Sleep And Sleep Deprivation
Acute sleep deprivation in healthy young adults has been reported to raise fasting blood glucose concentrations in association with altered diurnal cortisol secretion and reduced heart rate variability. These effects suggest increased counter-regulatory hormone secretion via hyper-arousal with activation of the hypothalamo-pituitary adrenal axis. There is also accumulating evidence that chronic sleep deprivation may impact on insulin and insulin resistance. Recent epidemiological studies report that reduced sleep duration is associated with increased BMI. Sleep deprivation is associated with decreased plasma concentrations of leptin, the adipocyte peptide hormone regulating fat mass and appetite, and increased concentrations of ghrelin, which increases appetite. Growth hormone is secreted during slow wave sleep, sleep declines with age and growth hormone deficiency in adults has been associated with central adiposity and insulin resistance, but whether sleep deprivation acts through these mechanisms is not clearly established. Obstructive sleep apnoea , where sleep disturbance results from obstruction to breathing during sleep, is associated with impaired glucose tolerance independent of adiposity, and improves with continuous positive airway pressure treatment but whether this is due to resolution of hypoxia and hypercapnia, or to effects on sleep quality, is unclear.
Pancreas: An Exocrine And Endocrine Organ
2.1.1 Location
It is located at the back of stomach, within left upper abdominal cavity.
2.1.2 Parts
Its parts are head, body and tail. Majority of this secretory organ consists of:
Acinar/exocrine cells : Which secrete pancreatic juice into main and accessory pancreatic duct.
Endocrine cells : Which secrete pancreatic hormones directly in blood stream . These cells cluster together and form the so-called islets of Langerhans . These are five different types of cells and release various hormones :
Glucagon-producing -cells: They are 1520% of the total islet cells and releases Glucagon to increase blood glucose levels.
Amylin-, C-peptide- and insulin-producing -cells: They are 6580% of the total cells and produces insulin to decrease glucose.
Pancreatic polypeptide -producing -cells: 35% of the total islet cells, to regulate the exocrine and endocrine secretion activity of the pancreas, is made of them.
Somatostatin-producing -cells: Constitute 310% of the total cells and releases Somatostatin which inhibits both, glucagon and insulin release.
Ghrelin-producing -cells: Comprise < 1% of the total islet cells.
Figure 1.
Genes To Regulate Blood Glucose Levels
Genetics is identifying a whole new set of genes, proteins and pathways that are related to diabetes and blood sugar control. Till now, scientist have identified a genetic disorder in MafA . Surprisingly, this genetic defect was present in an unrelated family along with diabetic and insulinoma family members. The link of this gene with a defect was detected for the first time and a stable resultant mutant protein was found with a longer life in the cell, and found to be significantly more abundant in -cells than its normal version .
Gene on chromosome-2 is linked with fasting glucose levels and is primarily expressed in pancreatic -cells to convert glucose-6-phosphate back to glucose. Its genetic variation may be responsible for reduction in insulin secretion that increases glucose concentration. Chronically elevated levels of glucose may be a precursor for type 2 diabetes .
13 new genetic variants has been discovered by an international research consortium and these variants can manipulate blood glucose regulation, insulin resistance and function of insulin-secreting -cells in European descent populations, in which 05 of the following newly discovered variants raised the risk of developing type 2 diabetes:
SNPs in the region of ADCY5 which influence fasting and postprandial glucose levels.
FADS1 which is linked with fasting glucose as well as lipid traits.
Only one variant, near IGF1 which is associated with insulin resistance
Don’t Miss: Can A Diabetic Eat Cheese
Functional Measures Of Insulin Resistance
Another approach is to identify insulin resistant patients, based on functional markers of insulin resistance. McLoughlin et al were able to identify insulin resistant individuals from an overweight-obese cohort by looking at plasma triglyceride concentration, ratio of triglyceride to high-density lipoprotein cholesterol concentrations and insulin concentration. Using cut points of 1.47 mmol/L for triglyceride, 1.8 mmol/L for the triglyceride-high-density lipoprotein cholesterol ratio and 109 pmol/L for insulin, they achieved comparable sensitivity and specificity to the Adult Treatment Panel III to diagnose the metabolic syndrome.
Insulin And Fat Storage
As well as being involved in the regulation of blood glucose, insulin is also involved in how fat is used by the body. When the liver is has taken up its capacity of glycoge, insulin signals fat cells to take up glucose to be stored as triglycerides.
