Favorite Resource For Diabetes Education
If insulin resistance has led you to be diagnosed with diabetes or you want to be educated if that day comes, enroll in a program led by Joslin Diabetes Center experts. The 12-week Why Wait program is designed to help you meet your weight goals, which could improve your bodys sensitivity to insulin.
What Would Happen If You Injected Too Much Insulin
If you did happen to accidentally inject too much insulin:
- your blood sugars will plummet,
- you will feel super hungry, and
- you would eat anything and everything you could get your hands on NOW to bring your blood sugars back to normal levels!
No amount of conscious willpower would stand in the way of your raging survival instincts.
And yes, if you continued to inject more insulin than you need and continue to due to the hunger it creates, you would eventually get fat. However, this fact is 100% irrelevant for the 98.5% of us that have a functioning pancreas and can produce the insulin we need.
- Endogenous and exogenous are different animals.
- Like everything in nature, your body is highly efficient your pancreas only makes just enough insulin to precisely respond to the food you eat and our body fat levels.
- Insulin alone cant magically store energy from food that you dont eat.
As you will see in this article, insulin due to the carbs you eat is not the primary driver of obesity.
Instead, the reverse is true: unless you are injecting insulin, obesity is the driver of high insulin levels.
How Is Insulin Controlled
The main actions that insulin has are to allow glucose to enter cells to be used as energy and to maintain the amount of glucose found in the bloodstream within normal levels. The release of insulin is tightly regulated in healthy people in order to balance food intake and the metabolic needs of the body. This is a complex process and other hormones found in the gut and pancreas also contribute to this blood glucose regulation. When we eat food, glucose is absorbed from our gut into the bloodstream, raising blood glucose levels. This rise in blood glucose causes insulin to be released from the pancreas so glucose can move inside the cells and be used. As glucose moves inside the cells, the amount of glucose in the bloodstream returns to normal and insulin release slows down. Proteins in food and other hormones produced by the gut in response to food also stimulate insulin release. Hormones released in times of acute stress, such as adrenaline, stop the release of insulin, leading to higher blood glucose levels to help cope with the stressful event.
Insulin works in tandem with glucagon, another hormone produced by the pancreas. While insulin’s role is to lower blood sugar levels if needed, glucagon’s role is to raise blood sugar levels if they fall too low. Using this system, the body ensures that the blood glucose levels remain within set limits, which allows the body to function properly.
Recommended Reading: Pork Rinds Good For Diabetics
The Discovery Of Insulin
In 1889 German scientists Minkowski and von Mering noted, from their experimental work with animals, that total pancreatectomy led to the development of severe diabetes. They hypothesised that a substance secreted by the pancreas was responsible for metabolic control. Others later refined this hypothesis, noting diabetes to be associated with destruction of the islets of Langerhans. While Minkowski, as well as Zuelzer in Germany and Scott in the USA attempted, with inconsistent results, to isolate and administer the missing pancreatic islet substance, Belgian investigator de Meyer in 1909 proposed the name insuline, as did British researcher Schaefer in 1916.
Mechanisms Of Insulin Resistance
Physiologically, at the whole body level, the actions of insulin are influenced by the interplay of other hormones. Insulin, though the dominant hormone driving metabolic processes in the fed state, acts in concert with growth hormone and IGF-1 growth hormone is secreted in response to insulin, among other stimuli, preventing insulin-induced hypoglycaemia. Other counter-regulatory hormones include glucagon, glucocorticoids and catecholamines. These hormones drive metabolic processes in the fasting state. Glucagon promotes glycogenolysis, gluconeogenesis and ketogenesis. The ratio of insulin to glucagons determines the degree of phosphorylation or dephosphorylation of the relevant enzymes. Catecholamines promote lipolysis and glycogenolysis glucocorticoids promote muscle catabolism, gluconeogenesis and lipolysis. Excess secretion of these hormones may contribute to insulin resistance in particular settings, but does not account for the vast majority of insulin resistant states.
