Selecting An Insulin Infusion Protocol
Numerous insulin infusion protocols have been published. However, head-to-head comparisons are rare, and efficacy and safety are difficult to determine because of differing patient populations, glycemic targets, metrics for evaluation, and definitions of hypoglycemia used in the various protocols., Selecting a validated protocol allows for more rapid implementation but does not eliminate the need for ongoing safety and effectiveness monitoring and continuous quality improvement.
Some paper protocols are table-based, whereas others require mathematical calculations. The level of clinical judgment and physician oversight also varies among the available protocols. Computerized protocols allow for more complex mathematical calculations and can provide alerts or alarms to remind staff members to check patients blood glucose level and adjust infusion rates.
Several studies comparing computerized and paper-based protocols have found improved protocol adherence, improved glycemic control, and less hypoglycemia with computerized protocols. It is worth noting that evaluations of computerized glucose control programs have used glycemic targets that are tighter than currently recommended, and although the percentages of blood glucose readings within the target range were higher than with paper protocols, they still were not optimal in most studies. It is not clear how computerized glucose control programs compare to paper-based protocols when currently recommended targets are used.
How Is Insulin Given
Insulin cannot be taken by mouth, as it is destroyed by the digestive juices in your digestive system. It is therefore given by an injection under the skin. Insulin may come:
- In a vial to be injected with a separate syringe.
- In a cartridge to be used with an injection pen.
- In a pre-filled injection device.
- In the form of a pump, which tries to mimic the natural delivery of insulin.
Your doctor or diabetes nurse will show you how to inject yourself with insulin. It is usually injected under the skin into your upper arms, thigh, buttocks or tummy . Most people take 2-4 injections of insulin each day.
The type and amount of insulin you need may also vary each day, depending on what you eat and the amount of exercise you do. Your doctor or nurse will tell you when to inject your doses, as different types of insulins are given at different times in relation to food. It is important that you inject your doses when you have been advised to and not miss out any of your doses of insulin.
It is important to remember that insulin doses are referred to in terms of units. Make sure you know how much to use – ask your doctor or nurse if you are unsure. Before you start treatment your doctor or diabetes nurse will give a lot of advice and instruction on how and when to take the insulin.
Continuous Insulin Infusion: When Where And How
The association between inpatient hyperglycemia and adverse patient outcomes is well documented. Thus, focus on inpatient glycemic control has increased in the past decade. However, optimal glycemic targets remain controversial, and significant barriers to optimal glycemic control persist.
Don’t Miss: Can You Lose Weight With Diabetes
Drug Forms And Strengths
Humulin R comes as a liquid solution. Its available in two strengths:
- Humulin R U-100. This strength contains 100 units of insulin per 1 mL of solution. It comes in 3-mL and 10-mL vials.* In the 3-mL vial, youll have a total of 300 units of insulin human. And in the 10-mL vial, youll have a total of 1,000 units of insulin human.
- Humulin R U-500. This strength contains 500 units of insulin per 1 mL of solution. It comes in a 20-mL vial.* Its also available as a 3-mL KwikPen,** which is a prefilled pen thats meant to be used only by one person. In the 20-mL vial, youll have a total of 10,000 units of insulin human. And in the 3-mL KwikPen, youll have a total of 1,500 units of insulin human.
* If youre using vials of Humulin R, youll need to purchase appropriate syringes and needles to administer the drug.
** If youre using the Humulin R KwikPen, youll need to purchase appropriate needles to use with the pen.
Both the vials of Humulin R and the KwikPens are meant to be used more than once. However, the actual number of times youll use a certain vial or pen will depend on your insulin dosage.
But keep in mind that youll need to use a new syringe and a new needle for each dose of Humulin R from a vial. And youll need to use a new needle for each dose of insulin from a KwikPen. Using needles or syringes more than once can increase your risk of infection.
