Joe Biden Has Raised The Price Of Insulin
United States
An order brought in under Trump, the 34B insulin pass, has been delayed but it has not been reversed.
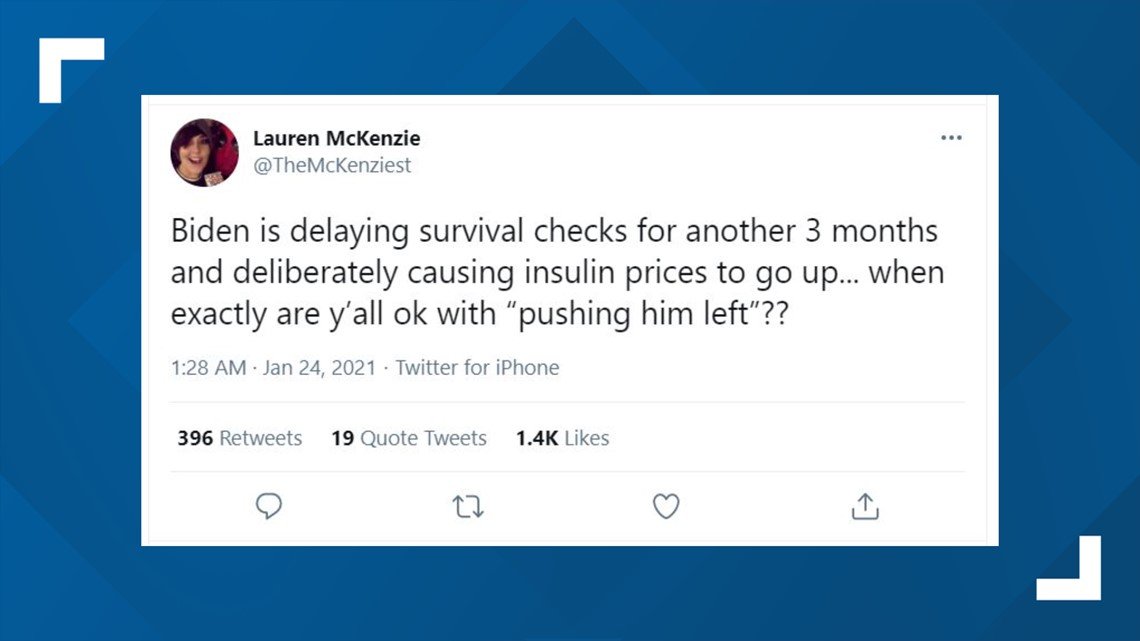
There are several claims on social media stating that President Joe Biden is reversing an executive order brought in under the Trump administration to reduce the cost of insulin.
According to USA Today, the Trump administration signed an order in 2020 after congress had pressured pharmaceutical companies to bring insulin costs under control. One of these rules requires federal health centers to pass on any savings they had made from discounted drug prices onto patients who may not be able to access healthcare. This rule disallows healthcare centers from receiving funds if prices for EpiPens and autoinjectors are too high. This rule was due to be implemented on January 22.
However, the Biden administration brought a regulatory rule freeze affecting all federal agency rules that had not gone into effect as of January 20, 2021. According to National Law Review, “At its core, the regulatory rule freeze requires all pending final rules to be delayed at least 60 days in order for the Biden administration to review and opine on the necessity and scope of affected rules.” This included Trump’s order on access to EpiPens.
Reference links
‘seems Like A Scam’: Biden’s Insulin Plan Sparks Backlash
It just seems like a big scam for the private insurance companies. Our lives are being used for propaganda. Wording is very important.
Story at a glance
- President Biden included an insulin price cap within his Build Back Better Act, which passed the House back in November 2021.
- For those enrolled in Medicare and with private group or individual health insurance plans, the price of insulin would be capped at $35.
- Yet in 2020, about 28 million people in the U.S. did not have health insurance, which means the insulin price cap would not apply to them.
President Biden has attempted to control the skyrocketing costs associated with having diabetes by capping the amount drug companies can charge for insulin, but there are glaring loopholes in the plan that many Americans are criticizing.
In this April 18, 2017 file photo, a woman with Type 2 diabetes prepares to inject herself with insulin at her home in Las Vegas. John Locher/ AP
In November of last year, the House passed Bidens Build Back Better Act , which included provisions that would limit the cost of insulin to $35, but only for those under Medicare or for those with private group or individual health insurance plans.