Read Also: Does Metformin Lower Blood Pressure
Insulin Side Effects You May Not Have Known About
The earliest injections given to people with diabetes were comprised of insulin derived from pigs. Nothing against pigs we like bacon as much as the next person but it was a relief when other forms of synthetic insulin were developed in the 1970s, enabling us to live longer, healthier lives with fewer contributions from our porcine friends.
But as terrific as the stuff is for controlling diabetes, its not without side effects.
Whether youve been taking insulin for a short time or for a couple of decades like I have you may sometimes wonder if that rumbling in your stomach is something you ate, or if its just your insulin talking.
Here, from people in the know, are four little-known insulin side effects that you may not know about, even if youve been using insulin for years.
An Inability to Tolerate Unreasonable People. Since insulin allows glucose to get where it needs to be , it affects our blood-sugar levels rapidly. In the process, it may cause us to feel irritable, anxious and jittery, and totally unwilling to deal with the guy who cut in line at the coffee shop. Dont worry these unpleasant sensations should quickly resolve, and youll return to your normal, relaxed self. Unfortunately, crazy people will still be among us, even after your insulin-induced irritability disappears.
What Are The Complications Of Insulin Resistance
The majority of the complications that can result from insulin resistance are related to the development of vascular complications due to elevated blood sugar levels and elevated insulin levels .
Not everyone who has insulin resistance will have complications. If youve been diagnosed with insulin resistance, Type 2 diabetes or metabolic syndrome, its important to see your healthcare provider regularly and follow your treatment plan to try to prevent these complications.
You May Like: What Happens If You Miss A Dose Of Long-acting Insulin
When Should I See My Healthcare Provider About Insulin Resistance
If youve been diagnosed with insulin resistance or conditions related to insulin resistance, its important to see your healthcare provider regularly to make sure your blood sugar levels are in a healthy range and that your treatment is working.
If youre experiencing symptoms of high blood sugar or prediabetes, contact your healthcare provider. They can run simple tests to check your blood sugar levels.
If you have a family history of diabetes or conditions that can cause insulin resistance, talk to your healthcare provider about your risk of developing insulin resistance.
What Is Type 2 Diabetes
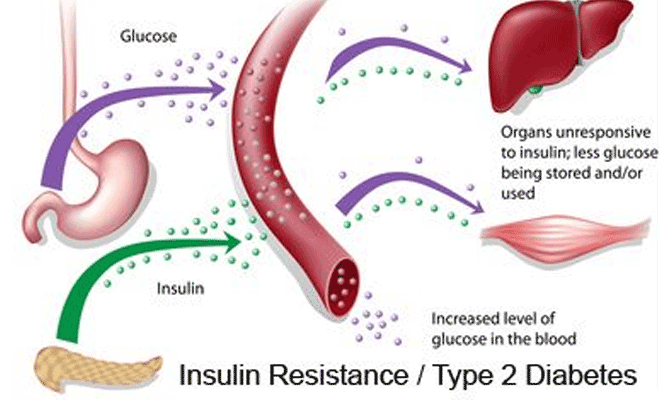
There are two major types of diabetes: type 1 and type 2. Each type causes high blood sugar levels in a different way.
In type 1 diabetes, the pancreas can’t make insulin. The body can still get glucose from food, but the glucose can’t get into the cells, where it’s needed, and glucose stays in the blood. This makes the blood sugar level very high.
With type 2 diabetes, the body still makes insulin. But a person with type 2 diabetes doesn’t respond normally to the insulin the body makes. So glucose is less able to enter the cells and do its job of supplying energy.
When glucose can’t enter the cells in this way, doctors call it insulin resistance. Although there’s plenty of insulin in the person’s body, because it doesn’t work properly, the pancreas still detects high blood sugar levels. This makes the pancreas produce even more insulin.
