What Is A Sliding Scale In Nursing
The term “sliding scale” refers to the progressive increase in pre-meal or nighttime insulin doses. The term sliding scale refers to the progressive increase in the pre-meal or nighttime insulin dose, based on pre-defined blood glucose ranges. Sliding scale insulin regimens approximate daily insulin requirements.
When To Call The Diabetes Team
You should always fix low blood sugars right away. Its also important to recognize when changes need to be made and adjust doses between clinic visits to reduce the chances of long term complications.
- Your childs blood sugars are worse after making a change in their insulin dose or if you make more than 3 changes in the dose since their last clinic visit
- Moderate or large ketones are present
Do you still have questions about when you should change your childs insulin doses? Contact the diabetes team at Childrens Diabetes Center, Childrens Hospital & Medical Center at for more information about insulin doses and pattern control.
Sliding Scale Therapy Approximates Daily Insulin Requirements
The term “sliding scale” refers to the progressive increase in pre-meal or nighttime insulin doses.
The term sliding scale refers to the progressive increase in the pre-meal or nighttime insulin dose, based on pre-defined blood glucose ranges. Sliding scale insulin regimens approximate daily insulin requirements.
Recommended Reading: Symptoms Of Sugar Being Too High
Total Daily Insulin Requirement
= 500 ÷ TDI = 1unit insulin/ 12 g CHO
This example above assumes that you have a constant response to insulin throughout the day. In reality, individual insulin sensitivity varies. Someone who is resistant in the morning, but sensitive at mid-day, will need to adjust the insulin-to-carbohydrate ratio at different meal times. In such a case, the background insulin dose would still be approximately 20 units however, the breakfast insulin-to-carbohydrate ratio might be breakfast 1:8 grams, lunch 1:15 grams and dinner 1:12 grams.
The insulin to carbohydrate ratio may vary during the day.
How Much Insulin To Take Per Carb
The average person will take about 1 unit of insulin for every 12 to 15 grams of carbohydrates consumed.
There is some variation to this, depending on how sensitive you are to insulin. For some people, this range is 1 unit for every 6 grams of carbohydrates, while for others, its 1 unit for every 30 grams of carbohydrates.
Recommended Reading: Prandial Insulin Types
What Is A Sliding Scale For Diabetes
Asked by: Thad Kutch
The term “sliding scale” refers to the progressive increase in pre-meal or nighttime insulin doses. The term sliding scale refers to the progressive increase in the pre-meal or nighttime insulin dose, based on pre-defined blood glucose ranges. Sliding scale insulin regimens approximate daily insulin requirements.
Combination With Other Antidiabetic Drugs
A combination therapy of insulin and other antidiabetic drugs appears to be most beneficial in people who are diabetic, who still have residual insulin secretory capacity. A combination of insulin therapy and sulfonylurea is more effective than insulin alone in treating people with type 2 diabetes after secondary failure to oral drugs, leading to better glucose profiles and/or decreased insulin needs.