The price capping is expected to lower out-of-pocket costs for insulin users, with GoodRx Health estimating the average price per dispenser or vial of insulin ranges from $63 to $363, prices varying by brand and dosage.
READ MORE STORIES FROM CHANGING AMERICA
Committee Found Companies Raised Prices To Balance Out Rebates
To balance out rising rebates, insulin manufacturers in turn “aggressively” raised the list price of their insulin, the committee found.
“The investigation found that Novo Nordisk and Sanofi not only closely monitored the others’ price increases, they actually increased prices in lockstep sometimes within hours or days of each other a practice known as ‘shadow pricing,'” said the committee.
Internal emails also show that in 2014 Lilly executives decided to enact a list price increase for Humalog earlier than expected when the company heard Novo Nordisk had decided to increase list prices for its and Levemir products.
The committee documented list price increases of 50%-70% for insulins, sometimes over just a 3-year period.
The investigation also found after reviewing internal documents that drug makers often set prices based on whether it might harm a PBM’s or health plan’s bottom line. The goal was to keep those clients happy and to preserve market share, said the committee.
PBMs did not do anything to discourage the increases in list prices, said the committee. Instead, “PBMs used their size and aggressive negotiating tactics, like the threat of excluding drugs from formularies, to extract more generous rebates, discounts, and fees from insulin manufacturers.”
The PBM industry’s lobbying group, the Pharmacy Management Care Association , said it shared the committee’s “urgency in addressing affordability and access for insulin-dependent patients,” in a statement.
Don’t Miss: What Is Side Effects Of Metformin
Seems Like A Scam: Americans With Diabetes Criticize Bidens Insulin Proposal
Insurance cap includes loopholes and doesnt impact individuals who dont have health coverage in the US
Samia Chowdhury of Ontario, California, saw her work hours in the restaurant industry dwindle from full-time to less than 10 hours a week when Covid shutdowns began in the US in March 2020.
But the loss of work was not her only problem. As a someone who has had type 1 diabetes since she was 12, Chowdhury could not afford health insurance after losing most of her work hours and couldnt get on Medicaid through California. Instead, she relied on visiting medical clinics for insulin prescription refills when she could afford to do so and mutual aid from other people with diabetes around the US.
I could barely scrape together the $35 for the visit, said Chowdhury. I could not make ends meet. I was essentially choosing either a roof over my head or my health insurance.
She relied on the clinics for doctor visits, lab work, and had to ration insulin and supplies while struggling to make ends meet with rent and other bills.
Because I have to take the quick-acting insulin more often when I eat, that would be the only prescription I would pick up. The only way I can describe the effects on someones body is it feels like your whole body is acidic, but at least youre getting to tomorrow, she added. I was making a vial last for up to two months.
Its the most expensive chronic disease in the US.
Insulin Bill Would Help Diabetic Patients By Lowering Out
UNITED STATES – MARCH 31: House Majority Whip Jim Clyburn, D-S.C., participates in a news conference … outside the Capitol on the on the Affordable Insulin Now Act vote in the House of Representatives on Thursday, March 31, 2022.
The House of Representatives has passed a bill that would limit the out-of-pocket cost of insulin to $35 per month for Americans with health insurance. But, the legislation would not bring list prices down. Contrary to what many in the media say, as well as several top Democrats who support the bill, this legislation is not an insulin price control bill. Also, conspicuously, the bill does nothing for the uninsured. Two-thirds of the uninsured pay the highest possible price for insulin, which is the retail list price.
Moreover, pharmacy benefit managers and insurers may increase premiums, as an offset in response to having to cover more of the cost of insulin. In turn, on balance, this shifting of cost could undercut savings to diabetic patients.
The bill now moves to the Senate, where it would need some Republican support to pass. It will likely be debated in the Senate later this month.
If the bill is enacted, about 20% of Americans who have large employer coverage and are taking insulin would save money, the Kaiser Family Foundation has calculated.
The insulin bill doesnt include any guard-rails to avert premium increases, which implies cost shifting is likely, however suspect the reasoning by PBMs and insurers.
Recommended Reading: Most Common Side Effect Of Metformin
$35 Insulin Price Cap Endorsed By President Biden In State Of The Union Address
US pharmaceutical companies and insulin manufacturers react to proposed legislation that would cap insulin costs and prevent significant rises in the costs of prescription drugs.