The pancreas may eventually wear out from working overtime to produce extra insulin. When this happens, it may no longer be able to produce enough insulin to keep blood sugar levels where they should be. In general, when someone’s blood sugar levels are repeatedly high, it’s a sign that he or she has diabetes.
p
Also Check: Side Effect To Metformin
Does Insulin Push Glucose Into Cells
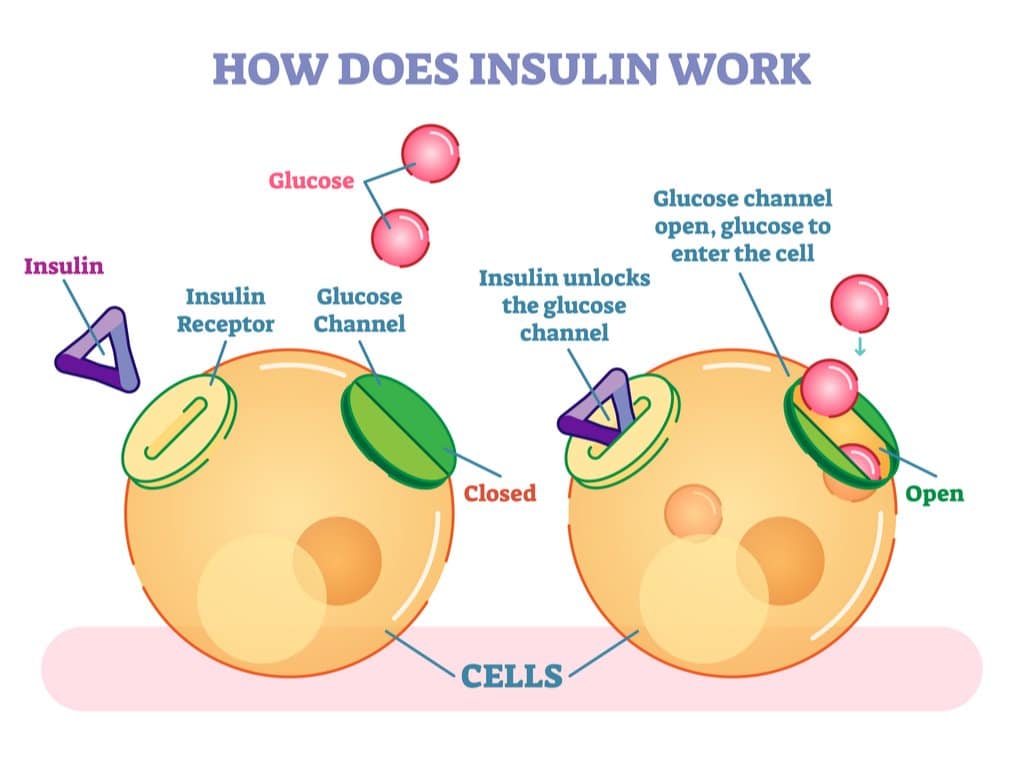
When my wife Monica was diagnosed with Type-1 Diabetes 35 years ago, she was taught that insulin is like a key that unlocks insulin receptors that work as cell doors to allow glucose into the cell. It can then be transformed and utilised as energy.
Our understanding of the role of insulin has come a long way since then. We now know that we can use energy in food via non-insulin mediated glucose uptake .
If your cells are running low on fuel, the energy from your blood basically floats into the cells to be used. Glucose is translocated across the gradient from high glucose in your blood to lower glucose in your cells. So, if your cells are using energy, they essentially suck it in from the bloodstream.
GLUT1 is the insulin-independent glucose transporter that allows cells to use glucose without insulin. A little bit of exercise goes a long way to increasing GLUT1 activity! Meanwhile, GLUT4 is the insulin-dependent glucose transporter that helps glucose enter cells.
The bottom line is that insulin isnt required to push glucose into the cells in the same manner as Japanese subway workers pushing more people onto the train. This only happens when you inject way more insulin than you need or build up an excessive amount of energy in your blood that your cells cant use.
Insulin And Type 1 Diabetes
In type 1 diabetes, the body produces insufficient insulin to regulate blood glucose levels.
Without the presence of insulin, many of the bodys cells cannot take glucose from the blood and therefore the body uses other sources of energy.
Ketones are produced by the liver as an alternative source of energy, however, high levels of the ketones can lead to a dangerous condition called ketoacidosis.
People with type 1 diabetes will need to inject insulin to compensate for their bodys lack of insulin.
