and underarms
- Dry, flaky skin
- Skin tags on your eyelids, neck, or underarms
- Yellow color of your palms, soles of your feet, and nails
- Dark patches on your shins
- A constant redness of your face and neck
- Thick skin on the back of your hands and the top of your feet
How To Protect Your Skin If You Have Diabetes
You know what you’re up againstnow for some solutions. Your first step should be to work with your doctor to effectively control and manage your blood glucose levels. In turn, that can help with many of the skin complications that are a side effect of diabetes.
Dr. Hu also recommends using gentle skin cleansers and non-irritating moisturizers that are rich in emollients every day. This will help reduce skin dryness or itchiness, according to Dr. Hu. She also recommends avoiding abrasive scrubs and exfoliators.
Another important habit is to carefully inspect your feet on a daily basis. “This can protect from a break in the skin going unnoticed until a serious wound develops,” says Dr. Beckman. Gently washing and drying your feet is one of the best routines to get into, he says. If you spot an injury in the process, it’s important to take it seriously and reach out to your doctor for advice.
If you notice injuries on other parts of your body, Dr. Beckman suggests cleansing the injured area with good soapy water, applying an antibiotic ointment, and putting on a bandage or dressing to protect it from further harm.
You May Like: Diabetic Too Much Sugar
Use Topical Antibiotics Liberally
Have a topical antibiotic cream available at all times and use it whenever you have a cut or tear in the skin. Whenever a cut or tear occurs, wash the skin carefully and apply topical antibiotic creams to prevent infection from occurring. If this doesnt work to treat an infection of the skin, see your doctor about using an oral antibiotic to treat the infection.
How Can I Prevent Diabetes

The best thing you can do to prevent skin problems is to keep blood sugar levels within the range recommended by your healthcare provider. Proper skin care can lower your chances of getting a skin rash, infection or wound thats difficult to heal.
Take these steps to prevent skin problems:
- Check your skin daily for signs of rashes, redness, infections or sores.
- Use warm water and moisturizing soap in the shower.
- Pat skin dry with a towel , making sure to dry in between fingers, toes and skin folds.
- Apply fragrance-free moisturizers after showering while skin is still damp and soft. Look for creams and ointments with ceramide to help skin retain moisture.
- Apply creams containing 10% to 25% urea to cracked, dry heels at bedtime.
- Prevent dehydration and keep skin hydrated by drinking plenty of fluids.
- Treat cuts and wounds immediately with soap and water. Use antibiotic ointments only if your healthcare provider gives the OK. Bandage the wound daily. Call your provider if you notice signs of redness, pain, drainage or infection.
- Use a humidifier to add moisture to the air in your home.
A note from Cleveland Clinic
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services.Policy
Also Check: High Blood Sugar Symptoms Type 2
Can Diabetics Use A Foot Peel
It’s common knowledge that diabetes is often associated with skin problems. From ensuring your skin is dry to looking for sores, diabetes takes a toll on your feet’ health.
To combat dry and rough skin, a variety of top brands introduced foot peels. The innovative solution boasts exfoliating properties that help rid your feet off of peeling and cracking skin. However, the plethora of different chemicals included in the peel makes people with diabetes wonder whether they should use it or not. Here we discuss what foot peels are and if diabetic people can utilize them:
Can Diabetics Use a Foot Peel at a Glance
Yes and no. Depending on the foot peel you choose, the foot peel can either soften your skin or worsen your skin condition.
Checking the label to read about the ingredients employed allows you to make an informed decision.
What is Foot Peel?
Foot peels, otherwise known as exfoliating socks, refer to state-of-the-art plastic socks boasting remarkable mixtures. These naturally break down your dead skin with time. In turn, it eliminates dead cells and calluses from your heel.
Typically, you slip your feet in the sock and wait for an hour as your feet absorb the solution. Then you remove them and throw the socks away.
What Does it Contain?
Brand to brand, your foot peel may contain a plethora of contrasting ingredients. Typically, foot peels claim to utilize nothing but natural products that promise visible and positive results.
How Does it Work?
A Cooling Cream
A Skin Balm
Recognize Diabetic Nerve Damage
If you are suffering from diabetic neuropathy , you will need to take special care to manage your dry skin. With diabetic nerve damage, you may not be aware of dry skin conditions and you have an increased likelihood of having cracks in the skin that can get infected. If you have dry skin and diabetic nerve damage, youll need to check the skin of your lower extremities every day to make sure that you havent developed any type of crack or tear in the skin that you didnt notice because of numbness secondary to neuropathy.