Choosing And Using Insulins
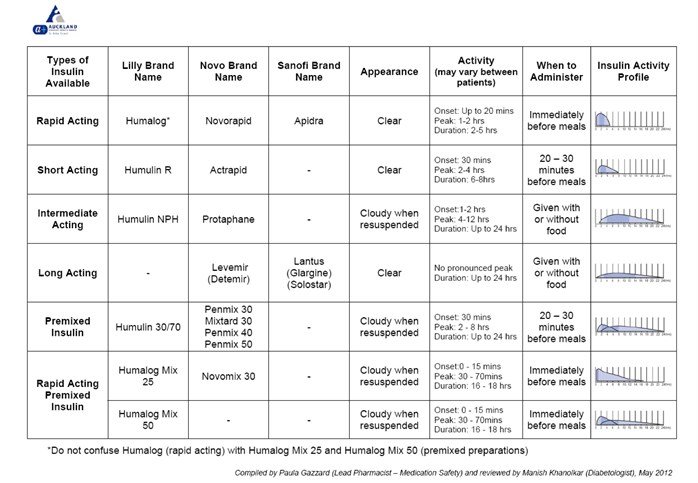
As there are different insulins available in different parts of the world, decisions about which insulin to choose are sometimes not based upon what is ideal but more practically what is possible. Older insulins cost less than newer analogues but tend to have more variable peak and valley effects as well as producing more hypoglycaemia and hyperglycaemia as a result. Such older animal-source or human regular and NPH insulins are associated with less flexibility and greater rigidity of food and activity timing than with newer but more costly analogues. In previous decades without much monitoring possibility, more rigid food and activity schedules attempted to compensate for such lack of flexibility but glycaemic control was also less optimal so there were more short and long-term complications.
Most diabetes specialists and most guidelines acknowledge that the improved control possible with modern diabetes regimens is partly attributed to the improved insulin profile available with newer but costlier analogue insulins, using MDI regimens or pumps. It should be remembered that insulin pump therapy is not the only way to have excellent glucose control. Targeted blood glucose control as proven by the landmark DCCT studies remain the essential element of T1DM care if resources can be provided for such monitoring and insulin delivery coupled with educational, nutritional and psychosocial support for the child and adolescent.
1Fast-Acting Insulins
2Rapid-Acting Insulins
Don’t Miss: How Does Squeezing Finger Affect Blood Sugar
Barriers To Implementing A Continuous Insulin Infusion Protocol
Potential barriers to implementing an insulin infusion protocol include fear of hypoglycemia, confusion regarding appropriate glycemic targets, insufficient nurse-to-patient ratios, insufficient availability or convenience of glucose-monitoring devices, lack of administrative support, various system and procedural issues, and resistance to change. Before implementing an IV insulin infusion protocol, it is imperative to evaluate the current glycemic-related practices within the institution and address the following crucial questions: What is the current level of glycemic control? Who is checking patients blood glucose and how often? How interested is the staff in optimizing glycemic control, and do they have the support they need to achieve this goal?
Key steps to overcoming these barriers include building support with multidisciplinary champions, involving key staff members in the process, educating staff and administrators about the benefits of optimizing glycemic control, and internally marketing the clinical success of the protocol. Descriptions of several models of implementation have been published, including endocrinologist consultation models, glycemic control teams, and system-wide models. It is important to adapt whichever model is selected to meet the needs of the specific institution.
How To Take Humulin R
Humulin R is given by subcutaneous injection . When Humulin R is prescribed for you, your doctor or pharmacist will show you how to give yourself the drug injections. You should take Humulin R according to your doctors or healthcare providers instructions.
The manufacturer of Humulin R offers step-by-step instructions on how to give yourself an injection of Humulin R using a vial of the drug, insulin syringes, and needles. The instructions for Humulin R U-100 can be found on this web page. And instructions for Humulin R U-500 can be found on this web page. You can also watch a video that shows how to inject your dose of Humulin R U-500 using a needle and syringe on this website.
If youre using the Humulin KwikPen, the drug manufacturers website offers specific instructions, including a video, on how to inject your dose. You can also view written directions on how to use the KwikPen on this web page.
Its important to remember that you should never use syringes or needles more than once while taking Humulin R.
After using these supplies for each dose, you should dispose of them right away into a sharps container. For more information about this, see the section Humulin R expiration, storage, and disposal above.
In addition, you should never share syringes or needles with other people or use these supplies more than once. Doing so can increase your risk of getting or spreading infection.
