Response To An Increase In Blood Glucose
In the absorptive state, an increase in blood glucose is detected by the beta cells of the pancreatic islets, causing them to increase the release of insulin into the blood. Insulin stimulates cells, especially adipose and muscle cells, to take up glucose from the blood.
Insulin and the transport of glucose into cells – To enter cells, glucose requires trans-membrane transporters and there is a family of these called GLUT . The most numerous is GLUT4, which is found on muscle and fat cells.
When insulin binds to insulin receptors on the cell membrane, cells are stimulated to increase the number of glucose transporters. The more transporters are produced, the more glucose is transported into cells – with a corresponding drop in blood glucose.
The precise mechanism whereby insulin binds to receptors causing translocation is still to be determined .
Not all tissues require insulin to take up glucose, for example brain and liver cells use GLUT transporters that are not dependent on insulin.
Further effects of insulin – The hormone also has other effects on the bodys cells, all of which contribute to an increase in glucose usage and storage – and therefore a reduction in blood glucose. These include:
– The promotion of glycolysis, a process that breaks down glucose for cellular energy
– The promotion of glycogenesis, a process that converts glucose into glycogen for storage
– The inhibition of lipolysis, a process that breaks down lipids to release energy.
The Insulin Secretion Signaling Pathway
Endocrine cells secrete their respective hormones in response to external signals, such as nutrient intake or stress, via humoral, neural or hormonal signaling pathways. The underlying molecular process that translates the stimulus into the actual hormone release is called stimulus-secretion coupling which is known as the stimulus-dependent exocytosis of a particular substance, such as glucose-stimulated -cell insulin release.
Glucose-stimulated insulin release from a pancreatic -cell. Exogenous glucose is taken up by GLUT2 and undergoes glycolysis inside the cell. Elevated adenosine triphosphate levels alter the ATP/ADP ratio, which in turn leads to the closure of ATP-sensitive K+-channels. The subsequent membrane depolarization opens voltage-dependent Ca2+-channels in response to increasing intracellular calcium levels, which eventually trigger insulin secretion following vesicle fusion with the membrane.
How Can Chemicals Affect The Endocrine System
Scientific research on human epidemiology, laboratory animals, and fish and wildlife suggests that environmental contaminants can disrupt the endocrine system leading to adverse-health consequences. It is important to gain a better understanding of what concentrations of chemicals found in the environment may cause an adverse effect. Various types of scientific studies are necessary to resolve many of the scientific questions and uncertainty surrounding the endocrine disruptor issue. Many such studies are currently underway by government agencies, industry, and academia.
Learn more with EDSP about concerns and examples of endocrine disruption.
Don’t Miss: Do Antibiotics Affect Blood Sugar
What Does The Pancreas Do
The pancreas carries out two important roles:
The pancreas produces hormones in its ‘endocrine’ cells. These cells are gathered in clusters known as islets of Langerhans and monitor what is happening in the blood. They then can release hormones directly into the blood when necessary. In particular, they sense when sugar levels in the blood rise, and as soon as this happens the cells produce hormones, particularly insulin. Insulin then helps the body to lower blood glucose levels and ‘store’ the sugar away in fat, muscle, liver and other body tissues where it can be used for energy when required.
The pancreas is very close to the stomach. As soon as food is eaten, the pancreas releases digestive enzymes into the bowel to break food down. As the food is digested, and nutrient levels in the blood rise, the pancreas produces insulin to help the body store the glucose away. Between meals, the pancreas does not produce insulin and this allows the body to gradually release stores of energy back into the blood as they are needed.
