Insulin Secretion In Response To Stimuli
Response to Glucose
In healthy individuals glucose stimulated pancreatic secretion is biphasic. Intravenous administration of glucose is associated with a rapid first phase of insulin release within 1 minute, peaking at 35 minutes, and lasting about 10 minutes the slower onset second phase of insulin secretion begins shortly after the glucose bolus but is not apparent until 10 minutes later, lasts the duration of the hyperglycaemia and is proportional to the glucose concentration immediately prior to the glucose administration. The first phase of insulin secretion represents release of insulin already synthesised and stored in secretory granules the second phase represents secretion of both stored and newly synthesised insulin. Overall insulin secretion relates to the total dose of glucose and its rate of administration maximal pancreatic response occurs with 20 g of glucose given intravenously over 3 minutes in humans.
In contrast to the reproducible pattern of insulin secretion in response to intravenous glucose, insulin secretion following oral glucose is much more variable. With an oral glucose load, gastric emptying and gastrointestinal motility affect glucose absorption, gastro-intestinal hormones and neural input associated with glucose ingestion modify the insulin response, and insulin secretion continues some time after glucose ingestion.
Response to Arginine
Effects of Lipids
Response to Mixed Meal
Incretin Hormones
Effects of Neural and Hormonal Stimuli
Vphysiology Of Insulin Secretion In Vivo
Insulin secretion in vivo has also been extensively studied. As predictable from the studies of single beta cells described above, the most important regulators of insulin secretion are circulating nutrients, in particular, glucose. In the fasting state, insulin secretion is maintained at levels that provide sufficient insulin to constrain hepatic glucose release at rates that match glucose utilization and so the plasma glucose concentration is maintained at normal levels of 90 mg/dl . After meal ingestion, glucose concentrations in the circulation rise and stimulate insulin secretion . Increased delivery of insulin into the circulation causes further suppression of hepatic glucose release and increased stimulation of glucose uptake by insulin-sensitive tissues such as muscle to restore normoglycemia. Therefore, the simplest model to describe insulin secretion in vivo would have two components: a constant basal rate of insulin secretion superimposed on which are meal-related increments. Although this model is commonly employed by physicians attempting to replace insulin in patients who secrete insufficient insulin, it is an oversimplification of a very complex dynamic neuroendocrine secretory system.
Juris J. Meier, in, 2016
Response To An Increase In Blood Glucose
In the absorptive state, an increase in blood glucose is detected by the beta cells of the pancreatic islets, causing them to increase the release of insulin into the blood. Insulin stimulates cells, especially adipose and muscle cells, to take up glucose from the blood.
Insulin and the transport of glucose into cells – To enter cells, glucose requires trans-membrane transporters and there is a family of these called GLUT . The most numerous is GLUT4, which is found on muscle and fat cells.
When insulin binds to insulin receptors on the cell membrane, cells are stimulated to increase the number of glucose transporters. The more transporters are produced, the more glucose is transported into cells – with a corresponding drop in blood glucose.
The precise mechanism whereby insulin binds to receptors causing translocation is still to be determined .
Not all tissues require insulin to take up glucose, for example brain and liver cells use GLUT transporters that are not dependent on insulin.
Further effects of insulin – The hormone also has other effects on the bodys cells, all of which contribute to an increase in glucose usage and storage – and therefore a reduction in blood glucose. These include:
– The promotion of glycolysis, a process that breaks down glucose for cellular energy
– The promotion of glycogenesis, a process that converts glucose into glycogen for storage
– The inhibition of lipolysis, a process that breaks down lipids to release energy.
You May Like: Diabetes Symptoms High Blood Sugar
Foods That Turn Into Sugar
A food’s glycemic load can also be used to measure the degree to which a particular product may affect your overall blood sugar. A low glycemic load signifies a lesser effect on glucose levels, so where there is a high glycemic load, the opposite is true.
For this reason, if you want to avoid foods that cause high blood sugar, avoid foods that possess a high glycemic load. These are the foods that turn into sugar once they are in the body.
The Harvard T.H. Chan School advises that a glycemic load of 20 and above is considered high, which includes the following foods:
- Baked potato
- White basmati rice: 1 cup cooked
- White-flour pasta: 1 1/4 cup cooked
It’s important to be aware of these levels regardless of whether you have diabetes, due to the negative effect that high-glycemic-load foods can have on the body.