In his State of the Union address on March 1, President Biden advocated for a $35 price cap on the cost of insulin. If passed, this legislation would limit the out-of-pocket cost of insulin to $35 per month, helping make insulin more affordable and accessible to all people with diabetes who need it.
The presidents call for a limit on out-of-pocket insulin costs comes from his support of a bill introduced to congress by Senator Reverend Raphael Warnock . This bill, the Affordable Insulin Now Act, would cap insulin costs for insulin dependent Americans who are insured, including those on Medicare.
The high cost of insulin, which can potentially be over $1,300 per month for those without insurance, has had a drastic impact on the health of people with diabetes. Research suggests that over 1 in 4 Americans with type 1 diabetes have had to ration their insulin because they could not afford the cost of the drug each month. Rationing insulin can be extremely dangerous, causing higher blood glucose levels and increasing the risk of death due to diabetic ketoacidosis .
Drug pricing and the American healthcare system are complex, with multiple factors contributing to the costs that individuals with diabetes pay for their insulin and other drugs.
Heres more information on how to get insulin at lower cost:
State Of The Union 2022
During his State of the Union address on March 1, 2022, President Biden specifically called out insulin pricing as a must-do policy change. With his down-to-earth charm, the president welcomed 13-year-old Joshua Davis who lives with T1D, and whod attended the address as a guest of First Lady Dr. Jill Biden. Davis is a young advocate whod previously attended JDRF Childrens Congress, talking with Congress and legislative leaders about diabetes policy change including insulin pricing.
The president is pressing for Congressional action on the Affordable Insulin Now Act, introduced in February 2022 by a group of Democrats including Sen. Michael Bennet and Sen. Raphael Warnock .
While the legislation aims to help those on Medicare plans as well as insurance plans through their employer, it does not address those using insulin who do not have insurance. That remains unaddressed, even as census and other data show that about 10 percent of people in the United States do not have health insurance.
Roughly 54.4 percent of insured Americans have employer-based plans, and more than half of those individuals are subject to high deductibles that often mean theyre forced to pay outrageous list prices for at least part of the year. This means a federal insulin copay cap particularly one that apples to people with the common ERISA-regulated health plans would have the most impact across the board, even if it doesnt achieve the #insulin4all dream of helping everyone who needs it.
Read Also: Does Metformin Cause Low Blood Sugar
Misleading Claims Cite Biden For Insulin Price Increases
CLAIM: President Joe Biden raised insulin prices after former President Donald Trump lowered them.
APS ASSESSMENT: Misleading. The president doesnt set the price of drugs. The Biden administration repealed a narrow, Trump-era regulation that sought to lower the cost of insulin at federally funded health centers. The regulation was never implemented and experts say its impact was expected to be limited.
THE FACTS: Biden called for capping the cost of insulin during his State of the Union address.
Referring to a 13-year-old with diabetes who was present for the remarks, Biden said: For Joshua, and for the 200,000 other young people with Type 1 diabetes, lets cap the cost of insulin at $35 a month so everyone can afford it.
But online, his words were met with misleading claims suggesting the president was himself responsible for the current high costs of the drug.
Republican Rep. Lauren Boebert tweeted, Joe Biden is the one who raised the price of insulin after Trump lowered it.
Biden LITERALLY CREATED THE INSULIN COST INCREASE, one conservative personality said in a tweet that garnered more than 30,000 likes.
In reality, insulin costs have been increasing for years and health policy experts say presidents dont have the power to simply set drug prices.
Boeberts office didnt respond to a request for more information on her claim, but experts say such assertions are likely referring to a narrow rule that the Biden administration repealed last year.
Big Pharma Hated Trump
Trumps most favored nation law seeks to lower prices in Medicare by linking the costs of certain medicines to cheaper prices in other developed countries. People often complain of buying the same drug in the U.S., when the price in Canada and Mexico are far cheaper. Obviously, the pharmaceutical industry strongly opposed the measure, arguing it would bring foreign price controls to the U.S. healthcare system and limit access. Groups including the Association of Community Cancer Centers and the Pharmaceutical Research and Manufacturers of America sued to block the rule. In December 2020, U.S. District Judge Catherine Blake issued a nationwide injunction on Trumps most favored nation drug pricing rule that would tie Medicare Part B drug prices to those paid in other wealthy countries starting January 1, 2021. The Trump administration also removed the gag clauses that prevented pharmacists from telling patients how to buy less expensive drugs. Apparently, pharmacists could not talk to patients about how to buy drugs.
