Adjusting Insulin Sensitivity Factor
Correction insulin is an extra dose of insulin given to reduce high blood glucose. The correction factor, or Insulin Sensitivity Factor , specifies how much insulin is needed to correct blood glucose back to the target range. It is expressed as a ratio, such as 1:3, or 1:15, where the second number represents how much the blood glucose drops when 1 unit of rapid-acting insulin is given. For example, an ISF of 1:3 means one unit of insulin would drop the blood glucose by 3 mmol/L an ISF of 1:15 means one unit of insulin would drop the blood glucose by 15 mmol/L. We often talk about ISF in terms of this second number alone, as in my childs ISF is 3. The bolus calculator in an insulin pump uses a Correction Formula to calculate how many units of insulin to deliver for an above-target blood glucose reading: Correction Insulin = Current BG Target ISF It is informative, but not necessary, for you to understand how the pump uses this correction formula. What IS important is to understand the effect of changes to the ISF setting, as outlined below.Continue reading > >
Insulin Resistance Diet Tips
When it comes to treating insulin resistance, controlling your diet and getting regular physical activity are crucial. It is important to get proper dietary counseling and monitor your eating habits. Here you will find some tips which will help you not only control the insulin resistance symptoms, but also affect your health positively:
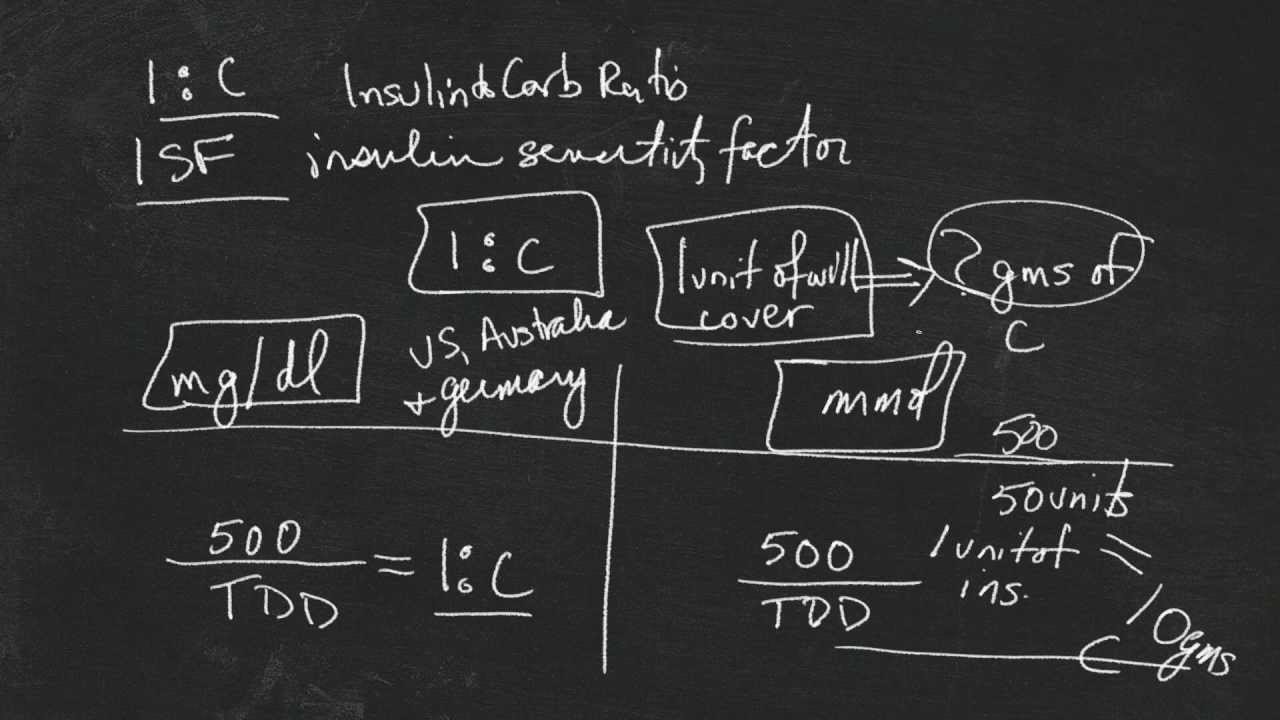
Total Daily Insulin Requirement:
= 500 ÷ TDI = 1unit insulin/ 12 g CHO
This example above assumes that you have a constant response to insulin throughout the day. In reality, individual insulin sensitivity varies. Someone who is resistant in the morning, but sensitive at mid-day, will need to adjust the insulin-to-carbohydrate ratio at different meal times. In such a case, the background insulin dose would still be approximately 20 units however, the breakfast insulin-to-carbohydrate ratio might be breakfast 1:8 grams, lunch 1:15 grams and dinner 1:12 grams.