Also Check: How Much Vitamin B12 Should A Diabetic Take
Transition From Iv To Subcutaneous Insulin
To avoid loss of glycemic control and optimize patient outcomes, it is important that patients are appropriately transitioned from IV to subcutaneous insulin. This is especially important for patients with type 1 diabetes, because they can develop DKA if scheduled basal insulin and prandial insulin are not initiated before stopping the insulin infusion. A transition protocol provides guidance regarding which patients are likely to require transition to subcutaneous insulin and when and how to make the transition. Patients with type 1 diabetes and most patients with type 2 diabetes who were treated with insulin before hospitalization will require such a transition. In addition, patients receiving > 2 units/hour of insulin on the infusion protocol will likely require subcutaneous insulin unless there is a significant change in their clinical situation, such as discontinuation of parenteral/enteral nutrition, tapering of steroids, or gastric bypass surgery.
The appropriate timing for the transition from IV to subcutaneous insulin depends on institutional policies regarding where and when insulin infusion can be used. Ideally, the transition occurs when patients begin an oral diet and their blood glucose levels are stable within the target range. IV insulin has a very short duration of action , and the onset of basal subcutaneous insulin is 1-2 hours. Thus, IV insulin should be continued for 1-2 hours after the first administration of subcutaneous basal insulin.
Hypoglycemia Prevention And Treatment
Recent data have brought renewed appreciation of the risk for hypoglycemia.,, Historically, hypoglycemia has been variably defined as a blood glucose level of anywhere from < 40 to < 70 mg/dl. The ADA currently defines hypoglycemia as a blood glucose level < 70 mg/dl. The most effective strategies to prevent hypoglycemia include frequent blood glucose monitoring and proactive adjustment of the infusion rate if the blood glucose level decreases too rapidly. In addition, more frequent blood glucose monitoring should be implemented until blood glucose is consistently > 100 mg/dl. Some hypoglycemia protocols temporarily stop the insulin infusion for hypoglycemia and restart it at a lower rate once hypoglycemia has resolved. However, failure to restart the infusion can result in profound hyperglycemia and ultimately diabetic ketoacidosis in patients with type 1 diabetes. Thus, some hypoglycemia protocols do not stop the infusion, but significantly reduce the rate.
Read Also: Where To Dispose Of Insulin Needles
Indications For Intravenous Insulin
Because of their susceptibility to deep wound infections, patients who undergo open cardiac surgery may benefit from the routine use of intravenous insulin. Patients with diabetes who have suboptimal glucose control with conventional subcutaneous insulin treatment may also benefit from intravenous therapy.
What Is Intravenous Insulin Used For
Insulin is used to treat diabetes.;
People with type 1 diabetes do not produce insulin and they need insulin injections so the body can use the glucose from meals.;
People with type 2 diabetes make insulin, but their bodies do not respond properly to it. This is called insulin resistance. Some people with type 2 diabetes need insulin shots, though most are treated with pills and diet changes.;
Read Also: How To Determine If You Have Diabetes
How Insulin Is Supplied
- It can be drawn out of an insulin vial ONLY using an insulin syringe. When injecting insulin, it is important to allow at least 10 seconds before the needle is removed. This helps to ensure that the full insulin dose administered is absorbed. Wet skin at the injection site after the needle is removed could be insulin that has not been absorbed.
Figure: using an insulin syringe to draw insulin out of an insulin vial
- It can be provided as a prefilled pen device, which is disposed of once empty.
- It can be provided as a cartridge that can be loaded into an insulin pen.
Insulin should never be drawn out of a cartridge using a syringeFigure: insulin should never be drawn out of a cartridge using a syringe
Should Cii Be Restricted To The Icu

IV insulin infusion protocols have generally been reserved for theintensive-care setting. Studies to support use of CII have primarily beenlimited to ICUs. However, patients who could benefit from insulin infusiontherapy are not restricted to the intensive-care setting. The use of IVinsulin protocols has been widely accepted in the treatment of patientspresenting with hyperglycemic hyperosmolar state and diabetic ketoacidosiswithout a requisite admission to the ICU. Events leading to prolongedhyperglycemia or significant fluctuations in blood glucose levels should notrequire admission to the ICU for appropriate treatment. Conversely, patientsin the ICU who are now clinically stable should not have transfer to astep-down unit or regular medical floor delayed secondary to hospitalrestrictions regarding IV insulin.