An additional effect of insulin is in inhibiting the breakdown of fats.
You May Like: What Happens When You Have Type 1 Diabetes
Does Ozempic Cause Bloating As A Side Effect
Yes, Ozempic may cause bloating as a side effect.
In very rare cases, Ozempic causes pancreatitis . It can be either short-term or long-term. If you ever had pancreatitis or other pancreatitis problem, you must inform the physician before starting the treatment. Pancreatitis may cause the following symptoms:
- Fever
- Vomiting
- Abdominal pain
If you have any of the above symptoms, inform your doctor immediately. If the doctor confirms that you have pancreatitis, they will stop your treatment with Ozempic and manage the condition.
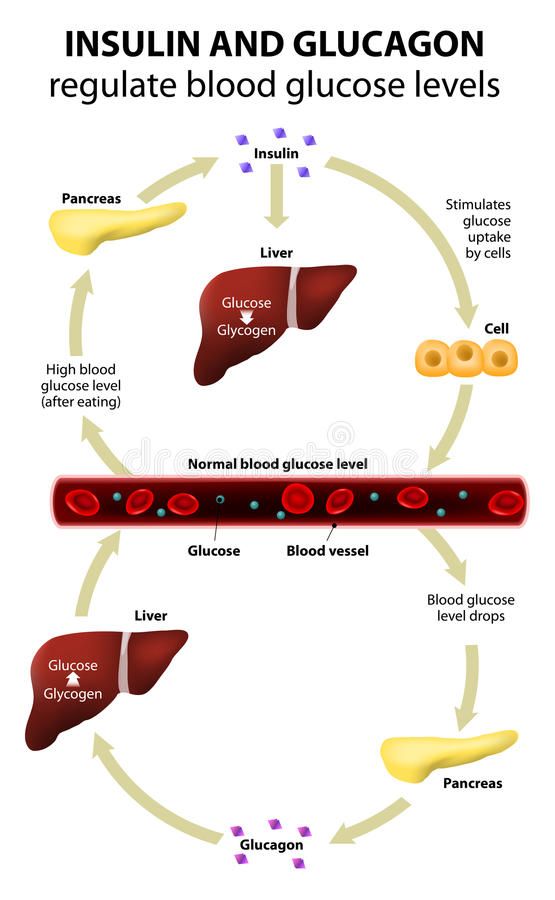
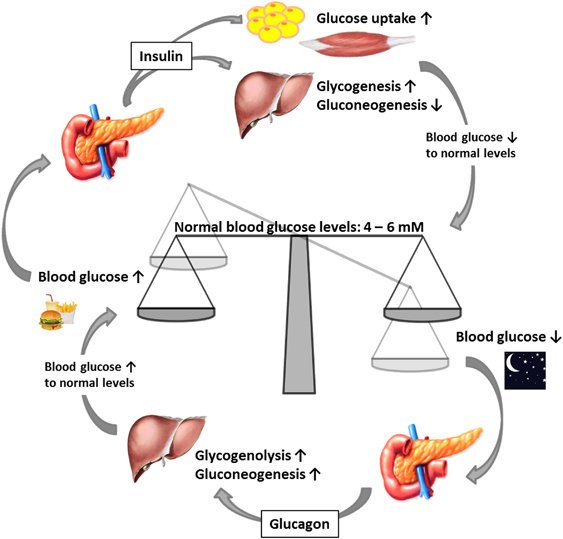
How Do Insulin And Glucagon Regulate Blood Glucose Levels
Insulin and glucagon work to help keep your blood glucose level under control. Both of these hormones are produced in the pancreas. Insulin, which helps to normalize a high level of blood sugar, is produced by the beta cells. On the other hand, glucagon, which helps to control a low level of blood sugar, is produced by the alpha cells.
You May Like: What Kind Of Candy Can A Diabetic Eat
Antagonistic Glucagon Peptide Analogs
Extensive efforts have been made to generate linear and cyclic peptide glucagon analogs. Compared with the wild-type glucagon, some of these peptide analogs have been shown to have distinct properties in terms of their ability to bind to the glucagon receptor and affect glucagon-stimulated cAMP production. They act as pure agonists, partial agonists/antagonists, or pure antagonists of the glucagon receptor . It was first reported that -glucagon, a potent antagonistic glucagon analog, significantly decreased hyperglycemia in streptozotocin-induced diabetic rats in vivo . -glucagon amide, another potent antagonistic glucagon analog, was also found to completely block exogenous glucagon-induced hyperglycemia in normal rabbits and to block hyperglycemia due to endogenous glucagon in streptozotocin-induced diabetic rats . Finally, similar glucose-lowering effects have been reported for another antagonistic glucagon analog, -glucagon-NH2 . It is therefore possible that such antagonistic peptide glucagon analogs may also have therapeutic potentials.