You May Like: Low Blood Sugar Diagnosis
Description Of The Intervention
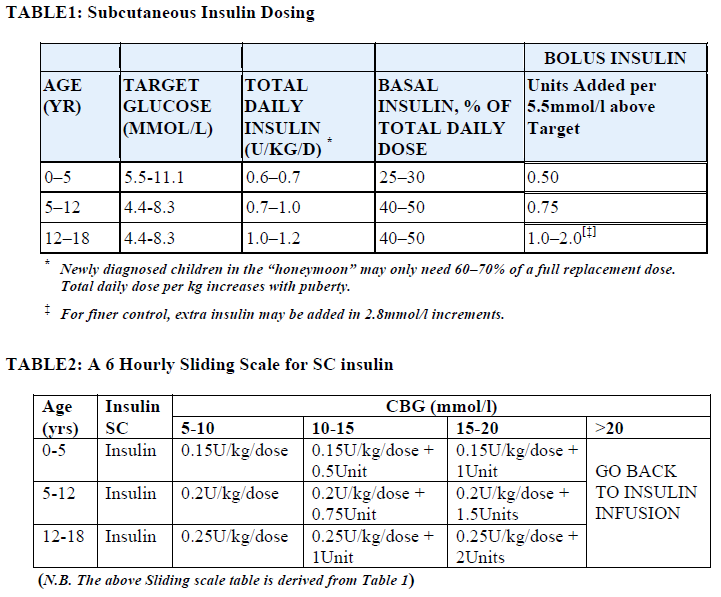
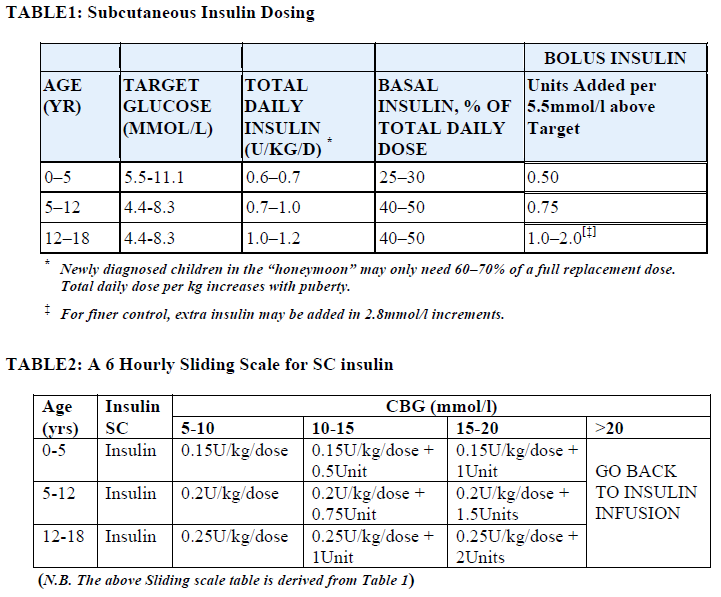
Four strategies are used to achieve glycaemic control in hospitalised diabetic people: basal insulin, prandial insulin, correctiondose insulin, and sliding scale insulin . These strategies are used to maintain optimal glucose levels . The main difference between these strategies is the intervention purpose: basal insulin administration inhibits hepatic glucose production and is mainly responsible for controlling fasting glucose prandial insulin aims to control postprandial glucose levels by promoting glucose disposal into the muscles and correction dose insulin is administered in addition to prandial insulin using an algorithmbased treatment to provide an adjustment to carbohydrate intake .
Sliding scale insulin is poorly defined and is used in different ways: traditionally, the insulin prescription is administered according to the measured blood glucose levels and therefore constitutes a reactive response to hyperglycaemia SSI is an intervention usually characterised by a subcutaneous administration , regardless of the timing of food intake, presence or absence of preexisting insulin administration, and sensitivity to insulin, without the acute illness consideration. The SSI scheme aims to maintain the glucose levels between 7.7 mmol/L and 10 mmol/L . Some physicians even employ this approach using longacting insulin analogues or neutral protamine Hagedorn insulin.
Adverse effects of the intervention
Things To Remember In Order To Change Insulin Doses:
- If the pattern happens at the blood sugar check before breakfast, change the long-acting insulin dose by 10 percent.
- If the pattern happens at the blood sugar check before lunch, change the breakfast rapid-acting insulin dose by 10 percent.
- If the pattern happens at the blood sugar check 2 to 3 hours after lunch, change the lunch rapid-acting insulin dose by 10 percent.
- If the pattern happens at the blood sugar check 2 to 3 hours after supper , change the supper rapid-acting insulin dose by 10 percent.
- If your blood sugar is above 180 two to three hours after a meal, ask yourself what caused this.
