What Happens After My Baby Is Born
If you have been having insulin injections to help manage gestational diabetes these are usually stopped once your baby is born. This is because womens blood glucose levels usually return to the optimal range quite quickly after their babys birth.
Your blood glucose levels will be measured for a few days after your baby is born to make sure that they are within the recommended range. Glucose checking times are usually before breakfast and two hours after meals. An oral glucose tolerance test is done six to twelve weeks after the baby is born to check that your diabetes has gone away.Following the birth of your baby, it is important that your babys blood glucose levels are measured to check that their blood glucose is not too low. If it is, this can be treated by feeding your baby breast milk or formula. Breastfeeding is encouraged as this is best for you and your baby.
A baby whose mother had gestational diabetes will not be born with diabetes, but they may be at risk of developing type 2 diabetes later in life.
Reducing The Risk Of Gestational Diabetes
Recent research has shown that diet and exercise in those that have a high BMI before pregnancy, could reduce the risks of developing gestational diabetes and a further article published in BJOG stated:
Analysis of 13 trials, involving more than 2,800 women, found that exercise reduced the risk of gestational diabetes by more than 30% for women who exercised throughout pregnancy this was even greater . This effect was strongest for women who combined toning, strength, flexibility and aerobic exercise.
Diabetic Eye Screening In Pregnancy
You will be offered regular diabetic eye screening during your pregnancy. This is to check for signs of diabetic eye disease .
Checking your eyes during pregnancy is important. The risk of diabetic retinopathy increases in pregnancy.
Diabetic retinopathy is treatable, especially if it is caught early.
If you decide not to have the test, you should tell the doctor looking after your diabetes care.
- ophthalmologists
- other health care professionals
The obstetricians and midwives will have training in diabetes in pregnancy. They will work with you to provide your antenatal care. They will organise visits and ultrasounds to check on your babys development and growth.
Recommended Reading: Can Type 2 Diabetics Eat Bananas
Urgent Advice: Contact Your Diabetes Team Straight Away If:
- you find out you’re pregnant
You’ll need to make an urgent appointment.
Keeping your blood glucose levels stable can be more difficult in early pregnancy as your hormones change, especially if you have morning sickness. Low blood sugars can happen more easily. It is important to check your blood glucose often. Carry hypo treatment with you in case your blood glucose goes too low.
You’ll have extra appointments with your maternity and diabetes teams when you’re pregnant. This usually means check-ups every 2 weeks, as well as extra tests and scans.
You can have a normal birth, but it’s recommended you have your baby in hospital. You might be advised to have your labour started early .
Risk Factors For Diagnosing Gestational Diabetes
Obesity is mentioned in the media a lot with regards to gestational diabetes and there is a stigma attached to GD diagnosis that only obese or unhealthy women get diagnosed. Sadly this means that many women feel it is not necessary to be tested because they are not overweight, or those that are diagnosed feel embarrassed or ashamed that they have caused this complication.
We see so many ladies joining our Facebook support group who are not overweight so I wanted to conduct some research from our members around risk factors linked to diagnosing gestational diabetes.
On a google survey that was advertised in our Facebook groups and our Facebook page , I received 1,878 responses and here are the results:
When asked to select which of the following risk factors our ladies had, this is what we have found :
- BMI of 30 or more 48%
- Family history of diabetes 44.8%
- Aged 35 or over 35.6%
- Had gestational diabetes in a previous pregnancy 24.3%
- Has PCOS 15.5%
- Previously given birth to a baby who weighed 10lb or more 6.8%
- Family origins are South Asian, black Caribbean or Middle Eastern 4.2%
- Pregnant with a multiple birth 1.5%
- NO RISK FACTORS LISTED ABOVE 9.8%
Don’t Miss: Which Pancreatic Cells Release Insulin And Glucagon
The Glucose Drink Used For Diagnosis In The Uk And Roi
Last year Lucozade changed the amount of glucose in their drink to help lower the amount of sugar consumers are drinking, therefore to deliver a 75g glucose load would require in excess of 800mL of Lucozade! For this reason, the majority of hospitals will now be using a glucose replacement drink to conduct the OGTT.
