Xiv Glucagon’s Effect On Autophagy
In 1955, the legendary Christian de Duve identified saclike particles in the cytoplasm of rat liver slices, which positively stained for acid phosphatase . Electromicroscopy then demonstrated that the particles are surrounded by a lipoprotein membrane, classifying them as yet unknown intracellular organelles . The presence and quantity of acid hydrolases in these organelles, which were appropriately named lysosomes, pointed to a role in cellular autophagy , which was later confirmed experimentally . The lysosomes can be divided in several subtypes, such as membrane-lined bodies filled with glycogen , membrane-lined bodies containing amorphous material of various electron density , or autophagic vacuoles containing cell organelles at various stages .
Camp Effects On Electrical Activity And Ca2+ Signalling
It has long been known that cAMP promotes electrical activity with Ca2+ signalling in islets and -cells. These effects are largely explained by the action of PKA on KATP and voltage-dependent Ca2+ channels. Closure of KATP channels may also be facilitated by Epac2, which binds to the SUR1 subunit of the channel. The underlying mechanism is unclear but has been suggested to involve activation of phospholipase C- with concomitant lowering of PIP2, which in turn shifts the ATP-sensitivity of the channel. cAMP has been found to contribute to glucose- and GLP-1-induced -cell depolarization also via PKA-independent activation of the non-selective cation channel TRPM2, and via activation of niflumic acid-sensitive Cl channels, supposedly involved in -cell sensing of gradual changes of the glucose concentration.
The effects of cAMP on -cell Ca2+ signalling is not restricted to regulation of membrane potential and voltage-dependent Ca2+ influx, but also involve mobilization of the ion from intracellular stores. The latter effect is essentially due to PKA-induced sensitization of IP3 receptors. Epac has been proposed to promote Ca2+-induced Ca2+ release via ryanodine receptors, but later studies from the same laboratory instead favour IP3-gated Ca2+ release secondary to the Epac/Rap1-mediated activation of phospholipase C-.
How Do Different Glp
Abstract Glucagon-like peptide-1 mimetics have been developed to overcome the pharmacokinetic limitations of GLP-1 for the treatment of type 2 diabetes. Their mechanisms of action and clinical effects appear particularly interesting because they target the main pathophysiologic mechanisms involved in type 2 diabetes. GLP-1 receptor agonists are more powerful and are particularly advantageous by their weight loss-inducing capacity, whereas dipeptidyl peptidase IV inhibitors exhibit a better tolerance profile. However, their ultimate role is still to be defined in the therapeutic strategy of type 2 diabetes. Preview Unable to display preview. Download preview PDF.Continue reading > >
Read Also: Can A Diabetic Eat A Banana
Regulation Of Blood Glucose Levels By Thyroid Hormones
The basal metabolic rate, which is the amount of calories required by the body at rest, is determined by two hormones produced by the thyroid gland: thyroxine, also known as tetraiodothyronine or T4, and triiodothyronine, also known as T3. These hormones affect nearly every cell in the body except for the adult brain, uterus, testes, blood cells, and spleen. They are transported across the plasma membrane of target cells and bind to receptors on the mitochondria resulting in increased ATP production. In the nucleus, T3 and T4activate genes involved in energy production and glucose oxidation. This results in increased rates of metabolism and body heat production, which is known as the hormones calorigenic effect.
Disorders can arise from both the underproduction and overproduction of thyroid hormones. Hypothyroidism, underproduction of the thyroid hormones, can cause a low metabolic rate leading to weight gain, sensitivity to cold, and reduced mental activity, among other symptoms. In children, hypothyroidism can cause cretinism, which can lead to mental retardation and growth defects. Hyperthyroidism, the overproduction of thyroid hormones, can lead to an increased metabolic rate and its effects: weight loss, excess heat production, sweating, and an increased heart rate. Graves disease is one example of a hyperthyroid condition.
What Happens If I Have Too Little Glucagon
Unusual cases of deficiency of glucagon secretion have been reported in babies. This results in severely low blood glucose which cannot be controlled without administering glucagon.
Glucagon can be given by injection to restore blood glucose lowered by insulin . It can increase glucose release from glycogen stores more than insulin can suppress it. The effect of glucagon is limited, so it is very important to eat a carbohydrate meal once the person has recovered enough to eat safely.
