What Is The Role Of The Rdn In Medication Adjustment
RDNs providing MNT in diabetes care should assess and monitor medication changes in relation to the nutrition care plan. Along with other diabetes care providers, RDNs who possess advanced practice training and clinical expertise should take an active role in facilitating and maintaining organization-approved diabetes medication protocols. Use of organization-approved protocols for insulin and other glucose-lowering medications can help reduce therapeutic inertia and/or reduce the risk of hypoglycemia and hyperglycemia .
Effectiveness Of Diabetes Nutrition Therapy
Consensus recommendations
-
Refer adults living with type 1 or type 2 diabetes to individualized, diabetes-focused MNT at diagnosis and as needed throughout the life span and during times of changing health status to achieve treatment goals. Coordinate and align the MNT plan with the overall management strategy, including use of medications, physical activity, etc., on an ongoing basis.
-
Refer adults with diabetes to comprehensive diabetes self-management education and support services according to national standards.
-
Diabetes-focused MNT is provided by a registered dietitian nutritionist/registered dietitian , preferably one who has comprehensive knowledge and experience in diabetes care.
-
Refer people with prediabetes and overweight/obesity to an intensive lifestyle intervention program that includes individualized goal-setting components, such as the Diabetes Prevention Program and/or to individualized MNT.
-
Diabetes MNT is a covered Medicare benefit and should be adequately reimbursed by insurance and other payers or bundled in evolving value-based care and payment models.
-
DPP-modeled intensive lifestyle interventions and individualized MNT for prediabetes should be covered by third-party payers or bundled in evolving value-based care and payment models.
How Should Nutrition Therapy Vary Based On Type And Intensity Of Insulin Plan
For people with type 1 diabetes using basal-bolus insulin therapy, a primary focus for MNT should include guidance on adjusting insulin based on anticipated dietary intake, particularly carbohydrate intake recent or expected physical activity and glucose data. Intensive insulin management education programs that include nutrition therapy have been shown to improve A1C and quality of life . For people using fixed daily insulin doses, carbohydrate intake on a day-to-day basis should be consistent with respect to time and amount per meal .
You May Like: What Is A High Blood Sugar Reading
Remission Through A Low Calorie Energy Deficit Diet
The permanence of these changes was tested by a nutritional and behavioural approach to achieve long term isocaloric eating after the acute weight loss phase.39 It was successful in keeping weight steady over the next six months of the study. Calorie restriction was associated with both hepatic and pancreatic fat content remaining at the low levels achieved. The initial remission of type 2 diabetes was closely associated with duration of diabetes, and the individuals with type 2 diabetes of shorter duration who achieved normal levels of blood glucose maintained normal physiology during the six month follow-up period. Recently, 46% of a UK primary care cohort remained free of diabetes at one year during a structured low calorie weight loss programme .40 These results are convincing, and four years of follow-up are planned.
A common criticism of the energy deficit research has been that very low calorie diets may not be achievable or sustainable. Indeed, adherence to most diets in the longer term is an important challenge.24 However, Look-AHEAD, the largest randomised study of lifestyle interventions in type 2 diabetes , randomised individuals to intensive lifestyle management, including the goal to reduce total calorie intake to 1200-1800 kcal/d through a low fat diet assisted by liquid meal replacements, and this approach achieved greater weight loss and non-diabetic blood glucose levels at year 1 and year 4 in the intervention than the control group.41
Can Diabetes Be Prevented Or Avoided
Talk to your doctor about your risk factors for diabetes. Although you may not be able to change all of them, you can make changes to significantly lower your risk.
- Exercise and weight control. Exercising and maintaining a healthy weight can reduce your risk of diabetes. Any amount of activity is better than none. Try to exercise for 30 to 60 minutes most days of the week. Always talk with your doctor before starting an exercise program.
- Diet. A diet high in fat, calories, and cholesterol increases your risk of diabetes. A poor diet can lead to obesity and other health problems. A healthy diet is high in fiber and low in fat, cholesterol, salt, and sugar. Also, remember to watch your portion size. How much you eat is just as important as what you eat.
Read Also: What Happens In Type 1 Diabetes
The Prediabetes Diet Everyone Should Follow
A prediabetes diet can benefit everyone, regardless of your type 2 diabetes risk.
Experts believe the number of people living with diabetes will rise dramatically over the next 30 years.
If current trends continue, according to 2010 projections from the Centers for Disease Control and Prevention , one in three adults may have the disease by 2050.
More than 88 million American adults now have prediabetes, according to the CDC. Prediabetes is a condition marked by above-normal blood sugar levels that aren’t high enough to be diagnosed as type 2 diabetes.
