Signs & Symptoms Of Hypoglycemia
The signs and symptoms of hypoglycemia usually appear quickly and are related to the release of epinephrine as the body tries to compensate for the drop in blood glucose levels. In the beginning stages the patient may complain of severe hunger. The following signs and symptoms are normally associated with the decreased availability of glucose to the brain:
- Nervousness/trembling
- Seizures
- Coma in severe cases
Also hypoglycemia should be suspected in any diabetic patients with acute behavioral changes, abnormal neurological signs or unconsciousness with no apparent reason. Hypoglycemia is a true medical emergency and must be aggressively treated with glucose to prevent permanent brain damage or death.
Diabetic Emergencies When To Get Medical Help
This National Diabetes Month is the right time to learn about the types of diabetic emergencies and warning signs to go to the ER. Prestige ER is proud to join the American Diabetes Association and other organizations in educating our communities on diabetes, its potential complications, and what to do in case of a diabetic emergency.
How To Perform A Ketone Test
1. Assemble the required equipment to perform the urinalysis
3. Check the urine sample is fresh – observe the colour and odour. Cloudy urine may indicate the sample is contaminated or infection is present. A strong fishy smell may indicate infection and a sweet odour like pear drop sweet may indicate ketones are present.
4. Check the sample is from the correct person and note any medications they are taking .
5. Wash hands and apply gloves/apron.
6. Remove a test strip from the bottle and replace the lid.
7. Immerse the full length of the test strip in the urine sample, ensuring all the test pads are covered. Remove excess urine on the lip of the sample bottle.
8. Place the test strip on the tissue/absorbent paper to prevent the colours on the pads contaminating each other.
9. Start the timer/note the time.
10. Replace the lid on the urine specimen.
11. When the appropriate amount of time has passed, align the test pads with the corresponding result gauge on the test strip bottle.
12. Be sure to line the pads up with the corresponding test on the container. This is where most errors with urine testing are made!
13. Remove your glove and record the result of the urine test in the persons medical record. Report any abnormal result to a senior nurse, the diabetes care team or the persons doctor as appropriate to your role and care setting.
14. Dispose of all equipment in the clinical waste bag.
15. Wash your hands.
Recommended Reading: Child Blood Sugar Levels Chart
Wearable Glucose Monitoring Sensors
There are two types of wearable glucose monitoring technologies intermittently scanned flash glucose monitoring and continuous glucose monitoring which are described in this section. They are only funded by the NHS for people with type 1 diabetes who meet NHS England criteria.
Healthcare professionals who will be working with flash and continuous glucose monitoring are directed to these webinars. It is important you are able to help your patients access wearable glucose monitoring devices appropriately, interpret their data and improve their glycaemic outcomes.
Consensus Statement And Methodology
The correct answer is Option 1.
Feedback: Hypoglycaemia is described as a blood glucose < than 4 mmols. Glucose is a sugar carried in the blood stream that your body uses for energy. Blood glucose can be erratic at times, sometimes becoming very low when medication is taken and food is restricted or the patient is off their food.
As Mrs Patel is still conscious and responding to her name, and her swallowing reflex is intact you would aim to treat her hypo following the guidelines for the management of hypoglycaemia in the nursing home. Can you remember what the recommended treatments for hypoglycaemia are?
Feedback: Recommended treatments for hypoglycaemia:
- 10-20g glucose give by mouth
- or five jelly babies,
- or three glucose or dextrose tabs,
- or a small glass of sugary drink
- or a small carton of pure fruit juice
- or two tubes of a glucose gel such as GlucGel®.
If Mrs Patel does not feel better and the blood glucose is still less than than 4 mmols after 10-15 minutes repeat one of the above treatments again. When Mrs Patel starts to feel better it is advisable to give some longer-acting carbohydrate such as 1 slice of bread or 2 biscuits. Providing sustained carbohydrate will minimise further falls in blood glucose.
What was the cause of Mrs Patels hypoglycaemia?
The correct answer is Option 3.
Feedback: All of these ways are correct.