You may see pictures of a glucose drink which is used in the USA for gestational diabetes testing and pictures of babies in the womb with slogans like Mom, dont drink the glucola or dont drink this toxic drink. The problem with Glucola is BVO, or brominated vegetable oil and it is found in many US drinks. Brominated vegetable oil is banned as a food additive in Europe under Regulation No 1333/2008.
Please note, this is NOT the same as the products used in the UK! In the UK and Ireland there are a few different glucose load options used:
Polycal:
- Ingredients Demineralised water, glucose syrup, maltodextrin, acidity regulator .
- Ingredients Demineralised water, glucose syrup, maltodextrin, acidity regulator , flavour , colour
Rapilose: Ingredients Water, glucose syrup, glucose monohydrate, flavouring, citric acid , potassium sorbate, sodium benzoate
Glucose monohydrate/ Glucose BP/ Dextrose monohydrate
If you have any concerns over the product used for diagnosing gestational diabetes, then you could ask to see the listed ingredients before taking the test.
What If I Have Gestational Diabetes
GD is increasingly common, with about 7% of women having the condition. If you are found to have GD, you will work closely with your health care provider to keep your blood glucose levels in a healthy range. This involves choosing a healthy diet, gaining the recommended weight during your pregnancy, getting exercise, and if needed, taking insulin or pills to lower your blood sugar. Your babys wellbeing will be carefully monitored by regular measurements of growth and amniotic fluid volume. If you have GD you will be offered a repeat glucose tolerance test between 6 weeks and 6 months postpartum to detect prediabetes and diabetes. You may also be offered induction between 38-40 weeks of pregnancy. Finally, it is strongly recommended that women with GD breastfeed their infants.
Read Also: Which Pancreatic Cells Release Insulin And Glucagon
Should I Avoid Or Decline Being Tested
Ultimately it is up to each mother to make an informed choice as to what is best to do for her baby and pregnancy. You cannot be forced into taking any tests in pregnancy, but we highly advise looking at the complications gestational diabetes can have on your baby and you, many of which are symptomless.
A pregnancy diagnosed with gestational diabetes may mean more intervention, as you will be advised to test blood sugar levels regularly and will be referred for additional appointments at hospital, alongside additional ultrasound scans. Then depending on how well blood sugar levels can be managed, it may mean medication or insulin injections. Having gestational diabetes may also mean that you could be advised to have your baby earlier than planned and in a hospital setting, under consultant led care.
There are no certainties with gestational diabetes and some, or all of these interventions could be recommended, but it is up to each mother to decide which interventions to accept or decline. Use the B R A I N approach to help with making your decisions.
Monitoring blood sugar levels to record findings from fasting and after all meals would be a beneficial step, should you choose to refuse a GTT and is ultimately the most important thing in helping to manage the condition.
Refusing BOTH the GTT and monitoring blood sugar levels at home, could lead to many complications for your baby should you have undiagnosed and uncontrolled blood sugar levels.
Diagnosing Gestational Diabetes In The Uk & Roi
For women with any of the above risk factors, a 2 hour 75 g oral glucose tolerance test is used to for diagnosing gestational diabetes between 24 28 weeks.
If glycosuria of 2+ or above on 1 occasion, or of 1+ or above on 2 or more occasions is detected by urine dip test during routine antenatal appointments, this may indicate undiagnosed gestational diabetes and so women with this should be referred for an OGTT.
In some areas all pregnant women are screened for gestational diabetes.
Those that have previously been diagnosed with gestational diabetes are often tested at 16 weeks in subsequent pregnancies and again at 24 28 weeks should the first test come back as negative. Some hospitals will not test for gestational diabetes in subsequent pregnancies and may offer blood glucose monitoring from an early gestation instead.