A March 2013 study in the American Journal of Clinical Nutrition found that those who stuck to a diet comprised of low glycemic foods demonstrated a significantly lower risk of developing type 2 diabetes when compared to those who consumed foods with a higher glycemic load.
In addition, a similar October 2012 study in the Journal of the American Heart Association found a link between high glycemic foods and heart health. The study concluded that there was a significant link between increased high glycemic food consumption and coronary heart disease in women, but not in men.
Read more:15 Reasons to Kick Sugar
Vi Regulation Of Insulin Release
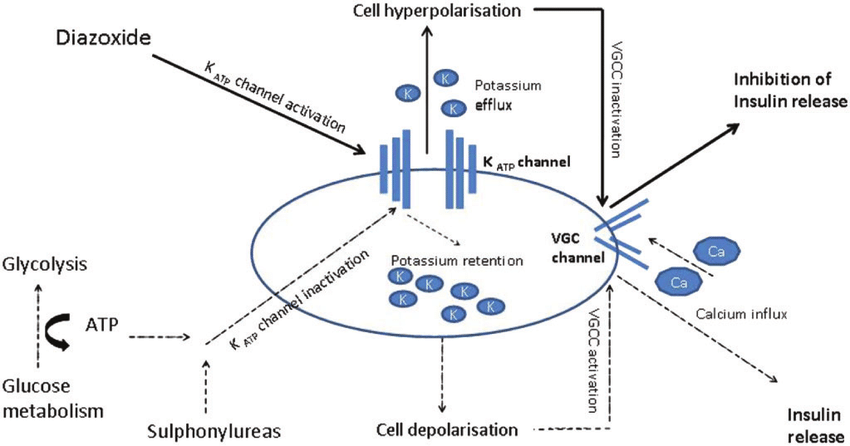
Insulin release from pancreatic b cells is tightly regulated, and allows the sensitive response of insulin levels to calorigenic nutrients in the body. Glucose, free fatty acids, and amino acids serve as fuel stimuli for insulin release, promoting insulin granule exocytosis. Additional hormonal factors influence the regulation pathway. Pharmacological agents can also be used to augment insulin release.
A. Glucose-stimulated insulin secretion
Figure 5. Hyperglycemic clamp illustration. Example of hyperglycemic clamp testing in obese adolescents with normal glucose tolerance , impaired glucose tolerance , and type 2 diabetes . In the hyperglycemic clamp in healthy, non-diabetic individuals, glucose concentration is briskly elevated by administering a suitable intravenous glucose infusion at time 0. This elicits a rapid and short-lived insulin secretion peak due to release of preformed insulin vesicles, followed by a drop towards basal levels and then by a relatively rapid return to a sustained increase in insulin in the second half of the clamp as dextrose infusion is continued. This example illustrates the loss, in first and second phase insulin secretion, as individual progress from normal to impaired glucose tolerance, to type 2 diabetes. In the latter, the first phase insulin response is essentially lost and the second phase insulin response is reduced. ).
B. Proteins and Amino Acids
C. Lipids and Free Fatty Acids
D. Incretin Hormones
Read Also: Which Stimulates The Pancreas To Secrete Glucagon
What’s It Like For Teens With Type 2 Diabetes
Sometimes people who have diabetes feel different from their friends because they need to think about how they eat and how to control their blood sugar levels every day.
Some teens with diabetes want to deny that they even have it. They might hope that if they ignore diabetes, it will just go away. They may feel angry, depressed, or helpless, or think that their parents are constantly worrying about their diabetes management.
If you’ve been diagnosed with type 2 diabetes, it’s normal to feel like your world has been turned upside down. Your diabetes care team is there to provide answers and support. Don’t hesitate to ask your doctors, dietitian, and other treatment professionals for advice and tips. It also can help to find support groups where you can talk about your feelings and find out how other teens cope.
Diabetes brings challenges, but teens who have it play sports, travel, date, go to school, and work just like their friends.
What Are Alternative Medications For People With Diabetes That Arent Insulin
- Metformin a pill that stops sugar production in the liver
- Glitazones pills that remove sugar from the bloodstream
- Sufonylureas and glinides pills that increase the release of insulin from your pancreas
- Starch blockers pills that slow starch absorption
- Incretin therapies and amvlin analogs pills and injections that reduce sugar production in the liver and slow food absorption. Types of the former include DPP4 inhibitors and GLP1 analogs .