You May Like: How Does High Blood Sugar Feel
Recommended Reading: Is Greek Yogurt Okay For Diabetics
Role Of Camp In Glucose
Before discussing the mechanisms underlying cAMP amplification of glucose-stimulated insulin secretion in more detail, it should be pointed out that cAMP is significant also for the ability of glucose to initiate insulin secretion. When -cells are exposed to a step increase of the glucose concentration there is an initial, distinct increase of insulin release lasting for a few minutes followed by a decline and increase to a new steady-state . This pattern has been explained by the release of different granule pools, where the first phase corresponds to exocytosis of readily releasable granules and can be triggered by i elevation alone, whereas the second phase reflects energy-requiring recruitment and priming of new granules for exocytosis. However, such distinction has been questioned, because both phases of secretion seem to involve the triggering and amplifying pathways, and when studied with sufficient temporal resolution, it is evident that the second phase secretion consists of pronounced pulses with a 2- to 5-minute periodicity, as if the first phase were recurring repeatedly.,
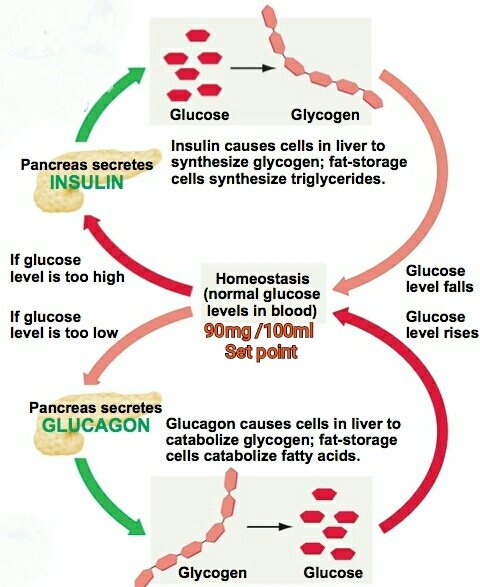
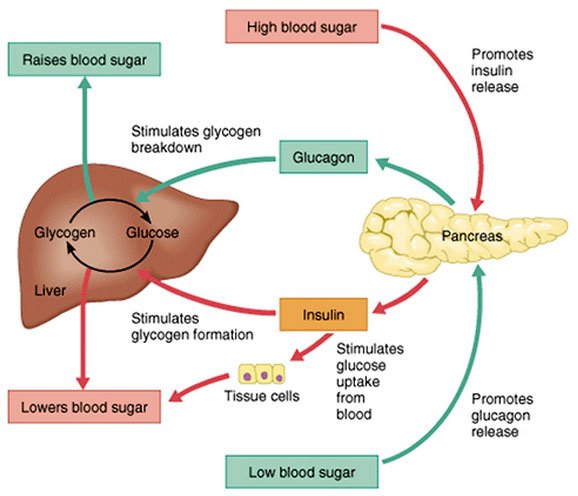
The Role Of Glucagon In Blood Glucose Control
The effect of glucagon is to make the liver release the glucose it has stored in its cells into the bloodstream, with the net effect of increasing blood glucose. Glucagon also induces the liver to make glucose out of building blocks obtained from other nutrients found in the body .
Our bodies desire blood glucose to be maintained between 70 mg/dl and 110 mg/dl . Below 70 is termed “hypoglycemia.” Above 110 can be normal if you have eaten within 2 to 3 hours. That is why your doctor wants to measure your blood glucose while you are fasting…it should be between 70 and 110. Even after you have eaten, however, your glucose should be below 180. Above 180 is termed “hyperglycemia” . If your 2 two blood sugar measurements above 200 after drinking a sugar-water drink , then you are diagnosed with diabetes.
Recommended Reading: Can Type 2 Diabetics Eat Bananas
Glucose Appearance And Disappearance
Rates of glucose appearance and disappearance did not differ before glucose ingestion on the 2 study days . As glucose concentrations increased more after glucose ingestion on the suppressed than on the nonsuppressed study day, this by definition meant that glucose appearance exceeded disappearance. The increase in glucose appearance and disappearance above basal over the 6 h of study did not differ on the nonsuppressed and suppressed study days. However, glucose appearance during the first 2 h was slightly higher on the nonsuppressed compared with the suppressed study days .
Urinary acetaminophenglucuronide specific activity and UDP glucose flux on the glucagon-suppressed and nonsuppressed study days. A glucose drink was ingested at time zero.
Chromaffin Tissue Of The Medulla
The adrenal gland of mammals is composed of an outer region, the cortex, which consists of adrenocortical tissue that secretes steroid hormones , and an inner region, the medulla, which is composed of chromaffin tissue, so called because its cells contain granules that can be characteristically coloured by certain reagents. Chromaffin tissue secretes two hormones, epinephrine and norepinephrine, which are members of a class of compounds called catecholamines. Both chromaffin and adrenocortical tissues are present in gnathostomes and probably in agnathans , but the tissues vary in the degree to which they are associated, being completely separated in elasmobranch fishes.
Norepinephrine and epinephrine are each composed of a benzene ring containing two hydroxyl groups and an amine side chain.
