Iii Insulin Gene Transcription
The insulin gene on chromosome 11 is primarily expressed in pancreatic b cells, but is expressed in low levels in the brain, thymus, and in the yolk sak during fetal development . It has three exons and two introns, and its transcription results in the 446 base pair preproinsulin mRNA .
Figure 1. Various levels of glucose regulation of insulin gene expression. Glucose stimulates nuclear translocation of Pdx-1 promotes Pdx-1 and MafA phosphorylation and binding to the insulin promoter and stimulates transcription of the insulin gene, pre-mRNA splicing, translation, and mRNA stability. ).
Transcription of the insulin gene to preproinsulin mRNA is sophisticated and reflects the tight regulation by transcription factors and recruited coactivators. Pdx-1, NeuroD1 and MafA are important transcription factors in b cell function, respond to elevated glucose levels. Individual b cells respond to ambient glucose with differential insulin secretion, and these changes are apparent at the level of gene transcription . At the level of the islet, rapid increase in blood glucose results in rapid elevation in preproinsulin mRNA in the endocrine pancreas. A rapid decrease in blood glucose results in a slow decline in preproinsulin mRNA.
This is due to the unusual stability of preproinsulin mRNA, further stabilized by increased glucose concentrations . The specific regulation of this molecules translation is the primary mechanism of insulin production control .
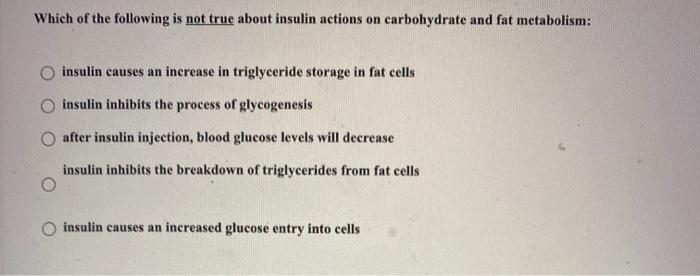
Muscle And Fat Storage
Insulin helps your muscles and fat cells store extra glucose so it doesnt overwhelm your bloodstream.
It signals your muscle and fat tissue cells to stop breaking down glucose to help stabilize your blood sugar level.
The cells then begin creating glycogen, the stored form of glucose. Glycogen provides your body with energy when your blood sugar level drops.
When your liver can hold no more glycogen, insulin triggers your fat cells to take in glucose. Its stored as triglycerides, a type of fat in your blood, that can be used for energy later.
How Is Type 2 Diabetes Treated
Sometimes people with type 2 diabetes take pills that help the insulin in their bodies work better. Some also need insulin shots or an insulin pump to control their diabetes.
People with type 2 diabetes have to pay a little more attention to what they’re eating and doing than people who don’t have diabetes. They may need to:
- Eat a healthy diet, as determined by the care team.
- Get regular physical activity to achieve a healthy weight and allow insulin to work more effectively.
- Check their blood sugar levels on a regular basis.
- Get treatment for other health problems that can happen more often in people with type 2 diabetes, like high blood pressure or problems with the levels of fats in their blood.
- Have regular checkups with doctors and other people on their diabetes health care team so they can stay healthy and get treatment for any diabetes problems.
People with type 2 diabetes might have to eat smaller food portions and less salt or fat, too. Those who eat healthy foods, stay active, and get to a healthy weight may bring their blood sugar levels into a healthier range. Their doctors may even say they don’t need to take any medicines at all.
Don’t Miss: Diabetes Ribbon Colors
Vi Regulation Of Insulin Release
Insulin release from pancreatic b cells is tightly regulated, and allows the sensitive response of insulin levels to calorigenic nutrients in the body. Glucose, free fatty acids, and amino acids serve as fuel stimuli for insulin release, promoting insulin granule exocytosis. Additional hormonal factors influence the regulation pathway. Pharmacological agents can also be used to augment insulin release.
A. Glucose-stimulated insulin secretion
Figure 5. Hyperglycemic clamp illustration. Example of hyperglycemic clamp testing in obese adolescents with normal glucose tolerance , impaired glucose tolerance , and type 2 diabetes . In the hyperglycemic clamp in healthy, non-diabetic individuals, glucose concentration is briskly elevated by administering a suitable intravenous glucose infusion at time 0. This elicits a rapid and short-lived insulin secretion peak due to release of preformed insulin vesicles, followed by a drop towards basal levels and then by a relatively rapid return to a sustained increase in insulin in the second half of the clamp as dextrose infusion is continued. This example illustrates the loss, in first and second phase insulin secretion, as individual progress from normal to impaired glucose tolerance, to type 2 diabetes. In the latter, the first phase insulin response is essentially lost and the second phase insulin response is reduced. ).