Response To A Decrease In Blood Glucose
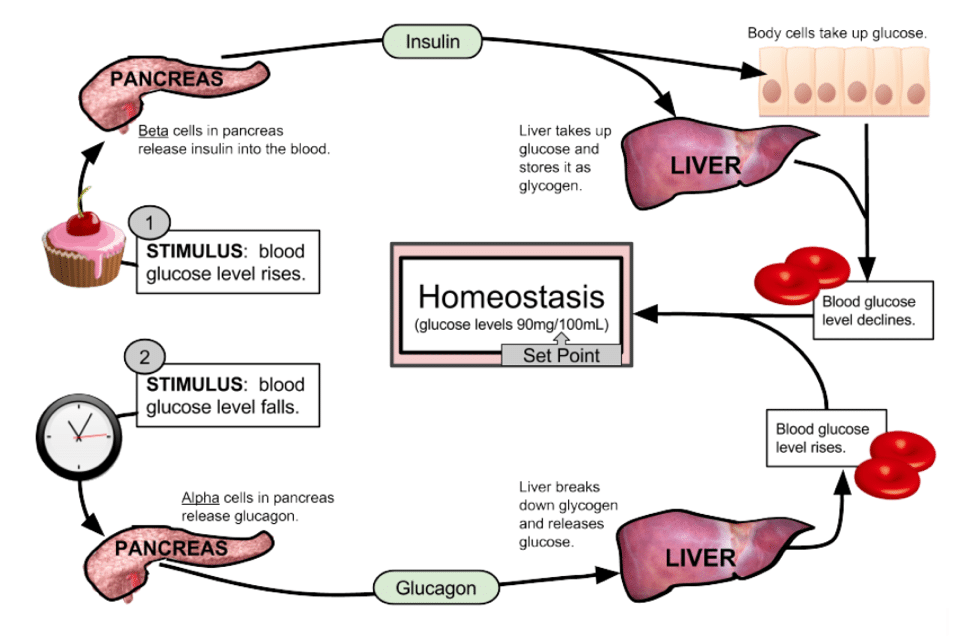
Several hours after eating a meal, when the body is in the post-absorptive state, insulin levels fall along with blood glucose and this results in the hormone glucagon being released by the alpha cells of the pancreas.
The role of glucagon – Glucagon has the opposite effect to insulin in that it increases blood-glucose levels and promotes processes that spare glucose utilisation.
Glucagon works primarily on the hepatocytes in the liver to:
– Convert stored glycogen into glucose and release it into the blood
– Promote gluconeogenesis, the manufacture of new glucose from lactic acid and other metabolites.
Glucagon binds to glucagon receptors, which are part of the G-protein-coupled receptor family. This stimulates a series of linked enzyme reactions, resulting in the activation of glycogen phosphorylase, the enzyme responsible for the mobilisation of glycogen reserves into free glucose. Glucagon release is inhibited by both insulin and somatostatin.
You May Like: 112 Sugar Level
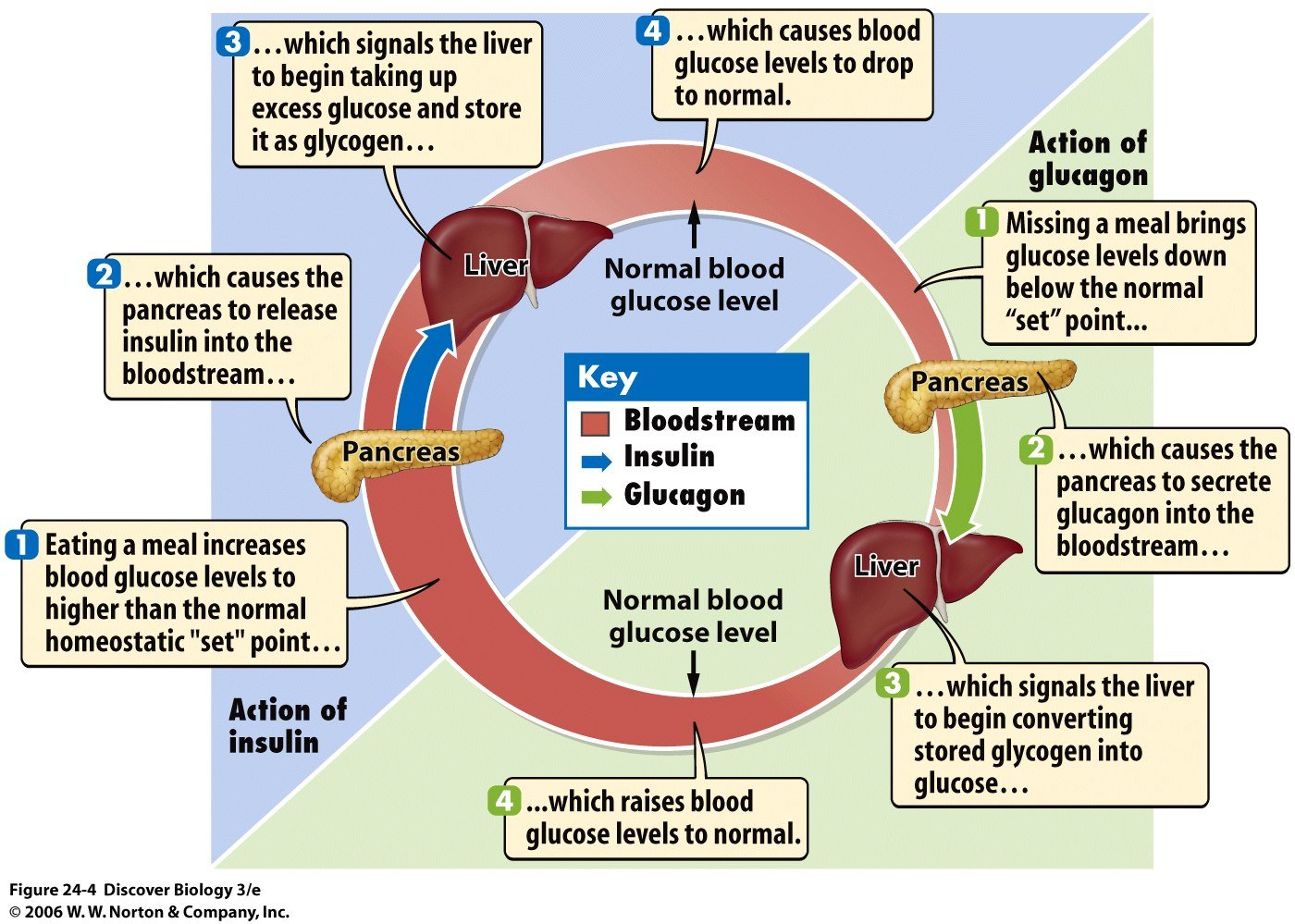
Regulation Of Blood Glucose Levels: Insulin And Glucagon
Cells of the body require nutrients in order to function. These nutrients are obtained through feeding. In order to manage nutrient intake, storing excess intake, and utilizing reserves when necessary, the body uses hormones to moderate energy stores. Insulin is produced by the beta cells of the pancreas, which are stimulated to release insulin as blood glucose levels rise . Insulin lowers blood glucose levels by enhancing the rate of glucose uptake and utilization by target cells, which use glucose for ATP production. It also stimulates the liver to convert glucose to glycogen, which is then stored by cells for later use. As insulin binds to its target cell via insulin receptors and signal transduction, it triggers the cell to incorporate glucose transport proteins into its membrane. This allows glucose to enter the cell, where it can be used as an energy source. These actions mediated by insulin cause blood glucose concentrations to fall, called a hypoglycemic, or âlow sugarâ effect, which inhibits further insulin release from beta cells through a negative feedback loop.
Diabetes mellitusThe regulation of blood glucose levels by insulin and glucagon
The Outlook For Women
As women get older, hormone changes before and during menopause often cause hot flashes, irritability, and trouble sleeping. Not only do these drops or spikes in the hormones impact your mood and life, but they can also affect your blood sugar. These ups and downs mean may mean you have to test your levels and make adjustments more often.