During the synthesis of these hormones, a sequence of enzyme-catalyzed reactions in the chromaffin granules of the secretory tissue transforms tyrosine into a compound commonly called dopa , which then forms dopamine dopamine then is hydroxylated to form norepinephrine. Epinephrine is formed from norepinephrine by methylation , a reaction that occurs outside the granules of the chromaffin cells. Norepinephrine is also formed in certain neurons, where it functions as a neurotransmitter.
Read Also: Symptoms Of Diabetes Onset In Adults
Ok But What Do They Have To Do With Each Other
Now you know insulin and glucagon have pretty similar jobs. But how do these hormones work together?
When theyre doing their jobs correctly, they work in perfect balance: Insulin prevents glucose levels from getting too high while glucagon prevents them from getting too low.
Both need to be effective for your blood sugar levels to stay, well, as close to perfect as possible.
When insulin and glucagon arent working correctly, things get complicated. If one or the other isnt properly regulating glucose levels, those levels will get thrown off, which can have some pretty serious side effects.
Iv Transcriptional Regulation Of Preproglucagon
Glucagon can be found in the developing mouse pancreas as early as E9.5 and as such represents in rodents the first hormone detected in the endocrine pancreas . In the developing human pancreas however, insulin can be detected as early as gestational week 8 while glucagon positive cells emerge 1 week later . During the development of the pancreas, the differentiation of the -cells is under tight control of a series of transcription factors, such as Prox1, Pax6, Arx, Nkx2.2, NeuroD1/Beta2, Isl1, Sox4, and Foxa2 . These transcription factors, especially Pax6, Arx, and Foxa2, are essential for -cell development since mice lacking any of these factors do not produce functional -cells .
Tissue specificity in Gcg expression is achieved through cell type specific binding of distinct transcription factors to selective DNA control elements in the Gcg promoter region to activate or inhibit Gcg expression . Accordingly, the rat Gcg promoter comprises at least six DNA control elements located within a 0.3 kb region upstream of the ATG start codon of Gcg . The control elements can be divided into an essential promoter, which comprises the TATA box as well as the G1 and G4 elements, which are crucial for -cell specific expression of Gcg and the more distally located enhancer elements G5, G2, G3, and CRE . The Gcg DNA control elements are targeted by more than half a dozen homeodomain proteins which either activate or inhibit Gcg expression .
Read Also: Type 2 Diabetes And Dizziness
The New Biology And Pharmacology Of Glucagon
Institute for Diabetes and Obesity, Helmholtz Diabetes Center, Helmholtz Zentrum München, German Research Center for Environmental Health, Neuherberg, Germany German Center for Diabetes Research, Neuherberg, Germany Department of Chemistry, Indiana University, Bloomington, Indiana Division of Metabolic Diseases, Technische Universität München, Munich, Germany
Institute for Diabetes and Obesity, Helmholtz Diabetes Center, Helmholtz Zentrum München, German Research Center for Environmental Health, Neuherberg, Germany German Center for Diabetes Research, Neuherberg, Germany Department of Chemistry, Indiana University, Bloomington, Indiana Division of Metabolic Diseases, Technische Universität München, Munich, Germany
Institute for Diabetes and Obesity, Helmholtz Diabetes Center, Helmholtz Zentrum München, German Research Center for Environmental Health, Neuherberg, Germany German Center for Diabetes Research, Neuherberg, Germany Department of Chemistry, Indiana University, Bloomington, Indiana Division of Metabolic Diseases, Technische Universität München, Munich, Germany
Institute for Diabetes and Obesity, Helmholtz Diabetes Center, Helmholtz Zentrum München, German Research Center for Environmental Health, Neuherberg, Germany German Center for Diabetes Research, Neuherberg, Germany Department of Chemistry, Indiana University, Bloomington, Indiana Division of Metabolic Diseases, Technische Universität München, Munich, Germany
Components Of The Camp Signalling System
cAMP is generated from ATP by adenylyl cyclases , an enzyme family with 10 members many of which are expressed in islet cells, . All but 1 isoform is regulated by G-protein-coupled receptors that either mediate stimulation via Gs or suppression via Gi subunits. Some of these ACs are also activated or inhibited by Ca2+/calmodulin and phosphorylation by protein kinases. The Ca2+-stimulated isoforms AC1, AC3 and AC8,, as well as the Ca2+-insensitive AC9 have been found important in rodent -cells and insulinoma cells. Less is known about human -cells but the Ca2+- and protein kinase A -inhibited AC5 was recently found critical for glucose stimulation of insulin secretion. One AC, named soluble AC , has also been implicated in the regulation of insulin secretion. sAC is structurally distinct, insensitive to G-proteins and instead regulated by Ca2+, HCO3 and probably ATP, because it is the only AC with reported ATP affinity that matches cytoplasmic concentrations. The functional importance of specific AC isoforms in -cell function is yet poorly defined.