B. Proteins and Amino Acids
C. Lipids and Free Fatty Acids
D. Incretin Hormones
What’s It Like For Teens With Type 2 Diabetes
Sometimes people who have diabetes feel different from their friends because they need to think about how they eat and how to control their blood sugar levels every day.
Some teens with diabetes want to deny that they even have it. They might hope that if they ignore diabetes, it will just go away. They may feel angry, depressed, or helpless, or think that their parents are constantly worrying about their diabetes management.
If you’ve been diagnosed with type 2 diabetes, it’s normal to feel like your world has been turned upside down. Your diabetes care team is there to provide answers and support. Don’t hesitate to ask your doctors, dietitian, and other treatment professionals for advice and tips. It also can help to find support groups where you can talk about your feelings and find out how other teens cope.
Diabetes brings challenges, but teens who have it play sports, travel, date, go to school, and work just like their friends.
Also Check: Treatment Of Hypertension In Diabetes
Infection Prevention During Blood Glucose Monitoring And Insulin Administration
The Centers for Disease Control and Prevention has become increasingly concerned about the risks for transmitting hepatitis B virus and other infectious diseases during assisted blood glucose monitoring and insulin administration.
CDC is alerting all persons who assist others with blood glucose monitoring and/or insulin administration of the following infection control requirements:
- Fingerstick devices should never be used for more than one person
- Whenever possible, blood glucose meters should not be shared. If they must be shared, the device should be cleaned and disinfected after every use, per manufacturers instructions. If the manufacturer does not specify how the device should be cleaned and disinfected then it should not be shared.
- Insulin pens and other medication cartridges and syringes are for single-patient-use only and should never be used for more than one person
Monitoring of blood glucose levels is frequently performed to guide therapy for persons with diabetes. Blood glucose monitoring and insulin administration can be accomplished in two ways: self-monitoring of blood glucose and insulin administration, where the individual performs all steps of the testing and insulin administration themselves, and assisted monitoring of blood glucose and insulin administration, where another person assists with or performs testing and insulin administration for an individual.
- Hospitals or clinics
- Schools or camps
V Insulin Secretory Pathway
The pancreatic b-cells act as a self-contained system to secrete insulin in response to changes in ambient blood glucose concentration, in order to maintain glucose homeostasis. Glucose is freely taken up into the b-cell via GLUT transporters, metabolized to produce ATP, which triggers a cascade of signals within the b cell necessary for glucose-induced insulin secretion. While GLUT2 has been traditionally assumed as the major mediator of glucose uptake into b-cells based on extrapolation from rodent studies and subsequent confirmation of GLUT2 transporters on human -cells , more recent studies in human islets suggest that the other insulin-independent glucose transporters GLUT1 and GLUT3 play a more important role, and are the main glucose transporters in human islet -cells . This redundancy explains why individuals with variants in the gene encoding GLUT2 do not have significant abnormalities in insulin secretion .
Figure 4. Diagrammatic illustration of insulin secretion. A low background secretion exists upon which is superimposed insulin secretory bursts stimulated by food intake. ).
Don’t Miss: Max Dose For Metformin
Vii Insulins Counterregulatory Hormones
The tight control of energy utilization and stores by insulin is balanced by the counterregulatory hormones glucagon, pancreatic polypeptide, somatostatin, cortisol, catecholamines, and growth hormone. There is asymmetry in the glucose regulation hormones, as insulin is the only hormone to prevent against hyperglycemia, while at least three other hormones prevent hypoglycemia. Collectively, these counter-regulatory hormones act to promote glucose release from the liver by glycogenolysis and gluconeogenesis, and inhibit glucose storage during times of starvation.
Mechanisms explaining glucagon secretion are not as well understood as those of insulin secretion, although the direct effect of reduced glucose on cAMP , and the sodium-glucose cotransporters are thought to play a role in a-cell glucose transport . Mice and human data suggest that a-cell inhibition can occur, at least in part, due to the paracrine action of somatostatin from d-cells as a result of gap junction-dependent activation by adjacent b-cells .
Cortisol antagonizes insulins function by promoting protein catabolism to provide amino acid substrate for gluconeogenesis and also impairs peripheral insulin-mediated glucose uptake.
Somatostatin is released from pancreatic islet d cells and exerts inhibitory effect on pancreatic b cells. Once bound to specific somatostatin receptors, b cell membrane repolarization is induced, resulting in reduction of calcium influx and thereby inhibiting insulin release .
How Should I Store My Insulin
- Keep current insulin at room temperature to help alleviate injection discomfort.
- Insulin can usually be stored at room temperature for about a month. Once in use, insulin pens should be stored at room temperature. Expiration dates of insulin pens can vary depending upon the type of insulin. For disposable pens, you should discard the entire device when empty or when you reach the expiration date.