If there’s a silver lining to these alarming statistics, it’s that there’s plenty you can do to prevent type 2 diabetes or slow its progression, and that includes eating a balanced diet. Maintaining a healthy weight is important for everyone, but especially someone who has type 2 diabetes, says Kimberly Rose-Francis, RDN, CDCES, a certified diabetes care and education specialist in Sebring, Florida. Losing weight can help to reduce insulin resistance and may even delay or prevent complications from arising.
RELATED: 10 Diabetes Care Tips During the Coronavirus Pandemic
What Is The Best Weight Loss Plan For Individuals With Diabetes
For purposes of weight loss, the ability to sustain and maintain an eating plan that results in an energy deficit, irrespective of macronutrient composition or eating pattern, is critical for success . Studies investigating specific weight loss eating plans using a broad range of macronutrient composition in people with diabetes have shown mixed results regarding effects on weight, A1C, serum lipids, and blood pressure . As a result, the evidence does not identify one eating plan that is clearly superior to others and that can be generally recommended for weight loss for people with diabetes . Thus, an individualized plan for diabetes nutrition therapy is warranted, taking into account dietary preferences together with the individuals health literacy, resources, food availability, meal preparation skills, and physical activity to maximize the ability to attain and maintain the eating plan . Individualized eating plans should support calorie reduction in the context of a lifestyle program, with appropriate modifications in the medication plan to minimize associated adverse effects such as weight gain, hypoglycemia, and hypotension.
Weight loss interventions can be implemented in usual care settings and alternately in telehealth programs . In general, the intervention intensity and degree of individual participation in the program are important factors for successful weight loss .
Recommended Reading: Drugs That Interact With Metformin
How Does Disordered Eating Factor Into Weight Management
When counseling individuals with diabetes and prediabetes about weight management, special attention also must be given to prevent, diagnose, and treat disordered eating. Disordered eating can make following an eating plan challenging . The prevalence of disordered eating varies, affecting 18% to 40% of people with diabetes . Health care professionals should consider screening for disordered eating, refer to a mental health professional, and individualize nutrition therapy accordingly .
Nutrition Transition And Population Specific Factors
Several countries in sub-Saharan Africa, South America, and Asia have undergone rapid nutrition transition in the past two decades. These changes have paralleled economic growth, foreign investment in the fast food industry, urbanisation, direct-to-consumer marketing of foods high in calories, sale of ultraprocessed foods, and as a result, lower consumption of traditional diets. The effect of these factors on nutrition have led to obesity and type 2 diabetes on the one hand, and co-existing undernutrition and micronutrient deficiencies on the other.
In some populations, such as South Asians, rice and wheat flour bread are staple foods, with a related high carbohydrate intake .77 Although time trends show that intake of carbohydrate has decreased among South Asian Indians, the quality of carbohydrates has shifted towards use of refined carbohydrates.71 The use of oils and traditional cooking practices also have specific patterns in different populations. For instance, in India, the import and consumption of palm oil, often incorporated in the popular oil vanaspati , is high.78 Moreover, the traditional Indian cooking practice of frying at high temperatures and re-heating increases trans fatty acids in oils.79 Such oils are low cost, readily available, and have a long shelf life, and thus are more attractive to people from the middle and low socioeconomic strata but their long term effects on type 2 diabetes are unknown.
You May Like: What Is A High Blood Sugar Reading
Golden Rules Of Healthy Eating When You Have Prediabetes
Here are 10 sound diet principles that can keep your average blood sugars from creeping upward, among other health benefits.
- Skip the sugary drinks. No sweet tea. No juice. No soda. No sweetened lemonade. No mocha latte coffee creations. “My number one recommendation to people is: Don’t drink your sugar,” says Barbara Borcik, RD, CDCES, who works at Clinical Associates in Reisterstown, Maryland. Sugary drinks provide nothing more than empty calories, and they won’t help you feel full. “All the sugary drinks out there are a real risk factor for obesity,” Borcik stresses. A study published in December 2017 in Obesity Facts found a link between sugar-sweetened beverage consumption and obesity among children and adults. And a study published in Circulation showed that sugary beverages increased the risk of type 2 diabetes.
- Pull back on portions. You still can eat many of the foods you like just have smaller amounts of them, Borcik says. Cut out high-calorie, junky snacks, and save your decadent desserts for special occasions. And when youre dining at a restaurant, consider splitting a dish or taking half of it home to eat as leftovers the next day, recommends the American Diabetes Association. Remember that even healthy foods can lead to weight gain if you eat too much of them, and being overweight is a primary risk factor for type 2 diabetes, according to the Mayo Clinic.