Also Check: Which Pancreatic Cells Release Insulin And Glucagon
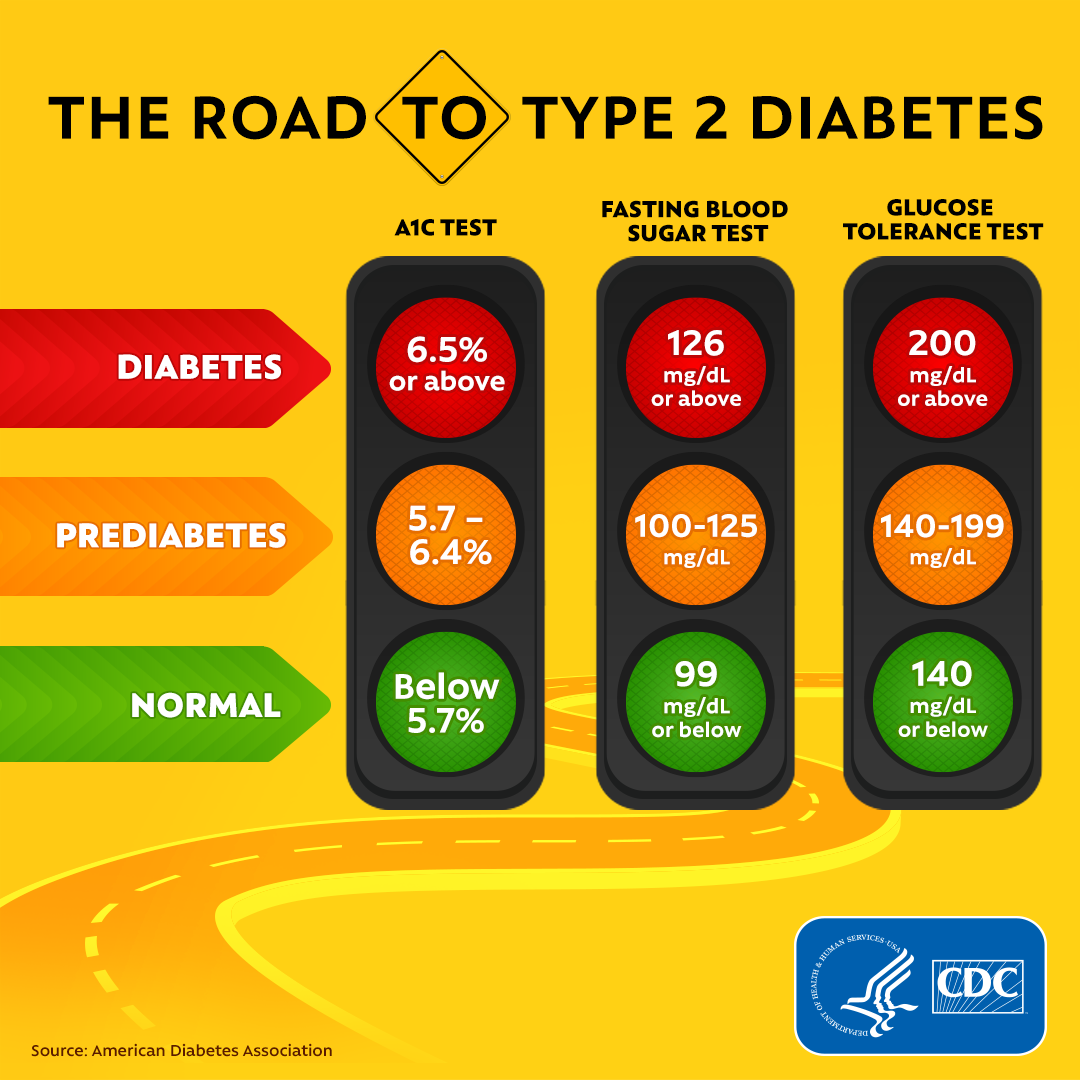
The Glucose Tolerance Test
This test is used to determine your body’s response to sugar . A glucose tolerance test is used to screen for type 2 diabetes and very often it is used to diagnose gestational diabetes. Generally speaking, your doctor will likely have a screening test during your second trimester – between 24 and 28 weeks of pregnancy.