The insulin to carbohydrate ratio may vary during the day.
Recommended Reading: Which Pancreatic Cells Release Insulin And Glucagon
How To Test For Insulin Sensitivity Factor
A person should test their insulin sensitivity factor every day.
To do this, they will:
If the ratio is correct, the blood sugar level of the person should be within a 40-point range of their target.
They may need to adjust their correction factor if it is out of this range on two or more occasions. The person should talk about this with their doctor. To confirm the results, they may need further testing.
If blood sugar levels drop below 70 mg / dL, the person should, for example, stop the evaluation and treat their low blood sugar by eating or drinking something.
Before taking further action, someone who feels they need to change their insulin sensitivity factor should talk to a healthcare provider.
Treating Diabetes With Insulin
There are three main types of diabetes:
- Type 1 – damage to the pancreatic cells means that little to no insulin is produced.
- Type 2– insulin production is inadequate, or body cells are resistant , or both.
- Gestational diabetes – diabetes that occurs in pregnant women without a prior history of diabetes. Usually disappears after giving birth.
Insulin can be used as a treatment for all three types of diabetes. Insulin is typically given by the injection under the skin. Patients with insulin-dependent diabetes usually require some base level of insulin throughout the day , as well as some short-acting insulin to cover meals . There are many different types of insulin, and just as many different treatment strategies. Which one an individual needs should be established by a doctor. Among the strategies are conventional insulin therapy, for patients with a regular lifestyle where insulin can be given in regular, fixed doses, and intensive insulin therapy, where the patient decides on their own mealtime insulin dose, which depends on the carbohydrate content of the meal, their current blood sugar concentration, and the amount of physical activity performed.
Don’t Miss: Glucose Definition Medical
Creating An Insulin Sensitivity Factor
Note: TDD = Total Daily Dose of insulin
100/TDD = ISF if using rapid insulin
83/TDD= ISF is using regular/Toronto insulin
EXAMPLE ONE: Teddy, TDD 33, takes rapid insulin
100/33= ISF of 3
1 unit rapid insulin is expected to lower Teddys blood sugar by about 3 mmol/L.
EXAMPLE TWO: Bear, TDD 80, takes regular insulin
83/80= ISF of 1
1 unit of regular is expected to lower Bears sugar by 1 mmol/L. This is aggressive a safer start may be an ISF of 2.
How To Calculate Insulin Sensitivity Factor
Health-care professionals use the 1500 rule to calculate insulin sensitivity factor for people who use Regular insulin. The 1500 rule works as follows: Divide 1500 by the total daily dose of Regular insulin, in units. For example, if a persons total daily dose is 30 units of Regular insulin, his insulin sensitivity factor would be 50 . So one unit of Regular insulin would be estimated to lower his blood glucose by 50 mg/dl.
Health-care professionals use the 1800 rule to calculate insulin sensitivity factor for people who use the rapid-acting insulin analogs lispro , aspart , and glulisine . This is done by dividing 1800 by the total daily dose of rapid-acting insulin. If the total daily insulin dose is 40 units, the insulin sensitivity factor would be 1800 divided by 40, or 45.
Insulin sensitivity factor can be calculated only for people with Type 1 diabetes. It cannot be calculated reliably for people with Type 2 diabetes, whose pancreases often still make some insulin and who have varying degrees of insulin resistance.
Disclaimer Statements: Statements and opinions expressed on this Web site are those of the authors and not necessarily those of the publishers or advertisers. The information provided on this Web site should not be construed as medical instruction. Consult appropriate health-care professionals before taking action based on this information.
Recommended Reading: What Is A Normal A1c For A Non Diabetic
How Do You Determine Insulin Dosage
Once you know how sensitive you are to insulin, you can figure out how much insulin you need to give yourself to lower your blood sugar by a certain amount.
For example, if your blood sugar is 200 mg/dL and youd like to use your short-acting insulin to lower it to 125 mg/dL, youd need your blood sugar to drop by 75 mg/dL.
From the insulin sensitivity factor calculation, you know that your short-acting insulin sensitivity factor is 1:60. In other words, one unit of short-acting insulin lowers your blood sugar by about 60 mg/dL.
How much insulin do you then need to lower your blood sugar by 75 mg/dL?
Youll need to divide the number of mg/dL you want to lower, which is 75, by the number from your insulin sensitivity factor calculation, which is 60. The answer of 1.25 tells you that you need to take 1.25 units of short-acting insulin to lower your blood sugar by 75 mg/dL.
These are rough calculations that are used by people with type 1 diabetes. If you have type 2 diabetes, youll need to check with your doctor for guidance.