If you have type 1 diabetes, you may notice low blood sugar levels more often as you get closer to menopause. This can be a sign that your hormones are going down and you may need less insulin. Itâs important to know the difference between low blood sugar and moodiness or other perimenopause symptoms.
You may reach menopause early if you have type 1 diabetes, but if youâre overweight and have type 2, your changes could start later. Thatâs because estrogen doesnât drop as quickly in heavier women.
As your bodyâs changing, itâs easy to confuse signs of menopause with symptoms of high or low blood sugar. Dizziness, sweating, irritability, and trouble concentrating could all result from hormonal changes or from blood sugar thatâs too high or too low. The only way to know for sure — and the safest thing to do — is to test it. But checking too often can take an emotional toll. If youâre worried, your doctor or diabetes educator can help you figure out how often to do it.
If you canât get your blood sugar levels where they need to be, your doctor might suggest hormone replacement therapy .
Read Also: Diabetes In 20s
Understanding The Processes Behind The Regulation Of Blood Glucose
20 April, 2004
VOL: 100, ISSUE: 16, PAGE NO: 56
Pat James, PhD, is senior lecturer in applied physiology
Roger McFadden, MSc, is senior lecturer in applied physiology both at the School of Health and Policy Studies, The University of Central England in Birmingham
Pat James, PhD, is senior lecturer in applied physiology
Glucose is one of the bodys principal fuels. It is an energy-rich monosaccharide sugar that is broken down in our cells to produce adenosine triphosphate. ATP is a small packet of chemical energy that powers the millions of biochemical reactions that take place in the body every second.
We obtain glucose from the food that we eat, predominantly starch-rich foods such as potatoes, rice, bread, and pasta. Starch is a polysaccharide that is broken down by digestive enzymes into individual glucose molecules.
In the small intestine, glucose is absorbed into the blood and travels to the liver via the hepatic portal vein. The hepatocytes absorb much of the glucose and convert it into glycogen, an insoluble polymer of glucose.
This is stored in the liver and can be reconverted into glucose when blood-glucose levels fall. Other types of simple sugars in our diet such as fructose, sucrose and lactose are also fuels that contribute to the production of ATP.