-
Be sure to ask your health care providers who will arrange your test and who will share the results with you.
- Fast for eight hours before the test. After the lab takes a blood sample, you will be given a sugary drink. Two hours later, you will have another blood test.
NOTE: If your results are abnormal, arrange to discuss this further with your health care provider. If your results are normal you will need to be tested before planning another pregnancy or every 3 years or more often depending on risk factors.
Screening For Gestational Diabetes
During your first antenatal appointment at around week 8 to 12 of your pregnancy, your midwife or doctor will ask you some questions to determine whether you’re at an increased risk of gestational diabetes.
If you have 1 or more risk factors for gestational diabetes you should be offered a screening test.
The screening test is called an oral glucose tolerance test , which takes about 2 hours.
It involves having a blood test in the morning, when you have not had any food or drink for 8 to 10 hours . You’re then given a glucose drink.
After resting for 2 hours, another blood sample is taken to see how your body is dealing with the glucose.
The OGTT is done when you’re between 24 and 28 weeks pregnant. If you’ve had gestational diabetes before, you’ll be offered an OGTT earlier in your pregnancy, soon after your booking appointment, then another OGTT at 24 to 28 weeks if the first test is normal.
Find out more about an OGTT.
Also Check: Insulin Glargine Warnings
Can Gestational Diabetes Cause Problems During Pregnancy
Yes. If not treated, GDM can cause pregnancy complications, including:
Gestational diabetes also can cause health complications for your baby after birth, including:
- Breathing problems, including respiratory distress syndrome . This is a breathing problem caused when babies dont have enough surfactant in their lungs. Surfactant is a protein that keeps the small air sacs in the lungs from collapsing.
- Jaundice. This is a medical condition in which a babys eyes and skin look yellow. A baby has jaundice when his liver isn’t fully developed or isnt working well.
- Low blood sugar
- Obesity later in life
Are Some Women At A Higher Risk Of Getting Gestational Diabetes Than Others
You have an increased risk of gestational diabetes if:
- your body mass index is 30 or more
- you have previously had a baby who weighed 4.5kg or more at birth
- you had gestational diabetes in a previous pregnancy
- you have PCOS
- you have a family history of diabetes one of your parents or siblings has diabetes
- your family origins are South Asian, black Caribbean or Middle Eastern
- you are aged 35 or older
You May Like: What Is A High Blood Sugar Reading
Oral Glucose Challenge Test
If you are not at high risk of diabetes in pregnancy, your midwife will offer you an oral glucose challenge test when you are between 24 and 28 weeks pregnant. This test measures how well your body can process sugar. You can have this test at any time of the day.
For this test, youll drink a sugary drink and then wait 1 hour before giving a blood sample. You will not need to do anything special before or after the test. Most people do not have side effects from the oral glucose challenge test.
Do Not Skip Breakfast:
It is always said that opting for a healthy breakfast is the way to go. Never skip your breakfast, especially when you are pregnant.
If you happen to do so, it will make you hungrier. You will indeed have a more significant chunk of the meal. The next time you eat. This, in turn, leads to the onset of diabetes or even gestational diabetes.
Read Also: How Many Points Does Metformin Lower Blood Sugar
Is There Another Way To Test Without Taking The Gtt
If you feel strongly that you do not want a GTT for diagnosing gestational diabetes, then you should discuss your reasons with your health care professionals.
Many hospitals will happily agree to home blood glucose monitoring which involves testing blood sugar levels at home with a blood glucose monitor and test strips.