Don’t Miss: How Many Carbs Should A Diabetic Eat
Camp Effects On Metabolism
It has been observed that elevations of cAMP by GLP-1 and forskolin stimulate ATP production in mouse islets. In contrast, no effects on ATP production or oxygen consumption were observed in another study using conventional biochemical approaches. Whether cAMP influences metabolism thus remains controversial, and it is unclear how quantitatively important such an effect would be in relation to established actions on the more distal steps of the stimulus-secretion-coupling process.
How Does Glucagon Increase Gluconeogenesis
Glucagon opposes hepatic insulin action and enhances the rate of gluconeogenesis, increasing hepatic glucose output. In order to support gluconeogenesis, glucagon promotes skeletal muscle wasting to supply amino acids as gluconeogenic precursors.
What is the difference between glucose and insulin? Glucose comes from the Greek word for sweet. Its a type of sugar you get from foods you eat, and your body uses it for energy. As it travels through your bloodstream to your cells, its called blood glucose or blood sugar. Insulin is a hormone that
You May Like: Metformin 1500 Mg Side Effects
Pharmaceutical Use Of Glucagon In Human Patients
Glucagon is employed as both a diagnostic and therapeutic agent. Although historically used for the diagnosis of pheochromocytoma, stimulation of catecholamine secretion in such patients may be dangerous and hence the glucagon stimulation test is not recommended. Glucagon may also be employed as part of a diagnostic test in patients with hypoglycemia of unknown origin. The most common clinical application of glucagon therapeutically is in the adjunctive management of severe hypoglycemia. Diabetic patients with hypoglycemia generally respond quickly with a rapid increase in blood glucose to intranasal, intramuscular, or subcutaneous glucagon.157,158 Glucagon is also used to inhibit gastrointestinal motility during radiologic investigations, and several studies have reported the efficacy of glucagon administration in patients with bronchospasm, symptomatic bradycardia, or refractory hypotension.
Nori Geary, in, 2004
Beffects Of Gip And Glp
In contrast to GLP-1, GIP has been shown to stimulate pancreatic glucagon secretion from perfused rat and dog pancreata with maximal effects in the presence of low glucose. In rat islets, the stimulatory effect of GIP involved activation of protein kinase A . GIP-induced glucagon release may play a role in maintaining normoglycemia during high protein meals in these species. Most studies in humans have examined the effect of GIP on glucagon secretion at elevated glucose concentrations and found no effect in normal individuals . However, GIP exerted glucagonotropic actions in perfused pancreata from human cadavers and increased glucagon levels under fasting conditions . GIP may therefore play a physiological role in the regulation of -cell secretion in humans. Similar to GLP-1 , GIP also stimulates secretion of pancreatic SS and both incretin hormones may stimulate pancreatic polypeptide secretion in rodents, although the significance of these effects for humans is unclear.
Read Also: Are Bananas Okay For Type 2 Diabetes
Glucagon Mechanisms Of Action
Glucagon Biosynthesis and Secretion
Glucagon is produced and processed from preproglucagon in pancreatic cells, in small intestine L cells, and in certain hypothalamic cells . Preproglucagon consists of a signal peptide, glicitin-related polypeptide, glucagon, glucagon-like peptide-1 , and glucagon-like peptide-2 . Though several of these peptides other than glucagon have received increased attention in recent years, we will only discuss here the biosynthesis of glucagon. Glucagon itself is produced primarily by processing the preproglucagon to proglucagon and then by a series of specific enzymes to glucagon. This complete processing occurs only in the pancreatic cells . Higher molecular weight forms are released from the gut and can be found in circulation. It appears that only glucagon is released from the normally functioning cell of the pancreas.
In diabetes, hyperglucagonemia is often present despite the elevated levels of glucose. Current evidence suggests that the elevated levels of glucagon in diabetes are entirely due to the insulin deficiency, at least in the insulin-deficient form of diabetes, since bringing insulin levels to normal in insulin-deficient diabetes can completely reverse hyperglucagonemia.
Glucagon: Biomedical Mechanisms of Action
Figure 2. Cascade of reactions that leads to the formation of glucose.
Figure 3. Effects of CAMP on various enzymes involved in glycolysis and gluconeogenesis.
David O. Norris Ph.D., James A. Carr Ph.D., in, 2013
What Is The Difference Between Insulin And Glucose
Glucose comes from the Greek word for “sweet.” It’s a type of sugar you get from foods you eat, and your body uses it for energy. As it travels through your bloodstream to your cells, it’s called blood glucose or blood sugar. Insulin is a hormone that moves glucose from your blood into the cells for energy and storage.
You May Like: Metformin 500 Mg Used For
Molecular Structure Of Of Insulin:
Insulin is made of amino acids and consists of two chains named an A chain and a B chain, that are joined together by sulfur bonds. Insulin is produced from a proinsulin hormone that actually has three amino acid chains. An enzyme modifies the hormone in such a way that only the A and B chain remains to form insulin.