Don’t Miss: How Long Can A Person Live With Diabetes
Solutions For Addressing Dry Skin
To help prevent dry skin, use a moisturizer daily. Some moisturizers are marketed specifically for people with diabetes. These products may contain ingredients called emollients that help keep the skin moist and feel smooth. Others may feature humectants that help draw moisture from the dermis to the epidermis , occlusives that hold water into the skin to minimize moisture evaporation, or a combination of these ingredients. Moisturizers can include additional additives like aloe vera, which may help soothe some skin discomforts. You can also find skin care products that contain over-the-counter anti-itch medications.
Good Blood Sugar Control Treats Digital Sclerosis
About a third of people with type 1 diabetes have digital sclerosis thick, tight, waxy skin that develops on the backs of the hands. The finger joints stiffen and become difficult to move. Sometimes this skin problem occurs on the toes and forehead as well. Rarely, knees, ankles, or elbows may stiffen. Again, good blood glucose control is the only treatment. Moisturizer may help soften the skin.
Recommended Reading: Side Effect Of Glucophage 500 Mg
Control The Blood Sugar Numbers
If your blood sugar is out of control, you will have a greater likelihood of suffering from dry skin. In order to get your diabetes under control, youll need to watch what you eat, try and achieve a healthy weight, decrease salt intake, maintain a normal blood pressure, and exercise to maintain a healthy weight.
Acanthosis Nigricans Turns Skin Dark And Velvety
Acanthosis nigricans causes skin problems in body folds and turns the skin creases dark, thick, and velvety. This diabetes skin problem usually develops in people who are very overweight. Theres no cure, but losing weight may improve the skins appearance. If you have the skin problem and havent been diagnosed with diabetes, talk to your doctor. Acanthosis nigricans usually appears before diabetes strikes.
Recommended Reading: Metformin Dosage Range
Poor Blood Flow Results In Itchy Skin
Itchy skin can have many causes. In people with diabetes, a yeast infection, dry skin, or poor circulation can be the root cause. When poor blood flow is the culprit, the lower legs may be the itchiest part of the body. What can you do to stop your skin from crawling? Consider bathing less often, and use mild soap when you do. Slather on some lotion to moisturize dry skin, but avoid applying it between your toes.
Discover Tips To Add To Your Skin Care Regime

If you have diabetes then youre more likely to have dry skin, which can lead to itchiness. Are you one of those who suffer with diabetes and itchy skin? Itchy skin and diabetes often go together. The good news is that by taking care of your skin, you may be able to help reduce the risk of developing skin problems due to dryness and maintain healthy-looking, smooth skin.
Tips and Tricks to Help Diabetic Skin Problems
Expert Advice The advice in this article does not constitute medical advice, it is solely available for information purposes.
You May Like: How Does It Feel When Your Blood Sugar Is High
Diabetic Treatment Suggestions For Dry Skin
Dry skin, a frequently overlooked complication of diabetes, is an irritating side effect of chronically high blood glucose levels. Try these tricks to keep your skin healthy and soft.
Say Goodbye to Dry Skin
Everyone gets dry skin from time to time. But for people with diabetes, it can be a chronic problem if your blood glucose levels are regularly high. High blood glucose causes the body to lose fluids at a faster rate. Skin can also become dry when nerves are damaged from years of diabetes and don’t get the message to sweat.
Tip: Outdoor Exercise Ideas for Diabetes-That You’ll Actually Look Forward To
For people with diabetes, dry skin can become more than an irritation — it can be dangerous. When skin is dry, it sloughs off easier, and often the outer layer is lost. This outer layer is your skin’s first defense against bacteria and acts as a barrier. And because bacteria feed on glucose, people with diabetes whose blood glucose isn’t in control have a higher risk of bacterial infection — the bacteria are literally on a feeding frenzy in the higher glucose levels. That’s why even the tiniest cut can become a major infection when your glucose levels are regularly high.
Experts say it’s vital to keep a close eye on your skin. If you identify a cut, scratch, or burn early, it’s possible to avoid major complications such as an amputation.