You May Like: Non Diabetic A1c Levels
How Is Glucagon Controlled
Glucagon works along with the hormone insulin to control blood sugar levels and keep them within set levels. Glucagon is released to stop blood sugar levels dropping too low , while insulin is released to stop blood sugar levels rising too high .
The release of glucagon is stimulated by low blood glucose, protein-rich meals and adrenaline . The release of glucagon is prevented by raised blood glucose and carbohydrate in meals, detected by cells in the pancreas.
In the longer-term, glucagon is crucial to the bodys response to lack of food. For example, it encourages the use of stored fat for energy in order to preserve the limited supply of glucose.
Recommended Reading: Skinny Diabetics
You May Like: What Is A Normal A1c For A Non Diabetic
Regulating Blood Sugar Levels
So as you can see, the body has several different hormones involved in the regulation of blood glucose. Even if you arent eating glucose per se, the body breaks down carbohydrates to obtain that energy source. Insulin is probably the more well known hormone in this process, but the pancreas and liver have other pathways they can use to maintain the necessary levels and prevent damage.
Effects Of Insulin And Glucagon On Blood Sugar Levels
Normal levels of blood sugar are between 70mg/dL and 110mg/dL. When your blood sugar level falls below 70mg/ dL, your body will signal the pancreas to release glucagon. When blood glucose levels rises above 110mg/dL insulin will be released. If insulin and glucagon are not functioning properly, this can lead to health conditions such as diabetes.
Don’t Miss: Bananas Raise Blood Sugar
Ideal Blood Sugar Levels
A range of factors, including insulin resistance, diabetes, and an unbalanced diet, can cause blood sugar levels to spike or plummet.
The standard measurement units for blood sugar levels are milligrams per deciliter . Ideal blood sugar ranges are as follows:
| Timing |
Insulin and glucagon do not take immediate effect, particularly in people whose blood sugar levels are extremely high or low.
What Are The Most Common Side Effects Of Ozempic & How To Manage Them
Ozempic is a prescription medication used to control blood sugar levels in adults with type 2 diabetes . Ozempic is usually prescribed with a diet and exercise program to control blood sugar levels in adults.
Like all other medications Ozempic may cause mild or severe side effects. You may experience some of them, and they will disappear using the drug.
Keep reading the article to understand what side effects Ozempic causes and how you can manage the side effects of the drug.
Ozempic injection may cause other side effects. Call your doctor if your symptoms are severe or persistent while using Ozempic.
You May Like: Side Effects Of Bad Insulin
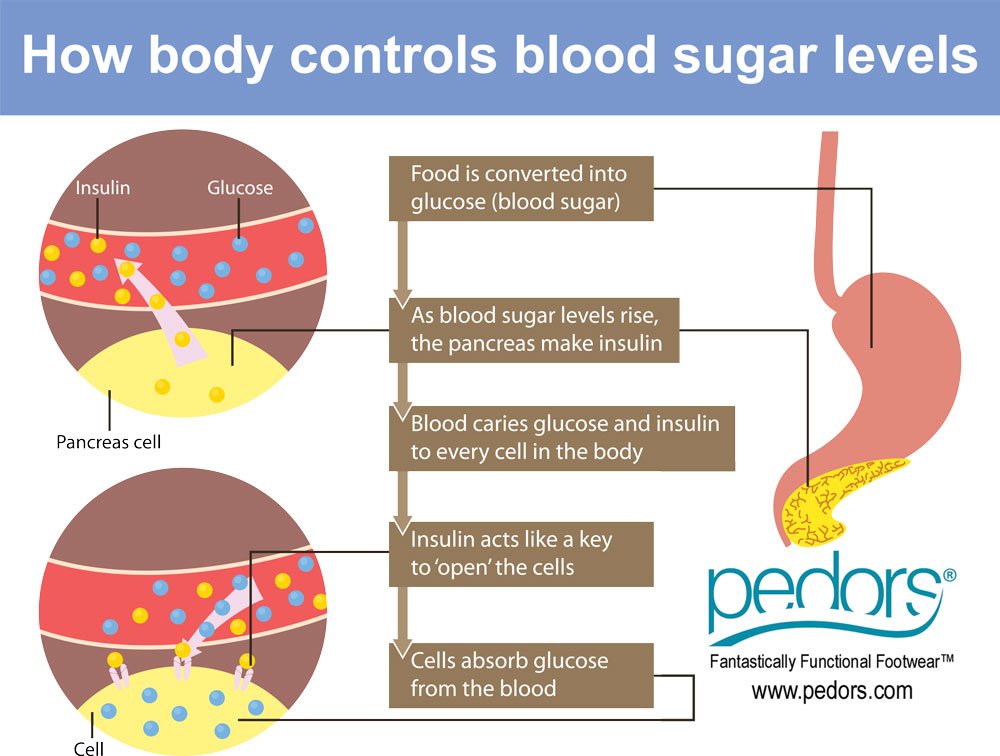
Insulin And Energy Usage
Blood sugar levels usually increase after eating, with levels reaching 180 mg/dL according to the American Diabetes Association. When receptors in the pancreas sense increases in blood glucose levels, the pancreas releases insulin. Insulin is a hormone that aids in the removal of glucose from the blood in a variety of ways: it promotes the entry of glucose into cells, enhances the storage of glycogen or fatty acids, and prevents the usage of fats and protein as energy. Fats and protein somewhat compete with glucose as sources of energy in the body.