- Common reasons for high blood sugar 2 to 3 hours after eating are:
- Not taking insulin at least 15 minutes before eating
- Eating too much carbohydrate or too much quick-acting carbohydrate
- Not taking enough insulin to cover the carbohydrate
- Not eating protein or fat in your meal
- Eating a very high fat meal
If you rule out numbers 1 and 2, you may need to take more insulin next time.
- If the pattern is high blood sugar, you will increase the insulin dose that affects that column of blood sugars.
- If the pattern is low blood sugar, you will decrease the insulin dose that affects that column of blood sugars.
Don’t Miss: Metformin Administration
Sliding Scale Insulin Therapy Chart For Diabetics
Insulin doses are put on a chart named sliding scale. The physician generates this insulin chart with the help of the patient. A chart is prepared on how the individuals body reacts to insulin, his or her everyday routine, and carbs consumption that they would consent on. Insulin doses differ based upon two factors:
- Pre-meal levels of blood sugar: This generally arises on the left side on the novolog sliding scale chart, from low to high, with higher insulin dosages toward the bottom of the scale. The higher the blood glucose an individual has, the greater amount of insulin individuals would require coping with it.
- Mealtime insulin dosing: This generally arises along the scales top row. This top row indicates breakfast, lunch, and then dinner.
The dose of insulin changes all through the day this is due to the reason, insulin sensitivity. Insulin sensitivity is the way how the body reacts to insulin, which may alter with the progression of the day. The meal composition also modifies during the day, and the physician may keep it in mind.
Ways To Determine Dosage Of Insulin
Insulin is the groundwork of treatment for a majority of diabetics. If a person is diabetic, his or her body either fails to produce sufficient insulin or effectively make use of insulin. Individuals with type 1 diabetes and few individuals with type 2 diabetes ought to take numerous injections of insulin each day. Insulin normalizes blood glucose and avoids spikes in glucose levels. This also assists in preventing complications. The insulin amount a person can take can be determined in different ways:
Also Read: Energy Drinks For Diabetics
Recommended Reading: Metformin Dosage 500 Mg
Humalog Sliding Scale Insulin Coverage
As Humalog is a short-acting insulin that is typically prescribed to be taken before mealtime, it is important to track sugar levels with the help of a special Humalog sliding scale chart. With its use, it is possible to identify how many units of insulin are needed to get glucose back to normal and guarantee a positive result at the end.
You may see the example of the insulin sliding scale below:
| Blood Sugar Result | |
|---|---|
| 10 units of Humalog Insulin | |
| 351-400 | 12 units of Humalog Insulin |
Measuring blood sugar is vital because an insulin dose cannot be injected during the low blood sugar episode . There are a few recommendations provided by medical experts on how not to experience extremely low or high blood sugar levels:
Dont hesitate to talk to a specialist if you are unsure how much insulin you need to feel better. Self-treatments may be dangerous, so dont try changing the dose on your own.
Advantages Of Intensive Insulin Regimens
- While intensive regimens require more calculation at each meal, they allow for more flexibility in timing and in the amount of carbohydrate content in meals and snacks.
- An accurate insulin dose will also result in better blood glucose control with fewer high and low blood sugars.
- Changes in activity and stress can be accommodated without sacrificing glucose control.
- Over time, high blood glucose correction can be separated from the food coverage. For example, if your blood sugar is very high , you can delay your meal and give yourself a correcting dose. Once your blood sugar falls below 200 mg/dl, you can inject your meal insulin and then eat.
- Learning these important skills will make managing your diabetes easier.
Also Check: Can Metformin Cause Joint Pain
How Much Insulin To Take For Bodybuilding
Injecting insulin is not a safe approach to weight training. However, some bodybuilders will inject it as a performance-enhancing drug. They believe injecting insulin will allow energy in the form of glucose to enter their cells so they can build more muscle.
This practice is unsafe and can lead to severe and potentially life threatening hypoglycemia, according to 2019 research.