If glucose levels fall to too low a concentration or rise too high then this situation can lead to the neurological processes in the brain being compromised.
What Happens If I Have Too Little Glucagon
Unusual cases of deficiency of glucagon secretion have been reported in babies. This results in severely low blood glucose which cannot be controlled without administering glucagon.
Glucagon can be given by injection to restore blood glucose lowered by insulin . It can increase glucose release from glycogen stores more than insulin can suppress it. The effect of glucagon is limited, so it is very important to eat a carbohydrate meal once the person has recovered enough to eat safely.
Read Also: Metformin And Antibiotics
The Pancreas Is An Exocrine And Endocrine Organ
Anatomical organization of the pancreas. The exocrine function of the pancreas is mediated by acinar cells that secrete digestive enzymes into the upper small intestine via the pancreatic duct. Its endocrine function involves the secretion of various hormones from different cell types within the pancreatic islets of Langerhans. The micrograph shows the pancreatic islets. LM × 760 . Adapted from Human Anatomy and Physiology, an OpenStax College resource.
Maintenance of blood glucose levels by glucagon and insulin. When blood glucose levels are low, the pancreas secretes glucagon, which increases endogenous blood glucose levels through glycogenolysis. After a meal, when exogenous blood glucose levels are high, insulin is released to trigger glucose uptake into insulin-dependent muscle and adipose tissues as well as to promote glycogenesis.
Hormones Of The Pancreas
Regulation of blood glucose is largely done through the endocrine hormones of the pancreas, a beautiful balance of hormones achieved through a negative feedback loop. The main hormones of the pancreas that affect blood glucose include insulin, glucagon, somatostatin, and amylin.
Insulin lowers BG levels, whereas glucagon elevates BG levels.
Somatostatin is formed in the delta cells of the pancreas and acts as the pancreatic policeman, balancing insulin and glucagon. It helps the pancreas alternate in turning on or turning off each opposing hormone.
Amylin is a hormone, made in a 1:100 ratio with insulin, that helps increase satiety, or satisfaction and state of fullness from a meal, to prevent overeating. It also helps slow the stomach contents from emptying too quickly, to avoid a quick spike in BG levels.
In a healthy liver, up to 10% of its total volume is used for glycogen stores. Skeletal muscle cells store about 1% of glycogen. The liver converts glycogen back to glucose when it is needed for energy and regulates the amount of glucose circulating between meals. Your liver is amazing in that it knows how much to store and keep, or break down and release, to maintain ideal plasma glucose levels. Imitation of this process is the goal of insulin therapy when glucose levels are managed externally. Basalbolus dosing is used as clinicians attempt to replicate this normal cycle.
Test Your Knowledge
Apply Your Knowledge
Online Resource
Don’t Miss: Blood Sugar Level Symptoms
How To Stay Healthy In Midlife
As it turns out, the things you do to get a handle on diabetes as you enter midlife arenât that different than what youâve been doing all along to stay healthy:
- Pay attention to your diabetes. That means you need to keep track of your blood sugar levels and talk to your doctor if theyâre are all over the place and you canât figure out why. Keep a record of your results and go over them with your doctor.
- Watch your weight.
- Eat a healthy diet. Get plenty of vegetables, choose whole-grain foods, and opt for lean proteins and low-fat dairy.
- Get at least 30 minutes of exercise a day. It will give you more energy and boost your mood. Youâll get the most benefit by doing a combination of an exercise that ups your heart rate — like brisk walking — along with strength training, like lifting weights.
Understanding Insulin And Diabetes
- The pancreas maintains the bodys blood glucose balance.
- Primary hormones of the pancreas include insulin and glucagon, and both regulate blood glucose.
- Diabetes is the most common disorder associated with the pancreas.
Anatomy of the Pancreasspineislets of LangerhansHormones of the Pancreas
- Gastrin: This hormone aids digestion by stimulating certain cells in the stomach to produce acid.
- Glucagon: Glucagon helps insulin maintain normal blood glucose by working in the opposite way of insulin. It stimulates your cells to release glucose, and this raises your blood glucose levels.
- Insulin: This hormone regulates blood glucose by allowing many of your bodys cells to absorb and use glucose. In turn, this drops blood glucose levels.
- Somatostatin: When levels of other pancreatic hormones, such as insulin and glucagon, get too high, somatostatin is secreted to maintain a balance of glucose and/or salt in the blood.
- Vasoactive intestinal peptide : This hormone helps control water secretion and absorption from the intestines by stimulating the intestinal cells to release water and salts into the intestines.