What Is Insulin Sensitivity Factor
To remain healthy, a person with diabetes needs to keep their blood sugar levels within a target range. Insulin may avoid an increase in blood sugar levels to dangerously high levels.
Their blood sugar levels drops when a person takes insulin. If blood sugar levels drop too high, however, this can be dangerous, too.
Insulin sensitivity or correction factor refers to the amount of milligrams per deciliter in which blood sugar levels decrease when 1 unit of insulin is taken by a person.
This number can be used by a person with type 1 diabetes when determining how much insulin they need to keep their blood sugar levels within the target range.
Typically, they apply this amount to their current dose of premeal insulin. Compared to their target, the amount would depend on how much higher the blood sugar level of the individual is.
To correct their personal target blood sugar levels, a person will work with their physician.
The goal level should be as similar as possible to the levels that a person without diabetes will have, according to the ADA.
These are:
- Between 70130 mg/dL before a meal
- No higher than 180 mg/dL up to 2 hours after a meal
Insulin treatment plans vary, but most people with type 1 diabetes now use two types of insulin:
- Basal insulin, a longer-acting form that keeps blood sugar levels stable between meals and when sleeping.
- Bolus insulin, a faster-acting form to regulate levels around mealtimes.
Also Check: Does Nicotine Raise Blood Sugar
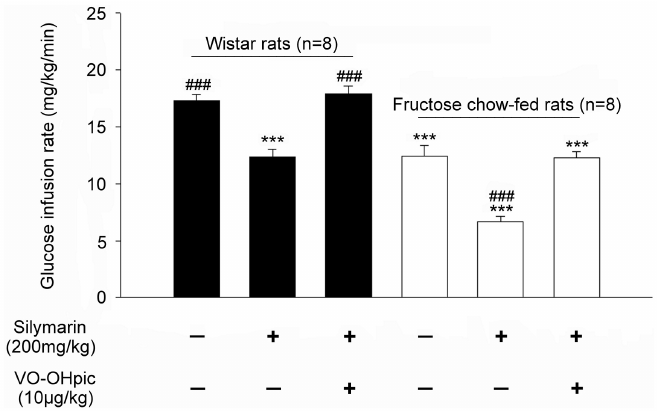
How Does This Insulin Sensitivity Quicki Calculator Work
This health tool determines insulin sensitivity based on fasting insulin and fasting glucose levels obtained from blood sample. QUICKI stands for Quantitative Insulin Sensitivity Check Index.
The index is defined as the inverse of the sum of the logarithms of fasting insulin and fasting glucose:
QUICKI = 1 / + log)
The calculation is used for measuring insulin sensitivity. The latter is the inverse of insulin resistance.
There are two established methods for determining insulin sensitivity: the glucose clamp and the minimal model analysis. However, these are more complicated to implement during clinical research, thus QUICKI is preferred.
By using a fasting blood sample, fasting insulin in µU/mL and fasting glucose in mg/dL are obtained. The insulin sensitivity QUICKI calculator allows users to input glucose in mmol/L as well and the converts it.
Obtainable values for QUICKI range between 0.45 in healthy individuals and 0.30 in diabetics. Lower values reflect greater resistance with values below 0.339 indicating insulin resistance which is associated with obesity and cardiovascular risk factors.
The original study performed hyperinsulinemic isoglycemic glucose clamp and insulin-modified frequently sampled IV glucose tolerance tests on a cohort of 56 patients .
The main discovery was that both fasting insulin and glucose values carry critical information about sensitivity.
Also, QUICKI and HOMA-IR compensate for fasting hyperglycemia.
Example #: Carbohydrate Coverage At A Meal
First, you have to calculate the carbohydrate coverage insulin dose using this formula:
CHO insulin dose = Total grams of CHO in the meal ÷ grams of CHO disposed by 1 unit of insulin .
For Example #1, assume:
- You are going to eat 60 grams of carbohydrate for lunch
- Your Insulin: CHO ratio is 1:10
To get the CHO insulin dose, plug the numbers into the formula:
CHO insulin dose =
- The carbohydrate coverage dose is 6 units of rapid acting insulin.
- The high blood sugar correction dose is 2 units of rapid acting insulin.
Now, add the two doses together to calculate your total meal dose.
Carbohydrate coverage dose + high sugar correction dose = 8 units total meal dose!
The total lunch insulin dose is 8 units of rapid acting insulin.