Also Check: Does Metformin Make You Hungry
The Pi3k/akt Signaling Pathway
The regulatory roles of insulin in cellular function and energy metabolism are largely mediated by the PI3K/Akt pathway . Once activated by IRS, PI3K phosphorylates phosphatidylinositol 4,5-bisphosphate to produce phosphatidylinositol 3,4,5-triphosphate, which phosphorylates, and thus activates, 3-phosphoinositide dependent protein kinase-1 . PDK1 then activates Akt, which mediates multiple cellular functions. Activated Akt phosphorylates glycogen synthase kinase to deactivate it and inhibits glycogen synthase and ATP-citrate lyase activity, thereby inhibiting glycogen and fatty acid synthesis, respectively. Akt also inactivates the mammalian target of rapamycin complex 1 to promote protein synthesis. In addition, Akt mediates cell survival by inhibiting the proapoptotic pathway, and it activates sterol regulatory binding proteins , which translocate to the nucleus to transcribe genes associated with fatty acid and cholesterol synthesis. The PI3K/Akt signaling pathway also regulates the translocation of the insulin-sensitive glucose transporter GLUT4 to the membrane of muscle and fat cells for glucose uptake. GLUT4 translocation involves the IR-facilitated phosphorylation of Cbl-associated protein and production of the CAP:CBL:CRKII complex .
What Causes Insulin Resistance
Scientists still have a lot to discover about how exactly insulin resistance develops. So far, theyve identified several genes that make a person more or less likely to develop insulin resistance. In addition, older people are more prone to insulin resistance.
Several factors and conditions can cause varying degrees of insulin resistance. Scientists believe that excess body fat, especially around your belly, and physical inactivity are the two main contributing factors to insulin resistance.
Acquired causes of insulin resistance
Acquired causes, meaning youre not born with the cause, of insulin resistance include:
Hormonal disorders that can cause insulin resistance
Your body makes hundreds of hormones, which are chemicals that coordinate different functions in your body by carrying messages through your blood to your organs, muscles and other tissues. These signals tell your body what to do and when to do it.
Issues with certain hormones can affect how well your body uses insulin. Hormonal disorders that can cause insulin resistance include:
Genetic conditions that cause insulin resistance
Certain inherited genetic conditions can cause insulin resistance for various reasons.
Theres a group of rare related conditions described as inherited severe insulin resistance syndromes that are considered part of a spectrum. Listed from most mild to most severe, these syndromes include:
Other inherited conditions that cause insulin resistance include:
Also Check: How Do You Know If You Have High Blood Sugar
Rash And Allergic Reaction
Less than 4 percent of people with diabetes have a hypersensitivity or allergy to insulin, but if youre one of those 4 percent, its a significant challenge.
Its believed that a persons allergic reaction is in response to additives and peptides within commercially manufactured insulin.
The symptoms of an insulin allergy include:
- Swelling at the injection site
- Intense rash, hives, and itching
- Low blood pressure
- Swelling within your throat and mouth
- Difficulty breathing
Insulin allergies can be local or systemic, as well as immediate or delayed, explains a 2016 study. The underlying mechanisms of insulin-associated allergy can be divided into three types: type I , type III , and type IV hypersensitivity. Type I hypersensitivity, which manifests as local edema, itching, wheals, and flares, is the most common form.
To date, there is no single treatment method that has proven effective enough to be widely used.
Various treatment options, ranging from symptom relief using simple antihistaminics to more complicated insulin desensitization therapy, have been advocated for managing allergic reactions to insulin, explains the study.
While steroids can also significantly help with the allergic reaction, they create tremendous insulin resistance and make blood sugar management very difficult, so its not a realistic long-term solution.
Types Of Diabetes Tests
- Fasting blood glucose test blood glucose levels are checked after fasting for between 12 and 14 hours. You can drink water during this time, but should strictly avoid any other beverage. People with diabetes may be asked to delay their diabetes medication or insulin dose until the test is completed.
- Random blood glucose test blood glucose levels are checked at various times during the day, and it doesnt matter when you last ate. Blood glucose levels tend to stay constant in a person who doesnt have diabetes
- Oral glucose tolerance test a high-glucose drink is given. Blood samples are checked at regular intervals for two hours.