Optimal Regulation Of Blood Glucose Level In Type I Diabetes Using Insulin And Glucagon
-
Roles Methodology, Writing original draft
Affiliation Mechanical Engineering Department, University of New Mexico, Albuquerque, NM 87131, United States of America
-
Roles Methodology, Writing original draft
Affiliation Mechanical Engineering Department, University of New Mexico, Albuquerque, NM 87131, United States of America
-
Affiliation Mechanical Engineering Department, University of New Mexico, Albuquerque, NM 87131, United States of America
-
Roles Methodology, Writing original draft
Affiliation Mechanical Engineering Department, University of New Mexico, Albuquerque, NM 87131, United States of America
Recommended Reading: What Kind Of Rice Can Diabetics Eat
Insulin And Type 1 Diabetes
In type 1 diabetes, the body produces insufficient insulin to regulate blood glucose levels.
Without the presence of insulin, many of the bodys cells cannot take glucose from the blood and therefore the body uses other sources of energy.
Ketones are produced by the liver as an alternative source of energy, however, high levels of the ketones can lead to a dangerous condition called ketoacidosis.
People with type 1 diabetes will need to inject insulin to compensate for their bodys lack of insulin.
Cells And Secretions Of The Pancreatic Islets
The pancreatic islets each contain four varieties of cells:
- The alpha cell produces the hormone glucagon and makes up approximately 20 percent of each islet. Glucagon plays an important role in blood glucose regulation low blood glucose levels stimulate its release.
- The beta cell produces the hormone insulin and makes up approximately 75 percent of each islet. Elevated blood glucose levels stimulate the release of insulin.
- The delta cell accounts for four percent of the islet cells and secretes the peptide hormone somatostatin. Recall that somatostatin is also released by the hypothalamus , and the stomach and intestines also secrete it. An inhibiting hormone, pancreatic somatostatin inhibits the release of both glucagon and insulin.
- The PP cell accounts for about one percent of islet cells and secretes the pancreatic polypeptide hormone. It is thought to play a role in appetite, as well as in the regulation of pancreatic exocrine and endocrine secretions. Pancreatic polypeptide released following a meal may reduce further food consumption however, it is also released in response to fasting.
Recommended Reading: Diabetes And The Digestive System
Also Check: How Many Carbs A Day For Diabetics
Physiological Role Of Insulin
Insulin is the pivotal hormone regulating cellular energy supply and macronutrient balance, directing anabolic processes of the fed state. Insulin is essential for the intra-cellular transport of glucose into insulin-dependent tissues such as muscle and adipose tissue. Signalling abundance of exogenous energy, adipose tissue fat breakdown is suppressed and its synthesis promoted. In muscle cells, glucose entry enables glycogen to be synthesised and stored, and for carbohydrates, rather than fatty acids to be utilised as the immediately available energy source for muscle contraction. Insulin therefore promotes glycogen and lipid synthesis in muscle cells, while suppressing lipolysis and gluconeogenesis from muscle amino acids. In the presence of an adequate supply of amino acids, insulin is anabolic in muscle.