You May Like: Low Blood Pressure And Diabetes
Diabetic Emergency First Aid: What Should You Do If Someone Is Having Diabetic Emergency
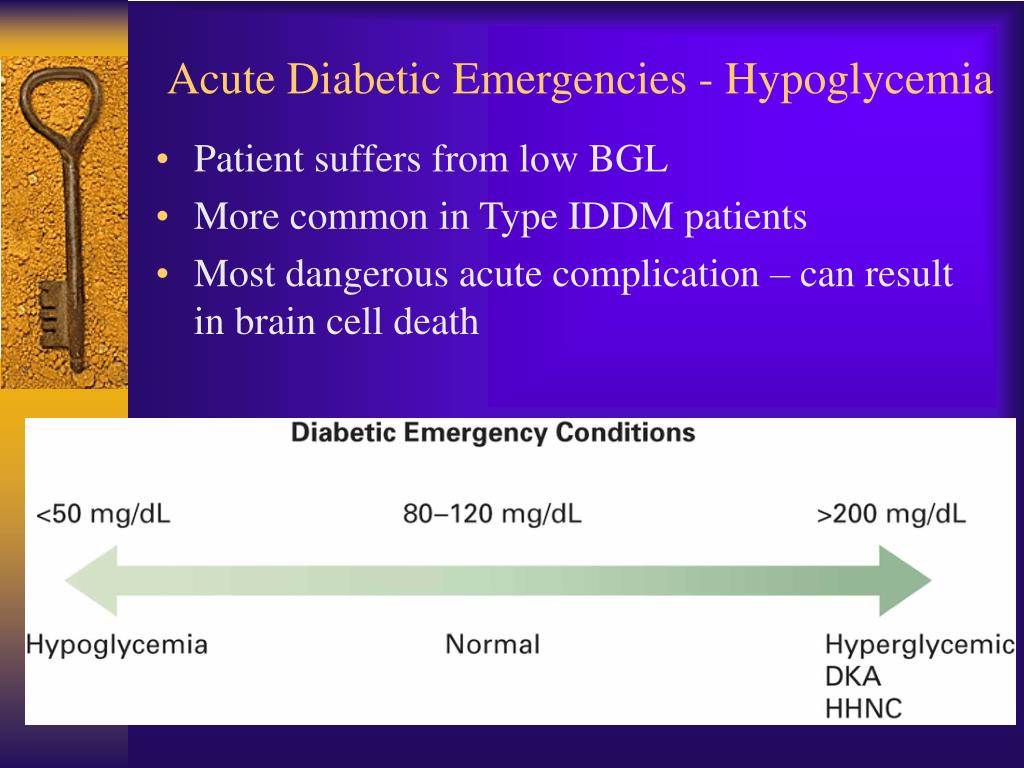
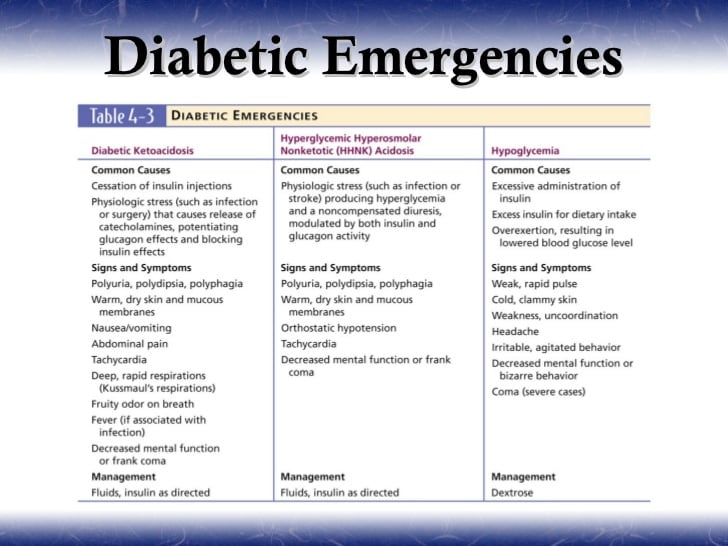
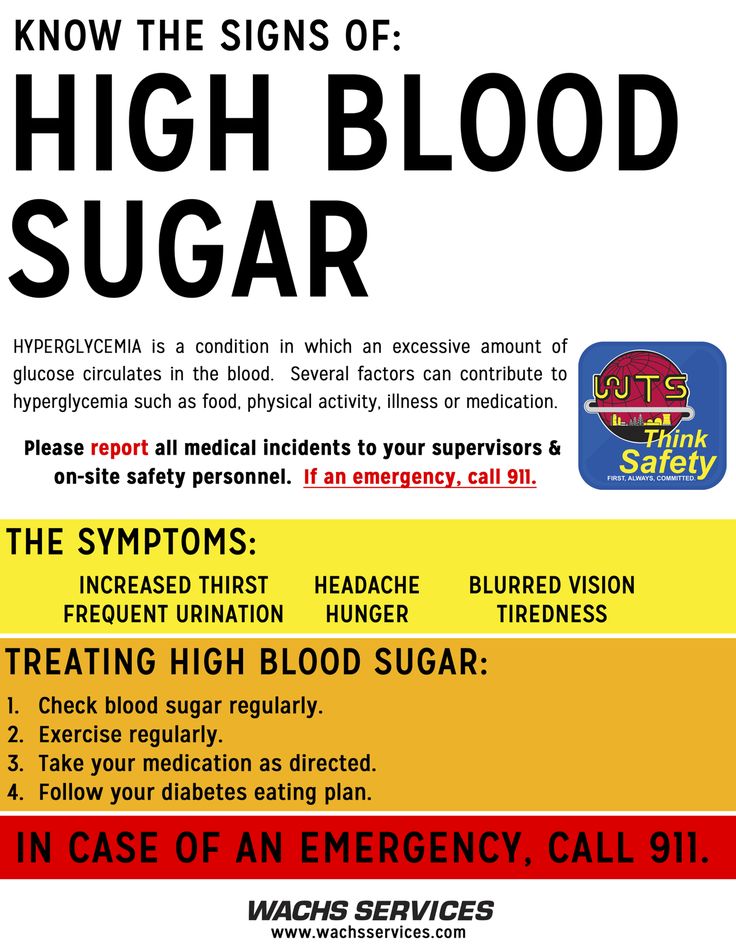
A diabetic can develop hyperglycemia or hypoglycemia , which above or below a particular range can turn into an emergency. Knowing how to handle such a situation is very necessary for the patient or the members around.
The most common diabetic emergencies are:
- Severe hypoglycemia
- Hyperglycaemic hyperosmolar syndrome
What Causes Diabetic Ketoacidosis
Heres an example of how high blood sugars can lead to DKA:
You May Like: Elevated Sugar Symptoms
When Is It Necessary To Call A Doctor If You Have Diabetes
- If you have diabetes and your blood sugar is 300 mg/dL or higher two times in a row for an unknown reason.
- If you have a low blood sugar that has not come up after three treatments, call your healthcare provider or 911.
- If you see a person with diabetes who appears confused, they may be having a low blood sugar episode. Left untreated, the low blood sugar could lead to a diabetic coma. If the person is still able to follow instructions, give him or her something to drink or eat and call for an ambulance or 911.
- If you see someone with diabetes become unresponsive, call 911.
If you do call 911, let the responders know that the person has diabetes if theyre not able to communicate. If you do have diabetes, you may want to wear a medical identification item like a bracelet or necklace.
When you are taken to a healthcare facility, providers will do a physical examination and take blood to determine levels of glucose, ketones and other substances.