RELATED: 8 Steps for Weight Loss Success if You Have Type 2 Diabetes
What Is The Role Of Fat In The Prevention Of Type 2 Diabetes
Large epidemiologic studies have found that consumption of polyunsaturated fat or biomarkers of polyunsaturated fatty acids are associated with lower risk of type 2 diabetes . Supplementation with omega-3 fatty acids in prediabetes has demonstrated some efficacy in surrogate outcomes beyond serum triglyceride levels. In a single-blinded RCT design in Asia, 107 subjects with newly diagnosed impaired glucose metabolism and coronary heart disease supplemented with 1,800 mg/day of eicosapentaenoic acid experienced improved postprandial triglycerides, glycemia, insulin secretion ability, and endothelial function over a 6-month period . Further, in a recent multisite RCT that included 57% of participants with diabetes, age 50 years or older, and with at least one additional CVD risk factor, plus elevated fasting triglycerides and low HDL-C, benefits were seen from adding 2 g of icosapent ethyl twice daily to statin therapy in terms of lower rates of a composite CVD outcome and CVD mortality, but there were also slightly higher rates of hospitalization for atrial fibrillation and serious bleeding .
For more information on fat intake and CVD risk, see the section role of nutrition therapy in the prevention and management of diabetes complications .
Don’t Miss: What Happens If You Stop Taking Diabetes Medication
Dietary Approaches To Diabetes
Food can be powerful in preventing and reversing diabetes. However, dietary approaches have changed as we have learned more about the disease. The traditional approach to diabetes focuses on limiting refined sugars and foods that release sugars during digestion-starches, breads, fruits, etc. With carbohydrates reduced, the diet may contain an unhealthful amount of fat and protein. Therefore, diabetes experts have taken care to limit fats- especially saturated fats that can raise cholesterol levels, and to limit protein for people with impaired kidney function. The new approach focuses more attention on fat. Fat is a problem for people with diabetes. The more fat there is in the diet, the harder time insulin has in getting glucose into the cells. Conversely, minimizing fat intake and reducing body fat help insulin do its job much better. Newer treatment programs drastically reduce meats, high-fat dairy products, and oils. At the same time, they increase grains, legumes, fruits, and vegetables. The study found that patients on oral medications and patients on insulin were able to get off of their medications after some days on a near-vegetarian diet and exercise program. During 2 and 3-year follow-ups, most people with diabetes treated with this regimen have retained their gains. The dietary changes are simple, but profound, and they work.
How Does Alcohol Consumption Impact Risk Of Developing Type 2 Diabetes
Comprehensive reviews and meta-analyses suggest a protective effect of moderate alcohol intake on the risk of developing type 2 diabetes, with a higher rate of diabetes in alcohol abstainers and heavy consumers . Moderate alcohol intake ranging from 648 g/day was associated with a 3056% lower incidence of type 2 diabetes . Knott et al. reported reduced risk of type 2 diabetes at all levels of alcohol intake < 63 g per day with peak reduction at a daily alcohol intake of 1014 g per day in women and non-Asian populations.
A meta-analysis and systematic review that examined the effects of specific types of alcohol beverage consumption and the incidence of type 2 diabetes found that wine consumption was associated with significantly lower diabetes risk, as compared with a smaller reduction in risk with beer and spirits. A U-shaped relationship between alcohol dose and diabetes risk was found among all three types of alcohol, with lowest diabetes risk at 2030 g of alcohol per day from wine and beer and 715 g of alcohol per day from spirits the decrease in diabetes incidence was 20% for wine, 9% for beer, and 5% for spirits.
Recommended Reading: How Long Do Type 1 Diabetics Live
Role Of Physical Activity Or Exercise
Regular physical activity helps the body cells take up glucose and thus lower blood glucose levels. Regular physical activity also helps with weight loss as well as controlling blood cholesterol and blood pressure. You need to let your doctor and dietitian know about the kinds of physical activities you do regularly. Your doctor and dietitian will help you balance your physical activity with your medication and diabetic meal plan. If you are not physically active now, your doctor may recommend that you increase physical activity. Important benefits of a regular aerobic exercise program in diabetes management include decreased need for insulin, decreased risk of obesity, and decreased risk for heart disease. Exercise decreases total cholesterol, improves the ratio of low-density lipoprotein to high-density lipoprotein cholesterol , and reduces blood triglycerides. It may also decrease blood pressure and lower stress levels. Walking is one of the easiest and healthiest ways to exercise. This is one activity that anyone can do for a lifetime without special equipment and with little risk of injury. Talk to your doctor about exercise. Supervised activity is best because of the risk of an insulin imbalance. Use the buddy system when you exercise.