You should not take insulin unless you have diabetes. If you do have diabetes, talk with your doctor about how your training regimen may affect your blood sugar levels.
Detection In Biological Fluids
Insulin is often measured in serum, plasma or blood in order to monitor therapy in people who are diabetic, confirm a diagnosis of poisoning in hospitalized persons or assist in a medicolegal investigation of suspicious death. Interpretation of the resulting insulin concentrations is complex, given the numerous types of insulin available, various routes of administration, the presence of anti-insulin antibodies in insulin-dependent diabetics and the ex vivo instability of the drug. Other potential confounding factors include the wide-ranging cross-reactivity of commercial insulin immunoassays for the biosynthetic insulin analogs, the use of high-dose intravenous insulin as an antidote to antihypertensive drug overdosage and postmortem redistribution of insulin within the body. The use of a chromatographic technique for insulin assay may be preferable to immunoassay in some circumstances, to avoid the issue of cross-reactivity affecting the quantitative result and also to assist identifying the specific type of insulin in the specimen.
Also Check: Metformin 500 Side Effects
Disadvantages Of Sliding Scale Insulin
SSI is often implemented in hospitals where it’s unclear how much the patient needs, says Kasia Lipska, MD, a Yale Medicine endocrinologist. This is because unlike fixed-dose insulin regimens which involve taking the same amount of insulin at every meal SSI allows healthcare providers to continually tweak the insulin dosage based on the patient’s pre-meal blood sugar.
However, sliding-scale insulin has still started to fall out of favor for a variety of reasons, such as:
Calculating A Bolus Dose For High Blood Glucose
- Use the high blood glucose correction factor, also called correction factor or sensitivity. Use this to calculate the correction bolus.
- Correction factor is how much 1 unit of rapid-acting insulin will reduce the blood glucose number.
- The target number is the blood glucose number that you want.
NOTE: You should not need to correct a high blood glucose with each meal. If you need insulin to correct high blood glucose often, the insulin dose may need to be changed at each meal. The goal is to predict and prevent high blood glucose.
Read Also: Metformin And A1c Levels
High Blood Sugar Correction
In step two, you will account for your current blood glucose concentration. It needs to be measured directly before the meal with your glucose meter. Your doctor should tell you what your target level of your premeal blood glucose is. Depending on the guidelines, your premeal glucose target may range from 80 to 130 mg/dL. If you measure your blood glucose in mmol/l, you can use our blood sugar converter. The third value you need to know is the insulin sensitivity factor. Again, it can be determined by your doctor, or you can calculate it when the total daily dose of insulin is known . Insulin sensitivity factor tells you by how many points one unit of insulin will decrease your blood glucose by.
How Much Insulin Is Too Much To Take For High Blood Sugar
Ideally, you should be able to correct your blood sugar with an appropriate insulin dose. How much insulin is too much varies based on how sensitive your body is to insulin.
If you have higher-than-expected blood sugar , you should check your urine for ketones. The presence of ketones suggests your bodys cells are having trouble getting enough glucose. You could be at risk for a serious condition called diabetic ketoacidosis if you have ketones in your urine.
In this instance, you need extra help correcting your blood sugar. You should seek emergency medical attention instead of trying to keep injecting insulin to lower your blood sugar.