When To Call 911
- the persons blood glucose level is above 14 mmol/L and there are ketones present
- in the urine: medium to high level
- in the blood: a level higher than 1.5 mmol/L
Read Also: Does Insulin Inhibit Glucagon
Storage Conditions For Pre
In relation to the storage, stability and sterility of pre-loaded insulin syringes in the home, studies have shown these can remain stable and sterile at refrigerator temperatures for up to 28 days .
Pre-loaded insulin syringes should be stored in the main part of the refrigerator at between 2ºC and 8ºC, and should not be placed in the freezer or at the back of the refrigerator. The needle should point upwards in mixtures containing isophane insulin to prevent blockage by suspended substances in the insulin .
Lantus or Abasglar are unsuitable for use in pre-loaded syringes as it will become turbid . Tresiba and Toujeo are also not suitable and should not be drawn from the cartridge or the pre-filled pen into a syringe as it is available in different doses and can overdose the patient.
Syringes should be stored in a sealable container, and both syringes and container should be clearly labelled. If the patient is required to administer insulin more than once per day there should be a separate container for each administration time even if the doses that are utilised are the same.
Running Out Of Diabetes Medication Or Supplies
You should ensure you have sufficient supplies, including spares, wherever possible but there can be times when you may need emergency medication or supplies.
If you need medication and supplies right away you will need to get an emergency prescription.