- SGLT2 inhibitors pills that are taken before meals that prevent the reabsorption of glucose
Recommended Reading: What Happens If You Stop Taking Diabetes Medication
Neuroregulation Of Blood Glucose
The autonomic division of the nervous system modulates the release of insulin and glucagon. The sympathetic stimulation that occurs with exercise stimulates glucagon production and this maintains blood-glucose levels that would otherwise fall as muscles use glucose for their energy.
During the periods when the body is at rest, parasympathetic activity stimulates digestion and also the release of insulin to deal with the expected rise in blood glucose.
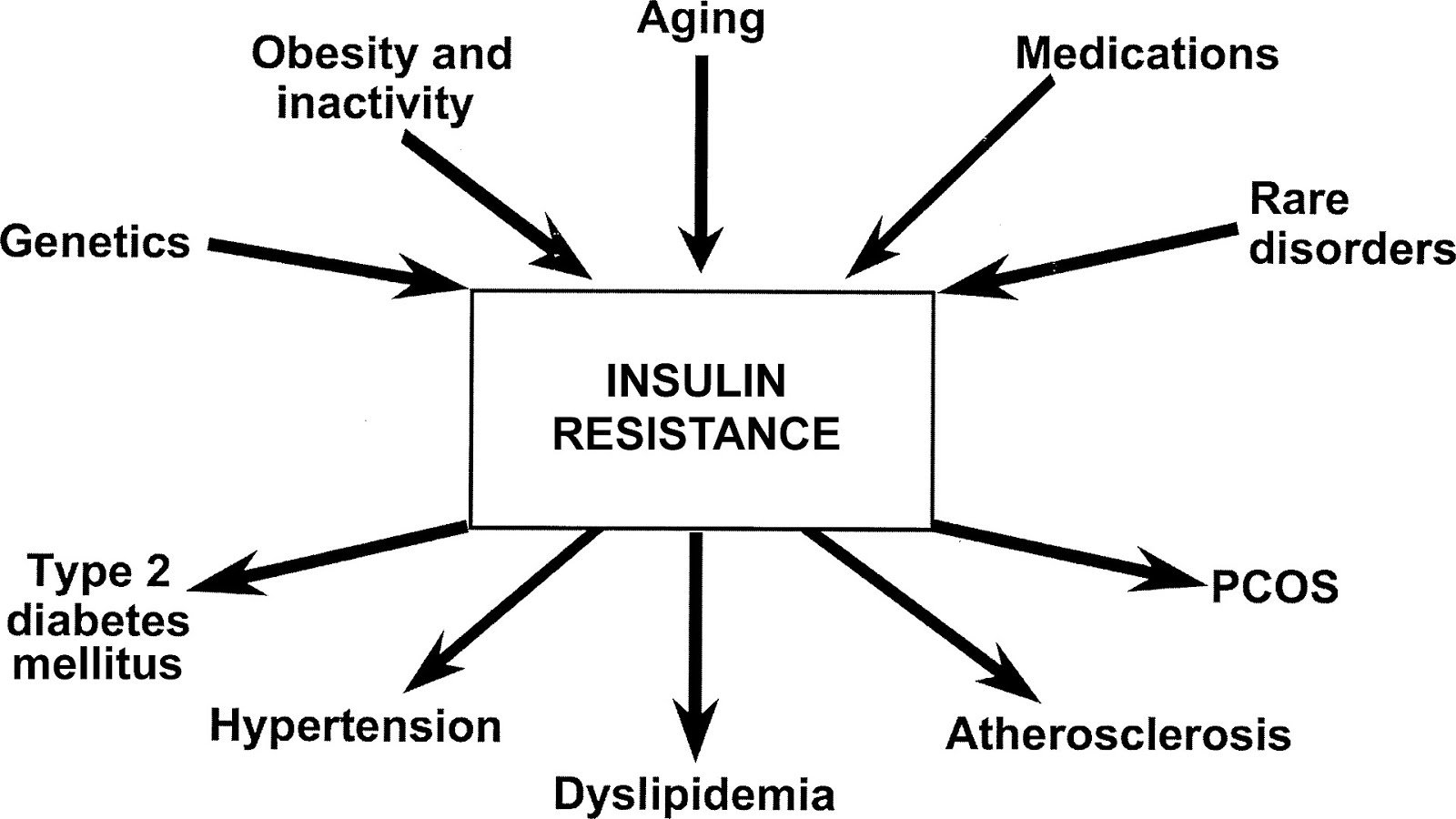
Sites Of Insulin Action And Manifestations Of Insulin Resistance
The effects of insulin, insulin deficiency and insulin resistance vary according to the physiological function of the tissues and organs concerned, and their dependence on insulin for metabolic processes. Those tissues defined as insulin dependent, based on intracellular glucose transport, are principally adipose tissue and muscle. However, insulins actions are pleotropic and widespread, as are the manifestations of insulin resistance and the associated compensatory hyperinsulinaemia.