Read Also: Hormone Sensitive Lipase Insulin
Nsulin Sensitivity & Carbohydrate Ratio Calculator
The Insulin Sensitivity Factor is the number of mg/dL one unit of insulin lowers glucose: 1500* / Total Daily Dose of Insulin = ISF The Carbohydrate Ratio is the number of carbohydrate grams covered by one unit of insulin: 450 / Total Daily Dose of Insulin To use the insulin sensitivity factor calculate the difference between the current blood sugar and the desired blood sugar. Then divide the result by the sensitivity factor. The result is the amount of insulin that needs to be added or subtracted from the premeal insulin dose. Example: Current blood sugar is 140, target blood sugar is 100. Insulin sensitivity factor is 20. Correction = /20 = 2 *The 1500 Rule was developed by Dr. Paul C. Davidson, Medical Director of the Diabetes Treatment Center in Atlanta. All calculations must be confirmed before use. The suggested results are not a substitute for clinical judgment. Neither OBFocus.com nor any other party involved in the preparation or publication of this site shall be liable for any special, consequential, or exemplary damages resulting in whole or part from any user’s use of or reliance upon this material.Continue reading > >
Assessing And Adjusting Insulin Sensitivity Factor
Correction insulin is an extra dose of insulin given to reduce high blood glucose. The correction factor, or Insulin Sensitivity Factor , specifies how much insulin is needed to correct blood glucose back to the target range. It is expressed as a ratio, such as 1:3, or 1:15, where the second number represents how much the blood glucose drops when 1 unit of rapid-acting insulin is given.
For example, an ISF of 1:3 means one unit of insulin would drop the blood glucose by 3 mmol/L an ISF of 1:15 means one unit of insulin would drop the blood glucose by 15 mmol/L. We often talk about ISF in terms of this second number alone, as in my childs ISF is 3.
The bolus calculator in an insulin pump uses a Correction Formula to calculate how many units of insulin to deliver for an above-target blood glucose reading:
Correction Insulin =
That is, the amount of insulin given to correct a high blood sugar is equal to the current BG minus the target BG, then divided by the ISF.
It is informative, but not necessary, for you to understand how the pump uses this correction formula. What IS important is to understand the effect of changes to the ISF setting, as outlined below.
Also Check: Is Ginger Ale Good For Diabetics
Insulin Sensitivity Factor And Type 2 Diabetes
Insulin sensitivity factor assessments are only useful for people with type 1 diabetes who no longer produce insulin.
People with type 2 diabetes may still produce some amounts of insulin in their pancreas, and so they cannot calculate their insulin sensitivity factor reliably.
People should be sure to talk to their doctor to find out what is best for them.
People with type 2 diabetes should focus first on diet and lifestyle changes to lower their blood sugar levels.
After this, a doctor may recommend medications, such as metformin. This works by reducing the amount of glucose the body releases into the bloodstream and makes the bodys cells more responsive to insulin.
How To Calculate Your Insulin Sensitivity Factor
There are two ways to calculate your insulin sensitivity factor. One method will help you determine your sensitivity to regular insulin, and the other will help you know your sensitivity to short-acting insulin.
Regular insulin. Regular insulin is a synthetic hormone that the body uses to process sugar that enters the bloodstream as part of the digestive process. It starts working within 30 minutes to an hour after intake, and it takes about two to four hours before the medication achieves maximum effectiveness. The effectiveness lasts for six to eight hours. Regular insulin comes in three forms:
- An injectable solution
- An inhalable powder
- An intravenous solution
To calculate your insulin sensitivity factor for regular insulin, use the â1500 rule.â It will help you know how much your blood sugar will drop per unit of regular insulin. For example, if your recommended daily dose of regular insulin is 30 units, divide that into 1500 to get 50. The interpretation is that your insulin sensitivity factor is 1:50. This means that one unit of regular insulin lowers your blood sugar levels by about 50 milligrams per deciliter.
Short-acting insulin. This type of insulin takes a shorter time to affect your glucose levels than regular insulin. It begins to work within 30 minutes, which means you should take the injection 30 minutes before taking a meal. The insulin reaches its maximum effect two to five hours later and can last for as long as six to eight hours.
Also Check: Can Diabetics Eat Macaroni And Cheese
Determining Patients Insulin Sensitivity Factor
A formula to help your patients determine their Insulin Sensitivity Factor. In order for your insulin patients to make corrections for elevated blood sugars, they need to determine how sensitive they are to their insulin. This formula provides an easy way to find out how much insulin they need to lower their blood sugars to the goal you have set for them.
Do I Need To Know The Carbohydrate Content Of Each Meal
You do need to know the carbohydrate content of your meal to use this calculator. It can be estimated by reading food labels or using tables and guidelines created for diabetic patients. When using the Nutrition Facts panel, you should always look for total carbohydrate section. Some labels might also have information about the carbohydrate units. One unit is usually 15 grams of carbohydrate .
Also Check: Dose Of Metformin For Prediabetes