Prevent Type 2 Diabetes
If your test results show you have prediabetes, ask your doctor or nurse if there is a lifestyle change program offered through the CDC-led National Diabetes Prevention Program in your community. You can also search for an online or in-person program. Having prediabetes puts you at greater risk for developing type 2 diabetes, but participating in the program can lower your risk by as much as 58% .
Read Also: Craving Milk Type 2 Diabetes
Symptoms Of Gestational Diabetes
Gestational diabetes does not usually cause any symptoms.
Most cases are only discovered when your blood sugar levels are tested during screening for gestational diabetes.
Some women may develop symptoms if their blood sugar levels gets too high , such as:
- needing to pee more often than usual
- a dry mouth
- tiredness
But some of these symptoms are common during pregnancy and are not necessarily a sign of gestational diabetes. Speak to your midwife or doctor if you’re worried about any symptoms you’re experiencing.
How Is Gestational Diabetes Managed After Pregnancy
Research has shown that women with gestational diabetes have a 3 to 7 percent chance of developing type 2 diabetes within five to 10 years which is why its so important to make those healthy habits routine during pregnancy and keep a check on your health even after your pregnancy is over.
Here are a few ways to stay healthy after baby is born:
You May Like: How Many Points Does Metformin Lower Blood Sugar
What If I Test Positive
Remember: its not the end of the world. Its scary, but as youll learn, you and your baby will be fine.
If your test is positive, your doctor will most likely prescribe more doctor appointments, and monitor your blood sugar closely. Youll be asked to take your blood sugar several times a day. I took mine every few hours, which meant I pricked my finger to get a reading 5 6 times per day.
Many times, you can control your blood sugar through a healthy, no sugar-diet. Other times, insulin may be required.
Because I closely monitored my sugar levels, ate a no-sugar diet, and made sure I exercised every day, I was able to stay off insulin.
Screening Diagnosis And Management Of Gestational Diabetes Mellitus

ANDREW GARRISON, MD, Central City Community Health Center and the University of Utah, Salt Lake City, Utah
Am Fam Physician. 2015 Apr 1 91:460-467.
Gestational diabetes mellitus affects approximately 6% of pregnancies in the United States, and it is increasing in prevalence. Pregnant women without known diabetes mellitus should be screened for GDM after 24 weeks of gestation. Treatment of GDM results in a statistically significant decrease in the incidence of preeclampsia, shoulder dystocia, and macrosomia. Initial management includes glucose monitoring and lifestyle modifications. If glucose levels remain above target values, pharmacologic therapy with metformin, glyburide, or insulin should begin. Antenatal testing is customary for women requiring medications. Induction of labor should not occur before 39 weeks in women with GDM, unless glycemic control is poor or another indication for delivery is present. Unless otherwise indicated, scheduled cesarean delivery should be considered only in women with an estimated fetal weight greater than 4,500 g. Women with a history of GDM are at high risk of subsequently developing diabetes. These patients should be screened six to 12 weeks postpartum for persistently abnormal glucose metabolism, and should undergo screening for diabetes every three years thereafter.
Also Check: How To Keep Blood Sugar From Dropping
During Labour And Delivery
Most women who have gestational diabetes are able to have their babies vaginally. Just because you have gestational diabetes does not mean that you will need to have a caesarean section .
Because a baby that has grown too large can be difficult to deliver safely, your doctor will do fetal ultrasounds to check the size of your baby. If your doctor thinks that your baby is in danger of being too large, he or she may decide to induce labour or do a C-section.
During labour and delivery, you and your baby are monitored closely. This includes:
- Checking your blood sugar level regularly. If your level gets too high, you may be given small amounts of insulin through a vein . If your level drops too low, you may be given IV fluid that contains glucose.
- Checking your baby’s heart rate and how well your baby’s heart responds to movement. Fetal heart monitoring helps your doctor know how your baby is doing during labour. If the baby is large or does not seem to be doing well, you may need to have a C-section to deliver your baby.