This initiative could save the over 1.3 million seniors who rely on Medicare Part D plans and use insulin, an average of $446, or 66 percent, a year on their insulin costs. For those whose health, and even lives, depend on insulin, the savings will be nothing short of a godsend.
Read Also: Type 2 Diabetes And Dizziness
Debate On The Real Impact Of The Proposal
The executive order signed by former President Trump was meant to require federally qualified health centers who purchase insulins and epinephrine in the 340B program to pass the savings from discounted drug prices directly on to medically underserved patients.
The statement made by the US Health and Human Services about the rule said that the proposal would increase access to life-saving insulin and epinephrine for the patients who face especially high costs among the 28 million patients who visit every year.
The rule was finalized in December of last year. However, upon publishing it, the HHS itself acknowledged that the rules economic impact will most likely be minimal since the majority of patients who get their insulin from community health centers already purchase the medication on a discounted price.
The health centers involved also said the same thing. They stated that they already pass on those savings and they even called the rule an administrative burden that paints them as predators and enemies that price-gouge patients.
Revenues Also Kept Rising
Despite complaints about increasing rebates, drug makers managed to take in rising revenues from insulin even as net price declined, the report found.
Lilly, for instance, reported that the average net price for Humalog KwikPen had declined slightly from $28 per pen in 2015 to $24 per pen in 2018, even though the list price nearly doubled during the same period. Humalog revenue meanwhile increased from $1.5 billion in 2007 to $3 billion in 2018.
The committee said that internal Sanofi documents show the average Lantus net price was $87.48 in 2016 $32 lower than the net price in 2014 but still almost double the net price of $46.93 in 2005.
The companies have also spent huge sums on sales and marketing, while investing less in research and development related to insulins.
Between 2014 and 2018, Lilly spent $979 million on sales and $497 million on marketing for insulin products. Meanwhile, global R& D spending was $244 million related to Humalog, $66 million for Humulin, and $85 million for Basaglar. The company reported $22.4 billion in revenue for these therapies during the same period.
Sanofi told the committee that between 2012 and 2018 it had invested about $4.5 billion in diabetes, which includes insulin and noninsulin products. In 2014-2018, Sanofi’s diabetes franchise generated nearly $37 billion in net sales, whereas R& D spending for five insulin products was $902 million.
Also Check: Can A Diabetic Person Get A Tattoo
Rule Implementation Was Delayed
Biden’s White House chief of staff, Ronald Klain, announced a regulatory freeze of any new and pending rules as Biden took office on Jan. 20. The freeze on the insulin and epinephrine rule is effective until March 22.
According to Bloomberg Law, “A regulatory pause is a common tradition among incoming presidents to ensure that the unfinished policies from the prior administration align with the new one.”
The National Association of Community Health Centers, among others, expressed support for the new administration’s move, saying the Trump rule would not have lowered the cost of insulin and EpiPens for most Americans who use them, as advertised.
In a Jan. 25 statement, it also said the Trump rule reflected “a fundamental misunderstanding” of federally qualified health centers and the 340B drug program, placing extensive administrative burdens on them.
The stated aim was to cut drug prices. However, it triggered alarm among safety net providers and bipartisan lawmakers because it would accomplish the opposite of what the Trump Administration intended ultimately making it harder for health centers to provide affordable life-saving services and prescription drugs especially during the pandemic, the association said.
It pointed out that the only patients affected would be those using the health centers.
More:Here are all the executive orders President Joe Biden has signed so far
Insulin Makers Lit The Fusepbms Fanned The Flames

“Insulin manufacturers lit the fuse on skyrocketing prices by matching each other’s price increases step for step rather than competing to lower them, while PBMs, acting as middlemen for insurers, fanned the flames to take a bigger cut of the secret rebates and hidden fees they negotiate,” added Sen. Ron Wyden, the Committee’s highest-ranking Democrat, from Oregon.
The three US insulin makers deny working with each other or PBMs.
Eli Lilly spokesman Greg Andrew Kueterman told Medscape Medical News that the company “makes independent decisions about list price increases.”
Similarly, a Sanofi spokesman said the company “makes all of its pricing decisions independently.”
And Michael Bachner, Novo Nordisk’s director of media relations, told Medscape Medical News that the company’s “pricing decisions are made independently and are based on a number of market dynamics, some of which include our competitors’ activities, current formulary access, and discussions with payers.”
Read Also: Clinical Manifestation Of Hyperglycemia