If your surgery/medical centre is open, your GP should be able to write out a prescription
You will need to get to take the prescription to either a pharmacy that has the medication or supplies or it may be possible to get the medication/supplies from a hospital.
If your need for medication and/or supplies is needed whilst your surgery is closed, contact your surgerys out of hours service or contact NHS 111
- If you are away from homen, contact NHS 111.
Don’t Miss: Greek Yogurt Good For Diabetics
Hyperosmolar Hyperglycemic Nonketotic Syndrome
Hyperosmolar hyperglycemic nonketotic syndrome usually occurs after the diabetic has experienced and even recovered from infection, or has experienced unusual stress 1. Infections and stress cause the blood sugar levels in the body to rise to very high levels, and as a result, the body tries desperately to rid itself of this excess sugar. The body does this by producing large amounts of urine. According to the Mayo Clinic, the person will then urinate frequently and lose excess body fluids leading to dehydration, electrolyte imbalances, coma and even death. Symptoms of this emergency include confusion, weakness on one side of the body, increased or rapid heart rate, fever and hallucinations.
- Hyperosmolar hyperglycemic nonketotic syndrome usually occurs after the diabetic has experienced and even recovered from infection, or has experienced unusual stress 1.
- According to the Mayo Clinic, the person will then urinate frequently and lose excess body fluids leading to dehydration, electrolyte imbalances, coma and even death.
What Are The Risk Factors For Diabetic Coma
While anyone who has diabetes is at risk for a diabetic coma, the causes depend on the type of diabetes:
- People with Type 1 diabetes have a greater chance of going into a diabetic coma as a result of diabetic ketoacidosis or hypoglycemia. This is because people with Type 1 diabetes always need insulin and have a wider range in their blood glucose levels than people with Type 2 diabetes.
- People with Type 2 diabetes have a greater chance of going into a diabetic coma from diabetic hyperosmolar syndrome than from diabetic ketoacidosis or hypoglycemia.
Other risks that can lead to diabetic coma in anyone who has diabetes include:
- Surgery.
Don’t Miss: Metformin Cause Low Blood Sugar
Table : The Five Is That Cause Diabetic Ketoacidosis And Hyperosmolar Hyperglycemic State
Infection
Non-compliance with diabetic diet
Insulin lack
Pump failure, skipping insulin doses
The most common external cause of DKA is infectionusually a urinary tract infection, but diabetics are also at risk for pneumonia, cellulitis and more invasive skin infections.3
Infarction of any type of tissue can also lead to DKA. These include myocardial infarctions and cerebral infarctions . Less commonly, bowel ischemia can lead to DKA. Thus, adult patients over the ages of 3040 with suspected DKA should be questioned for any symptoms consistent with myocardial ischemia or infarction.
Type 1 diabetics may not have chest pain with acute MI, and may present with shortness of breath, weakness or other subtler symptoms, such as isolated nausea and vomiting, and should have a 12-lead ECG performed when appropriate.
A rapid stroke exam should also be performed in patients with weakness, visual changes, and any other stroke-like symptoms or altered mental status.
Pregnancy can cause DKA due to an increased insulin requirement. All females of childbearing age should be questioned about their pregnancy status.
Indiscretion with sugar, going off a diabetic diet, or use of alcohol can cause DKA when patients take in too many calories without accounting for them with appropriate doses of increased insulin.
As insulin levels decline, blood glucose levels increase, because cells cant transport glucose across their membranes without insulin.
Older People With Diabetes
Some older persons with diabetes may experience poor nutritional status with physical, social and psychological factors affecting intake. Education should continue to be offered to older persons, including dietary intervention age should not restrict access. Dietetic input is key to assess nutritional status and formulate individualised care plans which take into account the changes in nutrients that are required as the body ages. Guidelines and care planning should be further adapted for those living with dementia with a focus on maintaining nutritional intake and preventing malnutrition.
Recommended Reading: Can A Person With Diabetes Get A Tattoo
What Can Happen If Blood Sugars Are High
In the short term, high blood sugars can turn into diabetic ketoacidosis . This is an emergency condition that needs treatment right away. DKA can happen to kids with type 1 diabetes and, less often, kids with type 2 diabetes. Kids with type 2 diabetes also can get another type of emergency called hyperosmotic hyperglycemic state . Both conditions need treatment in the hospital and are very serious.