Diseases and Disorders of the Pancreas
Recommended Reading: Rye Bread Good For Diabetes
The Pancreas And Insulin
The pancreas is responsible for producing insulin. The cells which produce insulin are beta cells. These cells are distributed in a cluster of cells in the pancreas called the Islets of Langerhans, named after the anatomist who discovered them
Insulin is a hormone that helps to regulate blood sugar levels by assisting the transport of glucose from the blood into neighbouring cells.
New Approaches To Drug Development And Therapies With A Particular Focus On Drug Development By Green Synthesis To Cure Blood Glucose Regulation Problems
Bioactive molecules from Natural products have been proved to improve insulin resistance and its associated complications by suppressing inflammatory signaling pathways . Medicinal plants cannot be obsolete and still play a prominent role in human health care. Among natural sources, over 1200 plants have been claimed as antidiabetic remedies. While over 400 plants along with its 700 recipes and compounds have been scientifically evaluated for type-II diabetes. Metformin was developed on the basis of biguanide compound from an antidiabetic herb, French lilac and is now its a first-line drug against type-II diabetes. Medicinal plants also contains a diverse bioactive compounds and can have multiple actions on insulin action, insulin production, or both. With a focus on scientific studies of selected glucose-lowering herbs, phyto compounds and their ability to target insulin resistance, cell function, incretin related pathways and glucose absorption , multiple studies have been done.
Figure 6.
Mechanisms underlying herbal therapies using antidiabetic plants and phytocompounds. Different types of medicinal herbs can be classified based on their modes of action such as insulin resistance , -cell function , and GLP-1 and glucose absorption , The selected.
Recommended Reading: What Are Side Effects Of Metformin 500 Mg
References And Recommended Reading
Ahrén, B. Islet G protein-coupled receptors as potential targets for treatment of type 2 diabetes. Nature Reviews Drug Discovery8, 369385 . doi:10.1038/nrd2782.
Kebede, M. A., Alquier, T., et al. Lipid receptors and islet function: therapeutic implications? Diabetes, Obesity and Metabolism11, 1020 . doi: 10.1111/j.1463-1326.2009.01114.x.
Kim, H., Toyofuku, Y., et al. Serotonin regulates pancreatic beta cell mass during pregnancy. Nature Medicine16, 804808 . doi:10.1038/nm.2173.
Langenberg, C., Pascoe, L., et al. Common genetic variation in the melatonin receptor 1B gene is associated with decreased early-phase insulin response. Diabetologia52, 15371542 . doi: 10.1007/s00125-009-1392-x.
Regard, J. B., Kataoka, H., et al. Probing cell type-specific functions of G in vivo identifies GPCR regulators of insulin secretion. Journal of Clinical Investigation117, 40344043 . doi:10.1172/JCI32994.
Rosengren, A. H., Jokubka, R., et al. Overexpression of alpha2A-adrenergic receptors contributes to type 2 diabetes. Science327, 217220 . doi: 10.1126/science.1176827.
Winzell, M. S. & Ahren, B. G-protein-coupled receptors and islet function-implications for treatment of type 2 diabetes. Pharmacology and Theraputics116, 437448 . doi:10.1016/j.pharmthera.2007.08.002.
Ideal Blood Sugar Levels
A range of factors, including insulin resistance, diabetes, and an unbalanced diet, can cause blood sugar levels to spike or plummet.
The standard measurement units for blood sugar levels are milligrams per deciliter . Ideal blood sugar ranges are as follows:
| Timing |
Insulin and glucagon do not take immediate effect, particularly in people whose blood sugar levels are extremely high or low.
Don’t Miss: Can You Get A Tattoo If Your Diabetic
The Exocrine Cells Of The Pancreas
The exocrine cells produce digestive juices about 1.5 to 2 liters per day. They are called exocrine because the digestive juices that they produce flow out into the small intestine rather than directly into the bloodstream. This clear, colorless fluid is mainly made up of water and also contains salt, sodium bicarbonate and digestive enzymes. There are three main types of enzymes:
- Lipases to break down fats
- Proteases to break down proteins
- Amylases to break down carbohydrates
The digestive juices that are made in the pancreas flow into the small intestine through a tube known as the pancreatic duct. In most people, this duct is joined by a similar duct coming from the gallbladder before it reaches the small intestine. There is a circular muscle at the shared opening of the two ducts. This muscle controls the release of the digestive juices into the small intestine.
The digestive juices usually only start working once they enter the small intestine. But if the pancreas is inflamed , they already become active in the pancreas. As a result, the pancreas starts digesting itself.
Pancreas and surrounding organs