- Store extra insulin in the refrigerator.
- Dont expose insulin to excessive cold or heat.
Read Also: Eating Too Many Carbs On Metformin
What Severe Complications Can Occur Because Of Rationing Or Running Out Of Insulin
Diabetic ketoacidosis is an emergency condition that results if you dont have enough insulin to regulate your blood sugar. DKA causes your body to break down fat for energy in the absence of insulin. This leads to a dangerous accumulation of acids known as ketones in your blood that can cause your brain to swell and your body to go into shock.
Signs of diabetic ketoacidosis include:
- Thirst or a very dry mouth
- Frequent urination
- High levels of ketones in your urine
- Fatigue
- Nausea, vomiting, or stomach pain
- Difficulty breathing
- A fruity or acetone odor on your breath
- Confusion or acting drunk while sober
DKA is so common and can come on so quickly that it is the first sign of Type 1 diabetes in 20% of cases, and the way many type 1 diabetics are first diagnosed with the condition. If you go into diabetic ketoacidosis, dont try to hide it or make light of it. Treat it as the emergency it is and get to a hospital as soon as possible to recover. Ive had people tell me theyre tired of taking insulin, or that theyre rationing it due to cost. In type 1 diabetes, thats all it takes to end up in a life-threatening situation, says Dr. Zilbermint.
Viii Pharmacologic Modulators Of Insulin Response
There is a plethora of pharmcologic agents designed to target various aspects of glucose metabolism. In this chapter, we provide examples of pharmacologic agents that directly or indirectly modulate insulin response.
A. Incretin mimetics
Diabetes therapeutics have recently utilized the role of incretin hormones for pharmacologic benefit. Due to the desirable effect of GLP-1 on hemoglobin A1c reduction and weight loss , GLP-1 receptor agonists and inhibitors of its degradation via dipeptidyl peptidase-4 inhibitors, have been used to treat type 2 diabetes since 2005.
Short-acting GLP-1 receptor agonists , and long-acting GLP-1 receptor agonists potentiate insulin secretion and reduce gastric motility . Given that GLP-1 receptor agonists potentiate glucose-induced insulin gene transcription, they, alone, do not induce hypoglycemia when used as monotherapy .
DPP-4 inhibitors can significantly increase the peak post-prandial concentration of GLP-1 . Additionally, sitagliptin has been found to potentiate GSIS independently of GLP-1 via islet peptide tyrosine tyrosine .
B. Sulfonylureas
C. Insulin Sensitizers
D. Diazoxide
Diazoxide is a sulfonamide pharmacological agent used in treatment of hyperinsulinism, insulinoma, and hypoglycemia due to overtreatment with sulfonylureas. It works by opening b cell membrane potassium ATP channels, hyperpolarizing the b cells, thus decreasing intracellular calcium concentration and inhibiting insulin secretion .
Don’t Miss: Ginger Ale And Diabetes
How Is Type 2 Diabetes Diagnosed
Doctors can say for sure if a person has diabetes by testing blood samples for glucose. Even if someone doesn’t have any symptoms of type 2 diabetes, doctors may order blood tests to check for it if the person has certain risk factors .
Some kids and teens with diabetes may go to a pediatric endocrinologist â a doctor who specializes in diagnosing and treating children and teens living with diseases of the endocrine system, such as diabetes and growth problems.
p
Types Of Insulin Administration With Needles Pumps Pens And Why Insulin Is So Expensive
What does insulin do? Help your body turn food into energy, for starters. When you have diabetes, and youre either not producing insulin or your insulin function is off, all sorts of things can go wrong. From needles to pens to pumps to types of insulin, were here to empower you with clear answers to all your pressing questions.
In This Article:
Alvin Powers, MD, Mihail Zilbermint, MD, and Irl Hirsch, MD
Also Check: Is Metformin A Diuretic
Summarize The Role Of Impaired Insulin Secretion
Impaired insulin secretion renders the woman unable to meet the requirement for greater insulin production necessitated by the insulin resistance and increased hepatic glucose production. These same pathophysiologic disorders, which are in large part genetically determined, make the patient with GDM more likely to develop type 2 diabetes mellitus later in life when weight gain and aging often contribute further to insulin resistance and impaired insulin secretion. Pregnancy can be thought of as a stress test for the development of type 2 diabetes, because the marked insulin resistance of pregnancy necessitates a two- to threefold increase in insulin secretion that the beta cell may not be able to achieve, resulting in a clinically evident abnormality in glucose metabolism.