The Basics Of High Blood Sugar
Diabetes is a problem with your body that causes blood sugar levels to rise higher than normal. This is also called hyperglycemia.
When you eat, your body breaks food down into sugar and sends it into the blood. Insulin then helps move the sugar from the blood into your cells. When sugar enters your cells, it is either used as fuel for energy right away or stored for later use. In a person with diabetes, there is a problem with insulin. But, not everyone with diabetes has the same problem.
There are different types of diabetestype 1, type 2 and gestational diabetes. If you have diabetestype 1, type 2 or gestationalyour body either doesn’t make enough insulin, can’t use the insulin well, or both.
Learn more about blood sugar Learn more about insulin
Also Check: What Is A Normal A1c For A Non Diabetic
Response To An Increase In Blood Glucose
In the absorptive state, an increase in blood glucose is detected by the beta cells of the pancreatic islets, causing them to increase the release of insulin into the blood. Insulin stimulates cells, especially adipose and muscle cells, to take up glucose from the blood.
Insulin and the transport of glucose into cells – To enter cells, glucose requires trans-membrane transporters and there is a family of these called GLUT . The most numerous is GLUT4, which is found on muscle and fat cells.
When insulin binds to insulin receptors on the cell membrane, cells are stimulated to increase the number of glucose transporters. The more transporters are produced, the more glucose is transported into cells – with a corresponding drop in blood glucose.
The precise mechanism whereby insulin binds to receptors causing translocation is still to be determined .
Not all tissues require insulin to take up glucose, for example brain and liver cells use GLUT transporters that are not dependent on insulin.
Further effects of insulin – The hormone also has other effects on the bodys cells, all of which contribute to an increase in glucose usage and storage – and therefore a reduction in blood glucose. These include:
– The promotion of glycolysis, a process that breaks down glucose for cellular energy
– The promotion of glycogenesis, a process that converts glucose into glycogen for storage
– The inhibition of lipolysis, a process that breaks down lipids to release energy.
How Insulin Treatment Helps Your Blood Sugar
Insulin treatment works in much the same way as natural insulin that the pancreas makes. After you eat, your body breaks down carbohydrates into glucose. That glucose goes into your bloodstream and causes your blood sugar level to rise.
When you take insulin, it helps to move glucose out of your bloodstream and into cells. Your cells use some of that sugar for energy and then store any leftover sugar in your fat, muscles, and liver for later.
Once the sugar moves into your cells, your blood glucose level should go back to normal.
You May Like: What Is A High Blood Sugar Reading
Insulin Basics: How Insulin Helps Control Blood Glucose Levels
Insulin and glucagon are hormones secreted by islet cells within the pancreas. They are both secreted in response to blood sugar levels, but in opposite fashion!
Insulin is normally secreted by the beta cells of the pancreas. The stimulus for insulin secretion is a HIGH blood glucose…it’s as simple as that! Although there is always a low level of insulin secreted by the pancreas, the amount secreted into the blood increases as the blood glucose rises. Similarly, as blood glucose falls, the amount of insulin secreted by the pancreatic islets goes down.
As can be seen in the picture, insulin has an effect on a number of cells, including muscle, red blood cells, and fat cells. In response to insulin, these cells absorb glucose out of the blood, having the net effect of lowering the high blood glucose levels into the normal range.
Glucagon is secreted by the alpha cells of the pancreatic islets in much the same manner as insulin…except in the opposite direction. If blood glucose is high, then no glucagon is secreted.
When blood glucose goes LOW, however, more and more glucagon is secreted. Like insulin, glucagon has an effect on many cells of the body, but most notably the liver.
Control Of Blood Glucose Concentration By Pancreas And Insulin
Glucose is needed by cells for respiration. It is important that the concentration of glucose in the blood is maintained at a constant level and controlled carefully. Insulin is a hormone – produced by the pancreas – that regulates glucose concentrations in the blood.
If the blood glucose concentration is too high, the pancreas produces the hormone insulin that causes glucose to move from the blood into the cells. In liver and muscle cells excess glucose is converted to glycogen for storage, and will be used at a later date.
Read Also: What Is My A1c Supposed To Be