List of foods/drinks to be avoided and their alternatives
Can Type 2 Diabetes Be Prevented
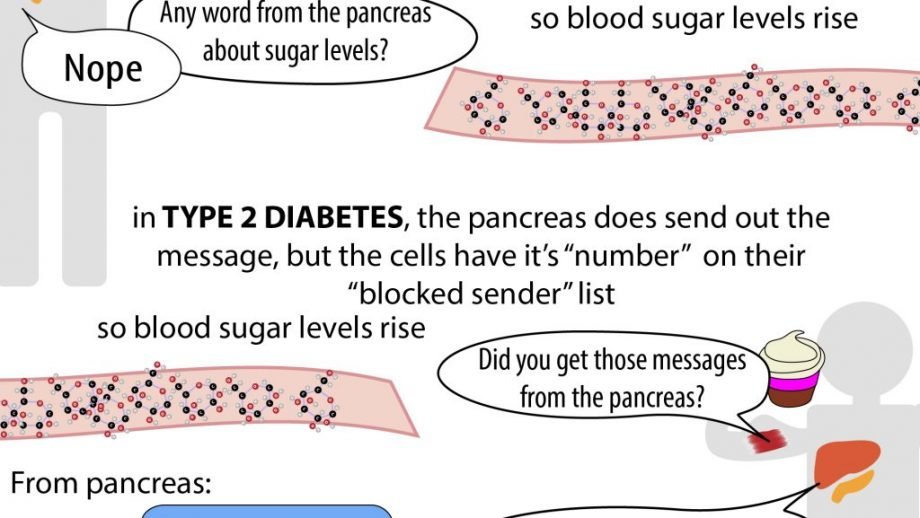
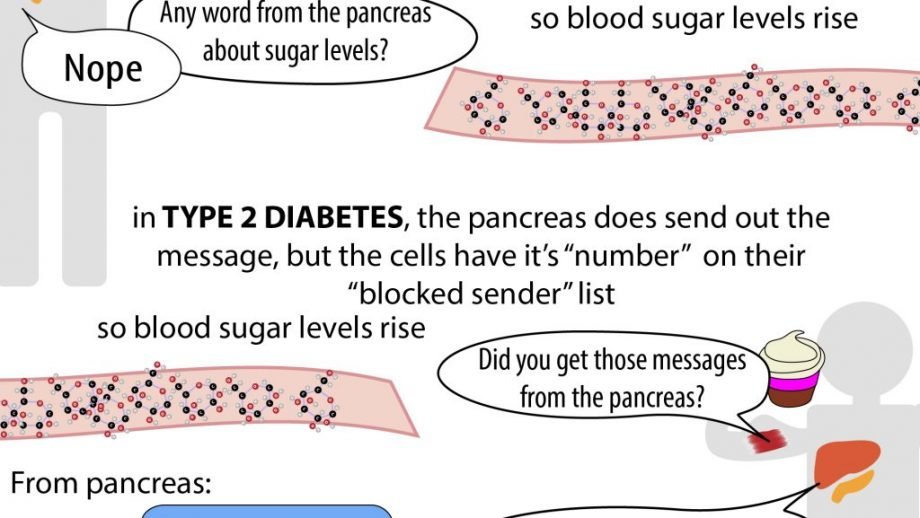
Type 2 diabetes is different. Sometimes, it can be prevented. In type 2 diabetes, the pancreas can still make insulin, but the body doesn’t respond to it in the right way.
Most people who have type 2 diabetes are overweight. In the past, mainly overweight adults got type 2 diabetes. Today, more kids have type 2 diabetes, probably because more kids are overweight.
How can you help prevent type 2 diabetes? Getting to a healthy weight is one way. That’s because a lot of extra weight makes it harder for the body to use insulin properly. Making healthy food choices and getting enough exercise are other good steps to take to help prevent diabetes.
You May Like: Which Pancreatic Cells Release Insulin And Glucagon
What Is The Role Of Weight Loss Therapy In People With Prediabetes Or Diabetes With Overweight Or Obesity
There is substantial evidence indicating that weight loss is highly effective in preventing progression from prediabetes to type 2 diabetes and in managing cardiometabolic health in type 2 diabetes. Overweight and obesity are also increasingly prevalent in people with type 1 diabetes and present clinical challenges regarding diabetes treatment and CVD risk factors . Therefore, MNT and DSMES that include an overall healthy eating plan in a format that results in an energy deficit, as well as a collaborative effort to achieve weight loss in people with type 1 diabetes, type 2 diabetes, or prediabetes and overweight/obesity, are recommended.
Eating plans that create an energy deficit and are customized to fit the persons preferences and resources can help with long-term sustainment and are the cornerstone of weight loss therapy. Regular physical activity, which can contribute to both weight loss and prevention of weight regain, and behavioral strategies are also important components of lifestyle therapy for weight management . Structured weight loss programs with regular visits and use of meal replacements have been shown to enhance weight loss in people with diabetes .
Regular physical activity by itself or as part of a comprehensive lifestyle plan can prevent progression to type 2 diabetes in high-risk individuals. Studies have demonstrated beneficial effects of both aerobic and resistance exercise and additive benefits when both forms of exercise are combined .