Untreated hyperglycemia can lead to serious health problems later in life. If it happens a lot, it can harm blood vessels, the heart, kidneys, eyes, and nerves.
Diabetic Emergency : Low Blood Sugar Or Severe Hypoglycemia
Hypoglycemia is a condition where the blood sugar levels drop down abnormally low. It normally occurs in patients taking diabetes medication to lower the sugar level. High alcohol consumption, missing or delaying meals, exercising without any adjustments in the food intake or insulin or overdosing the diabetic medication are some reasons for a hypoglycemic emergency.
- Pale skin which feels cold and clammy
- Feeling shaky or weak
- Rapid quick and pounding pulse
- Loss of consciousness
All these symptoms demand immediate sugar consumption. If you observe that the patient is not responding well to sugar and the condition is worsening call for a medical help.
Also Check: Incretin Effect In Type 2 Diabetes
Hyperosmolar Hyperglycemic Nonketotic Coma
HHNK is a true medical emergency, it usually occurs in older patients with type II or non-diagnosed diabetes. The syndrome is easily mistaken for diabetic ketoacidosis. But, HHNK differs from DKA in that their may be enough insulin present to prevent fat metabolism and the development of ketocacidosis as seen with DKA. However the amount of insulin may not be enough to prevent glucose use by the peripheral tissues or reduce glycogenesis by the liver.HHNK develops from sustained hyperglycemia that produces a hyperosmolar state. This is followed by an osmotic diuresis that results in marked dehydration and electrolyte losses. These patients often have an excessively high blood sugar level, up to 1000 mg/dl. This is considerably higher than DKA, simply because patients with HHNK are more dehydrated and have less ketone formation. HHNK tends to develop slowly, often over the course of several days and has a higher mortality rate than other diabetic conditions.The early signs and symptoms of HHNK include:
- Volume depletion including polydipsia and polyuria
- Orthostatic hypotension
Precipitating factors of HHNK coma may include:
- Advanced age
- Inadequate insulin secretion
- Increased insulin requirements
- Certain medication
Managing An Unconscious Diabetic
The pre-hospital management of an unconscious patient is clear properly manage the airway and providing ventilatory and circulatory support. Depending on local protocol, the initiation of an IV of lactated Ringers solution or saline to replenish electrolytes and fluid. The flow rate should depend on the patients BP and heart rate. Before glucose is administered, a blood sample should be drawn for the hospital lab.If alcoholism or other drug abuse is suspected then medical command may recommend the administration of thiamine, naloxone, or both before the administration of glucose.If IV access is unobtainable, subcutaneous or intramuscular injection of glucagon, may help raise serum glucose levels by stimulating the breakdown of liver glucagon. Glucagon is not effective on alcoholics and those with liver disease.Determining the cause of a diabetic emergency is sometimes difficult in the pre-hospital setting. When the EMS professional isn’t sure of the cause, all patients should receive glucose, if confirmed by field glucose testing.The difference in the signs and symptoms of the different diabetic emergencies should help determine the cause.
Recommended Reading: Sx Of High Blood Sugar
How Does It Work
A sensor the size of a £2 coin sits on the back of the arm with a probe just under the skin.
An overview of flash-GM
- Flash-GM requires an interstitial sensor the size of a £2 coin and a receiver. The sensor is self-inserted into the upper arm and lasts up to 14 days. It is attached to the body with clinical adhesives. It transmits glucose data to a receiver when it is scanned. The receiver may be a handset or the users mobile phone and it stores and displays their data.
- Various apps and software are available to present this data to the user and clinician using the cloud. They can then review and respond to glucose patterns.
- Interstitial glucose lags behind capillary blood glucose by 5-7 minutes. This means that when blood glucose is changing rapidly the measurements will differ. For this reason during episodes of hypoglycaemia patients and clinicians must revert to finger-prick testing.
- A new version of flash-GM has an optional alarm connected via Bluetooth to warn the wearer if their blood glucose is going too low. Scanning is still required to see the actual blood glucose level and trend arrow.
Having A Quality Conversation About Emotional Health And Diabetes
Its important to ask people about their emotional health at every appointment. Just because everything may seem okay the first time you ask, this can change over time. Dont think of this as an added extra. If someone is struggling emotionally, theyre going to find looking after their diabetes much more difficult
You May Like: Bananas And Diabetes 2