Recommended Reading: Metformin Dosage For Ketosis
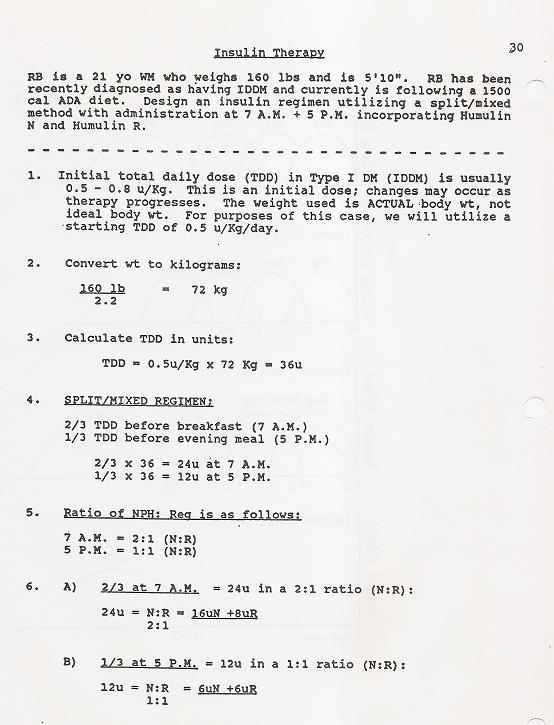
You’ll Need To Calculate Some Of Your Insulin Doses
You’ll also need to know some basic things about insulin. For example, 40-50% of the total daily insulin dose is to replace insulin overnight.
Your provider will prescribe an insulin dose regimen for you however, you still need to calculate some of your insulin doses. Your insulin dose regimen provides formulas that allow you to calculate how much bolus insulin to take at meals and snacks, or to correct high blood sugars.
Ineffective Blood Sugar Control
Some studies found SSI often causes fluctuations in blood sugar levels. This is because many scales are designed to only correct high pre-meal blood sugar levels, and may not account for them rising further after a meal, according to Peter.
In fact, a small 2006 study found 84% of administered SSI doses failed to correct excess blood sugar in hospital patients, and a 2015 meta-analysis found the use of SSI frequently led to high blood sugar.
Additionally, if you skip a meal or are simply more sensitive to insulin on a particular day, the doses on your sliding scale might be excessive, which can then lead to a dangerous drop in blood sugar. Hence why a 2012 study found sliding scale insulin therapy can cause unpredictable drops in blood sugar levels.
Don’t Miss: What Happens If You Stop Taking Diabetes Medication
How To Calculate Insulin Dose
For patients undergoing an intensive insulin therapy, their insulin dose regimen is partially prescribed by the doctor, but there are still some calculations that need to be made before establishing the dose of insulin. This insulin dosage calculator provides formulas that allow you to calculate how much bolus insulin you should take for your meal. It helps you to account for the carbohydrate content of your meal, and to correct for high blood sugar concentrations.To do this, you need to know the following information:
- the carbohydrate content of your meal
- the carbohydrate ratio, which tells you how many grams of carbohydrates are covered by one unit of insulin
- your current blood glucose concentration
- your target blood glucose concentration
- the insulin sensitivity factor, which tells you by how many points one unit of insulin will decrease your blood glucose
The two elements above that are not in bold can be calculated using your total daily insulin dose.When you know all the necessary information, your mealtime insulin dose can be calculated in three easy steps:
Step one – carbohydrate coverage
BG is blood glucose
ISF is insulin sensitivity factor
Please note, that this calculator will not work if your current blood glucose is below your target blood glucose.
Assessing And Changing An Isf
Assess correction insulin against the ISF formula: E.g. Sandy has high readings using an ISF of 3. The formula suggests an ISF of 1. In this situation consider a new ISF of 2 to start, as it is safer. If needed, the ISF can change to 1 in the future.
Assess correction insulin used alone without meal bolus:If the client took correction insulin but had no meal , assess if it worked. E.g. 12 mmol at breakfast, gave correction but no meal eaten and no food bolus, by lunch was 6.5 mmol/L. This correction worked. Clients are often hesitant to report times they’ve corrected but missed the meal. Be sure to let them know this could be useful information if they had any to share.
You May Like: Does Type 1 Diabetes Go Away
Data Collection And Analysis
Two review authors independently extracted data, assessed trials for risk of bias, and evaluated the overall certainty of evidence utilising the GRADE instrument. We synthesised data using a randomeffects model metaanalysis with 95% prediction intervals, if possible, or descriptive analysis, as appropriate.