Also Check: Insulin Metabolic Pathway
What Is Type 2 Diabetes
There are two major types of diabetes: type 1 and type 2. Each type causes high blood sugar levels in a different way.
In type 1 diabetes, the pancreas can’t make insulin. The body can still get glucose from food, but the glucose can’t get into the cells, where it’s needed, and glucose stays in the blood. This makes the blood sugar level very high.
With type 2 diabetes, the body still makes insulin. But a person with type 2 diabetes doesn’t respond normally to the insulin the body makes. So glucose is less able to enter the cells and do its job of supplying energy.
When glucose can’t enter the cells in this way, doctors call it insulin resistance. Although there’s plenty of insulin in the person’s body, because it doesn’t work properly, the pancreas still detects high blood sugar levels. This makes the pancreas produce even more insulin.
The pancreas may eventually wear out from working overtime to produce extra insulin. When this happens, it may no longer be able to produce enough insulin to keep blood sugar levels where they should be. In general, when someone’s blood sugar levels are repeatedly high, it’s a sign that he or she has diabetes.
p
The Effects Of Insulin On The Body
Insulin is a natural hormone produced by your pancreas that controls how your body uses and stores blood sugar . Its like a key that allows glucose to enter cells throughout your body.
Insulin is a vital part of metabolism. Without it, your body would cease to function.
When you eat, your pancreas releases insulin to help your body make energy out of glucose, a type of sugar found in carbohydrates. It also helps you store energy.
In type 1 diabetes, the pancreas is no longer able to produce insulin. In type 2 diabetes, the pancreas initially produces insulin, but the cells of your body are unable to make good use of the insulin. This is called insulin resistance.
Unmanaged diabetes allows glucose to build up in the blood rather than being distributed to cells or stored. This can wreak havoc with virtually every part of your body.
Blood tests can quickly indicate whether your glucose levels are too high or too low.
Complications of diabetes include kidney disease, nerve damage, heart problems, eye problems, and stomach problems.
People with type 1 diabetes need insulin therapy to live. Some people with type 2 diabetes must also take insulin therapy to control their blood sugar levels and avoid complications.
If you have diabetes, insulin therapy can do the job your pancreas cant. The following types of insulin are available:
Recommended Reading: Does Diabetes Cause Vomiting
Ask A Laboratory Scientist
This form enables patients to ask specific questions about lab tests. Your questions will be answered by a laboratory scientist as part of a voluntary service provided by one of our partners, American Society for Clinical Laboratory Science. Please allow 2-3 business days for an email response from one of the volunteers on the Consumer Information Response Team.
Incretins And The Regulation Of Insulin Secretion
Insulin secretion in response to orally administered glucose and other nutrients is 25% to 50% greater than that after their intravenous administration . This so-called incretin effect is mediated by hormones released from the gutprimarily GIP and GLP-1 . GIP is produced by K cells in the duodenum and upper jejunum, and it is released into the circulation after ingestion of nutrients. GLP-1 is synthesized in enteroglucagon or L cells, which also contain peptide YY and enteroglucagon. These L cells are primarily located in the distal small bowel, colon, and rectum. Of these two hormones, GIP is probably the major physiologic incretin. Glucose and amino acids are considered to be primary and direct stimulants of insulin secretion, but insulin secretion also is modulated by the incretins. They cause little or no insulin release in the absence of glucose or amino acids, but they can alter insulin release dramatically in response to either glucose or amino acids.
Also Check: Is Aloe Vera Good For Diabetes
Pharmacological Influences On Insulin Action And Insulin Resistance
A wide range of pharmacological agents have been associated with impaired glucose tolerance. Antihypertensive agents such as diuretics and -blockers, corticosteroids, oral contraceptives, nicotinic acid and antipsychotic agents have been reported to impair glucose tolerance, as have the anti-retroviral protease inhibitors used to treat human immunodeficiency virus infection. The mechanisms vary -blockers impair insulin secretion from the pancreas by blockade of -adrenoceptors, thiazide diuretics are thought to act by depleting potassium levels, corticosteroids and oral contraceptives have counter-regulatory hormonal activity, and the HIV-1 protease inhibitors result in partial lipodystrophy with loss of peripheral subcutaneous fat and accumulation of truncal adipose tissue leading to insulin resistance.