Don’t Miss: Cottage Cheese For Diabetes
Common Conditions Associated With Insulin Resistance
Type 2 Diabetes
Following pioneering work by Bornstein and the Nobel Prize-winning work of Yalow and Berson, the first insulin assays became widely available in the late 1960s it was subsequently confirmed that diabetic patients with so-called or maturity onset or type 2 diabetes had normal or increased plasma insulin levels. Insulin resistance was reported to be a characteristic feature of T2DM in the early 1970s. A progressive inability of the cells to compensate for the prevailing insulin resistance by sufficient hyperinsulinaemia, heralds the clinical onset of this disorder. While twin studies and linkage analyses are consistent with a strong genetic component in the development of type 2 diabetes, several decades of research have failed to identify a predominant genetic abnormality in the majority of cases. The aetiology of T2DM is thought to be polygenic, with environmental factors being superimposed upon this basic predisposition.
Insulin resistance typically predates the development of diabetes and is commonly found in unaffected first-degree relatives. The morbidity of the disorder relates both to the severity of hyperglycaemia and the metabolic consequences of insulin resistance itself. The primary defects in insulin action appear to be in muscle cells and adipocytes, with impaired GLUT 4 translocation resulting in impaired insulin-mediated glucose transport.
Metabolic Syndrome
-
Abdominal obesity
Men < 40 mg/dL
Women < 50 mg/dL
Dyslipidaemia
Hypertension
PCOS
OSA
Mechanisms Of Insulin Secretion
Increased levels of glucose induce the first phase of glucose-mediated insulin secretion by release of insulin from secretory granules in the cell. Glucose entry into the cell is sensed by glucokinase, which phosphorylates glucose to glucose-6-phosphate , generating ATP. Closure of K+-ATP-dependent channels results in membrane depolarization and activation of voltage dependent calcium channels leading to an increase in intracellular calcium concentration this triggers pulsatile insulin secretion. Augmentation of this response occurs by both a K+-ATP channel-independent Ca2+-dependent pathway and K+-ATP channel-independent Ca2+-independent pathways of glucose action. Other mediators of insulin release include activation of phospholipases and protein kinase C and by stimulation of adenylyl cyclase activity and activation of cell protein kinase A, which potentiates insulin secretion. This latter mechanism may be activated by hormones, such as vasoactive intestinal peptide , PACAP, GLP-1, and GIP. These factors appear to play a significant role in the second phase of glucose mediated insulin secretion, after refilling of secretory granules translocated from reserve pools.
Don’t Miss: Can A Diabetic Eat Rye Bread
Regulation And Mechanisms Of Insulin Secretion At The Cellular Level
Synthesis and secretion of insulin is regulated by both nutrient and non-nutrient secretagogues, in the context of environmental stimuli and the interplay of other hormones. Nutrient secretagogues such as glucose appear to trigger insulin secretion from the cell by increasing intracellular ATP and closing of K+-ATP channels as outlined above. Generation of cyclic AMP and other cellular energy intermediates is also augmented, further enhancing insulin release. Glucose does not require insulin action to enter the cell . Non-nutrient secretagogues may act via neural stimuli such as cholinergic and adrenergic pathways, or through peptide hormones and cationic amino acids.
Neural Stimuli
1. Cholinergic Transmission
It has been well recognised that vagus nerve stimulation results in pancreatic insulin secretion. This is thought to mediate the so-called cephalic phase of insulin secretion, occurring when food is seen, smelled or acutely ingested. Islet cell cholinergic muscarinic receptors activate phospholipase C, with subsequent intracellular events activating protein kinase C, phospholipase A2 and mobilizing intracellular calcium. Insulin secretion by these mechanisms does not occur in the fasting state or if blood glucose levels are low, but may augment the anabolic response to feeding.
2. Adrenergic Pathway
Peptide Hormones
Amino Acids
Schematic presentation of insulin secretory pathways. Adapted from references: & .
Footnotes: Figure Abbreviations
DAG = diacylglycerol