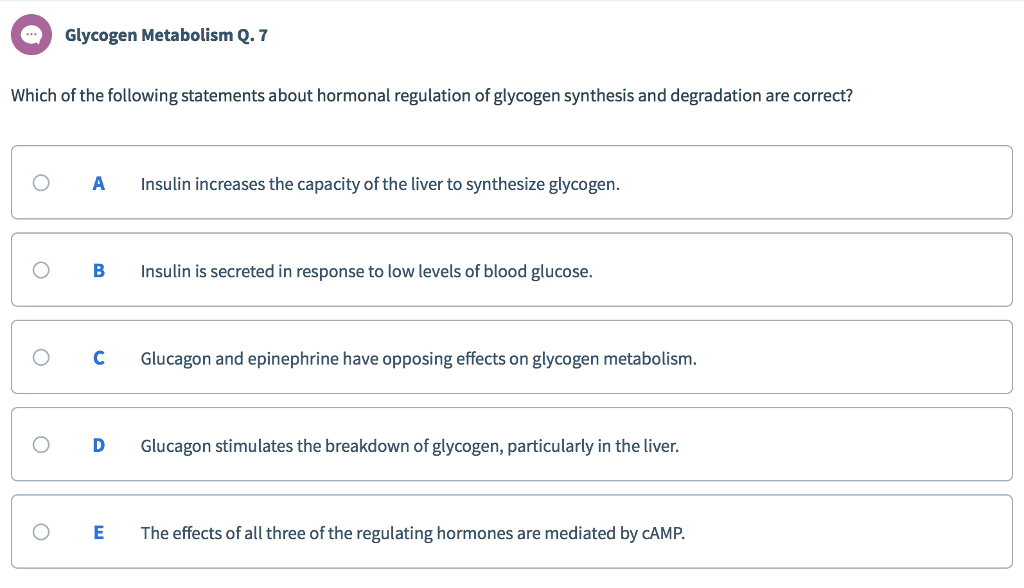
Regulation Of Blood Glucose Levels By Insulin And Glucagon
Glucose is required for cellular respiration and is the preferred fuel for all body cells. The body derives glucose from the breakdown of the carbohydrate-containing foods and drinks we consume. Glucose not immediately taken up by cells for fuel can be stored by the liver and muscles as glycogen, or converted to triglycerides and stored in the adipose tissue. Hormones regulate both the storage and the utilization of glucose as required. Receptors located in the pancreas sense blood glucose levels, and subsequently the pancreatic cells secrete glucagon or insulin to maintain normal levels.
Glucagon
Receptors in the pancreas can sense the decline in blood glucose levels, such as during periods of fasting or during prolonged labor or exercise ). In response, the alpha cells of the pancreas secrete the hormone glucagon, which has several effects:
- It stimulates the liver to convert its stores of glycogen back into glucose. This response is known as glycogenolysis. The glucose is then released into the circulation for use by body cells.
- It stimulates the liver to take up amino acids from the blood and convert them into glucose. This response is known as gluconeogenesis.
- It stimulates lipolysis, the breakdown of stored triglycerides into free fatty acids and glycerol. Some of the free glycerol released into the bloodstream travels to the liver, which converts it into glucose. This is also a form of gluconeogenesis.
Insulin
| Hormones of the Pancreas |
|---|
You May Like: Glucagon Inhibits Insulin
Energy Creation And Distribution
The function of insulin is to help transform glucose into energy and distribute it throughout your body, including the central nervous system and cardiovascular system.
Without insulin, cells are starved for energy and must seek an alternative source. This can lead to life threatening complications.
Cells And Secretions Of The Pancreatic Islets
The pancreatic islets each contain four varieties of cells:
- The alpha cell produces the hormone glucagon and makes up approximately 20 percent of each islet. Glucagon plays an important role in blood glucose regulation low blood glucose levels stimulate its release.
- The beta cell produces the hormone insulin and makes up approximately 75 percent of each islet. Elevated blood glucose levels stimulate the release of insulin.
- The delta cell accounts for four percent of the islet cells and secretes the peptide hormone somatostatin. Recall that somatostatin is also released by the hypothalamus , and the stomach and intestines also secrete it. An inhibiting hormone, pancreatic somatostatin inhibits the release of both glucagon and insulin.
- The PP cell accounts for about one percent of islet cells and secretes the pancreatic polypeptide hormone. It is thought to play a role in appetite, as well as in the regulation of pancreatic exocrine and endocrine secretions. Pancreatic polypeptide released following a meal may reduce further food consumption however, it is also released in response to fasting.
Read Also: Can Metformin Raise Blood Sugar
What Happens If I Have Too Little Glucagon
Unusual cases of deficiency of glucagon secretion have been reported in babies. This results in severely low blood glucose which cannot be controlled without administering glucagon.
Glucagon can be given by injection to restore blood glucose lowered by insulin . It can increase glucose release from glycogen stores more than insulin can suppress it. The effect of glucagon is limited, so it is very important to eat a carbohydrate meal once the person has recovered enough to eat safely.