Physiological Role Of Insulin
Insulin is the pivotal hormone regulating cellular energy supply and macronutrient balance, directing anabolic processes of the fed state. Insulin is essential for the intra-cellular transport of glucose into insulin-dependent tissues such as muscle and adipose tissue. Signalling abundance of exogenous energy, adipose tissue fat breakdown is suppressed and its synthesis promoted. In muscle cells, glucose entry enables glycogen to be synthesised and stored, and for carbohydrates, rather than fatty acids to be utilised as the immediately available energy source for muscle contraction. Insulin therefore promotes glycogen and lipid synthesis in muscle cells, while suppressing lipolysis and gluconeogenesis from muscle amino acids. In the presence of an adequate supply of amino acids, insulin is anabolic in muscle.
Read Also: Which Pancreatic Cells Release Insulin And Glucagon
The Insulin Resistance Syndrome
The insulin resistance syndrome describes the cluster of abnormalities which occur more frequently in insulin resistant individuals. These include glucose intolerance, dyslipidaemia, endothelial dysfunction and elevated procoagulant factors, haemodynamic changes, elevated inflammatory markers, abnormal uric acid metabolism, increased ovarian testosterone secretion and sleep-disordered breathing. Clinical syndromes associated with insulin resistance include type 2 diabetes, cardiovascular disease, essential hypertension, polycystic ovary syndrome, non-alcoholic fatty liver disease, certain forms of cancer and sleep apnoea.
Regulator Of Endocannabinoid Metabolism
Insulin is a major regulator of endocannabinoid metabolism and insulin treatment has been shown to reduce intracellular ECs, the 2-arachidonoylglycerol and anandamide , which correspond with insulin-sensitive expression changes in enzymes of EC metabolism. In insulin-resistant adipocytes, patterns of insulin-induced enzyme expression is disturbed in a manner consistent with elevated EC synthesis and reduced EC degradation. Findings suggest that insulin-resistant adipocytes fail to regulate EC metabolism and decrease intracellular EC levels in response to insulin stimulation, whereby obese insulin-resistant individuals exhibit increased concentrations of ECs. This dysregulation contributes to excessive visceral fat accumulation and reduced adiponectin release from abdominal adipose tissue, and further to the onset of several cardiometabolic risk factors that are associated with obesity and type 2 diabetes.
Hypoglycemia, also known as “low blood sugar”, is when blood sugar decreases to below normal levels. This may result in a variety of symptoms including clumsiness, trouble talking, confusion, loss of consciousness, seizures or death. A feeling of hunger, sweating, shakiness and weakness may also be present. Symptoms typically come on quickly.
You May Like: Somatostatin Insulin
Produced In The Pancreas
When you eat, food travels to your stomach and small intestines, where its broken down into nutrients that include glucose. The nutrients are absorbed and distributed via your bloodstream.
The pancreas is a gland located behind your stomach that performs an essential role in the digestion process. It creates enzymes that break down the fat, starches, and sugar in the food. It also secretes insulin and other hormones into your bloodstream.
Insulin is created in the beta cells of the pancreas. Beta cells comprise about 75% of pancreatic hormone cells.
Other hormones produced by the pancreas are:
- glucagon, which alerts your liver to raise your blood sugar if it gets too low
- gastrin, which stimulates the production of gastric acid in your stomach
- amylin, which helps control your appetite
V Insulin Secretory Pathway
The pancreatic b-cells act as a self-contained system to secrete insulin in response to changes in ambient blood glucose concentration, in order to maintain glucose homeostasis. Glucose is freely taken up into the b-cell via GLUT transporters, metabolized to produce ATP, which triggers a cascade of signals within the b cell necessary for glucose-induced insulin secretion. While GLUT2 has been traditionally assumed as the major mediator of glucose uptake into b-cells based on extrapolation from rodent studies and subsequent confirmation of GLUT2 transporters on human -cells , more recent studies in human islets suggest that the other insulin-independent glucose transporters GLUT1 and GLUT3 play a more important role, and are the main glucose transporters in human islet -cells . This redundancy explains why individuals with variants in the gene encoding GLUT2 do not have significant abnormalities in insulin secretion .
Figure 4. Diagrammatic illustration of insulin secretion. A low background secretion exists upon which is superimposed insulin secretory bursts stimulated by food intake. ).
Also Check: How Long Do You Live With Diabetes