In 2005, a group from Duke University published results of a projectevaluating the safety, effectiveness, and feasibility of using an IV insulinalgorithm in the general hospitalwards. Auditfindings indicated that the nomogram for monitoring IV insulin infusion couldbe used effectively on intermediate-care general medicine units with anurse-to-patient ratio as high as 1:6.
Don’t Miss: Is Dragon Fruit Good For Diabetes
Optimal Range Of Glucose Control
The results of the experience with intravenous insulin and tight glucose control led to a re-examination of the optimal range of glucose control. Although control of hyperglycemia did reduce infection rates, especially after cardiothoracic surgery, a net benefit was tempered by higher rates of hypoglycemia and mortality. The ideal target blood glucose level in the intensive care setting has yet to be established but seems to be less than 180 mg/dL .
The lowest acceptable threshold for serum glucose has not been established. However, given the increased risk of hypoglycemia associated with insulin protocols that sought to control blood glucose levels between 80 and 110 mg/dL, a goal of less than 110 mg/dL cannot be endorsed. This was also the sentiment of a consensus statement that suggested a glucose target of 140-180 mg/dL in critically ill patients; however, certain subgroups, such as patients undergoing cardiothoracic surgery, may benefit from a lower target range. Â;Therefore, a glucose target of 110-140 mg/dL may eventually be a more appropriate range for this subgroup and other critically ill patients; however, this level of control has not been subjected to rigorous investigation and determined with evidence-based support.
Alternative Drugs Other Than Insulin For Type 2 Diabetes
There are several drugs other than insulin that are used to help manage blood sugar levels in people with type 2 diabetes. Examples of these drugs include:
- biguanides, such as:
You may wonder how Humulin R compares with other medications that are prescribed for similar uses. Here we look at how Humulin R and Novolin R are alike and different.
Also Check: How Many Points Does Metformin Lower Blood Sugar
Some Side Effects Can Be Serious If You Experience Any Of The Following Symptoms Call Your Doctor Immediately:
- rash and/or itching over the whole body
- shortness of breath
- large weight gain in a short period of time
- swelling of the arms, hands, feet, ankles, or lower legs
If you experience a serious side effect, you or your doctor may send a report to the Food and Drug Administration’s MedWatch Adverse Event Reporting program online or by phone .
Metrics For Evaluating Insulin Infusion Protocols
Ongoing evaluation of efficacy and safety is also crucially important to the successful implementation of an insulin infusion protocol. Such evaluation facilitates continuous improvement and staff education and builds momentum to support expansion of the protocol into additional patient populations or additional settings within the institution. Evaluation metrics can be as simple as tracking 1) mean or median blood glucose with standard deviations or interquartile ranges by unit or patient population and 2) incidence of hypoglycemia. It is also important to evaluate glucose variability because increased variability is also associated with poor patient outcomes. Depending on the institutions specific goals and barriers, metrics can include more advanced evaluation, including financial analysis. Several institutions have published their metrics and financial impact assessments.- Similar to staff education, evaluation metrics will differ from one institution to another but remain a crucial tool for safe and effective insulin infusion programs in all institutions.
Also Check: What Causes Diabetics To Lose Their Legs
Ask The Diabetes Team
Question: From a nurse in Michigan, USA: Can insulin be given IV push ? I am a new nurse and this was a sliding scale order for one of my patients. The patient’s blood sugar level was 234 and the sliding scale order was to give 2 units of R insulin IV push and 8 units R subcutaneously. The patient was 54 years old. My nursing drug book stated not to give concentrated insulin IV. Is this something new that physicians are beginning to prescribe? Answer: Regular insulin can be given as an IV push undiluted. The only reason to dilute it is to facilitate low dose continuous infusion if this is what is needed. DTQ-19991105013815 Original posting 11 Jan 2000 Posted to Insulin This Internet site provides information of a general nature and is designed for educational purposes only. If you have any concerns about your own health or the health of your child, you should always consult with a physician or other health care professional. This site is published by T-1 Today, Inc. , a 501c3 not-for-profit organization, which is responsible for its contents. Our mission is to provide education and support to families living with type 1 diabetes. By using this site, you agree to our Terms of Use, Legal Notice, and Privacy Policy. © Children with Diabetes, Inc. 1995-2017. Comments and Feedback.Continue reading >>

